{}
Summary
General Perioperative Approach
1. Defer Elective Surgery
- Indication: Acutely intoxicated patients.
- Rationale: Reduces drug interactions, haemodynamic instability, and withdrawal risks.
2. Management of Recovering Addicts
- Considerations:
- Different protocols for patients on Methadone vs. Buprenorphine.
- Opiate antagonists can precipitate withdrawal.
- Use multimodal analgesia (MMA) or adequately dose opiates if used.
- Actions:
- Involve the multidisciplinary team (MDT) and pain team.
- Discuss with the patient the risk of relapse if opiates are used.
3. Hyperalgesia Management
- Medication: Ketamine.
- Dosage: 0.06 – 0.12 mg/kg/hr.
4. Catecholamine Management
- Issue: Potential depletion of catecholamine stores.
- Approach:
- Use direct-acting agents only (Avoid ephedrine).
- Avoid β-blockers to prevent unopposed α-stimulation.
- Dexmedetomidine can be used.
5. Management of Withdrawal/Delirium Tremens (DTs)
- Supportive Management:
- Sedation
- Fluids
- Electrolyte balance
- Glucose control
6. Pulmonary Considerations
- Potential Complications:
- Pulmonary toxicity
- Pulmonary hypertension (PHT)
- Cause: Chronic inhalation or sympathomimetic use.
7. Analgesic Options
- Strategies:
- Full multimodal analgesia (MMA)
- Infusions
- Regional anesthesia
- Neuraxial anesthesia
Alcoholism
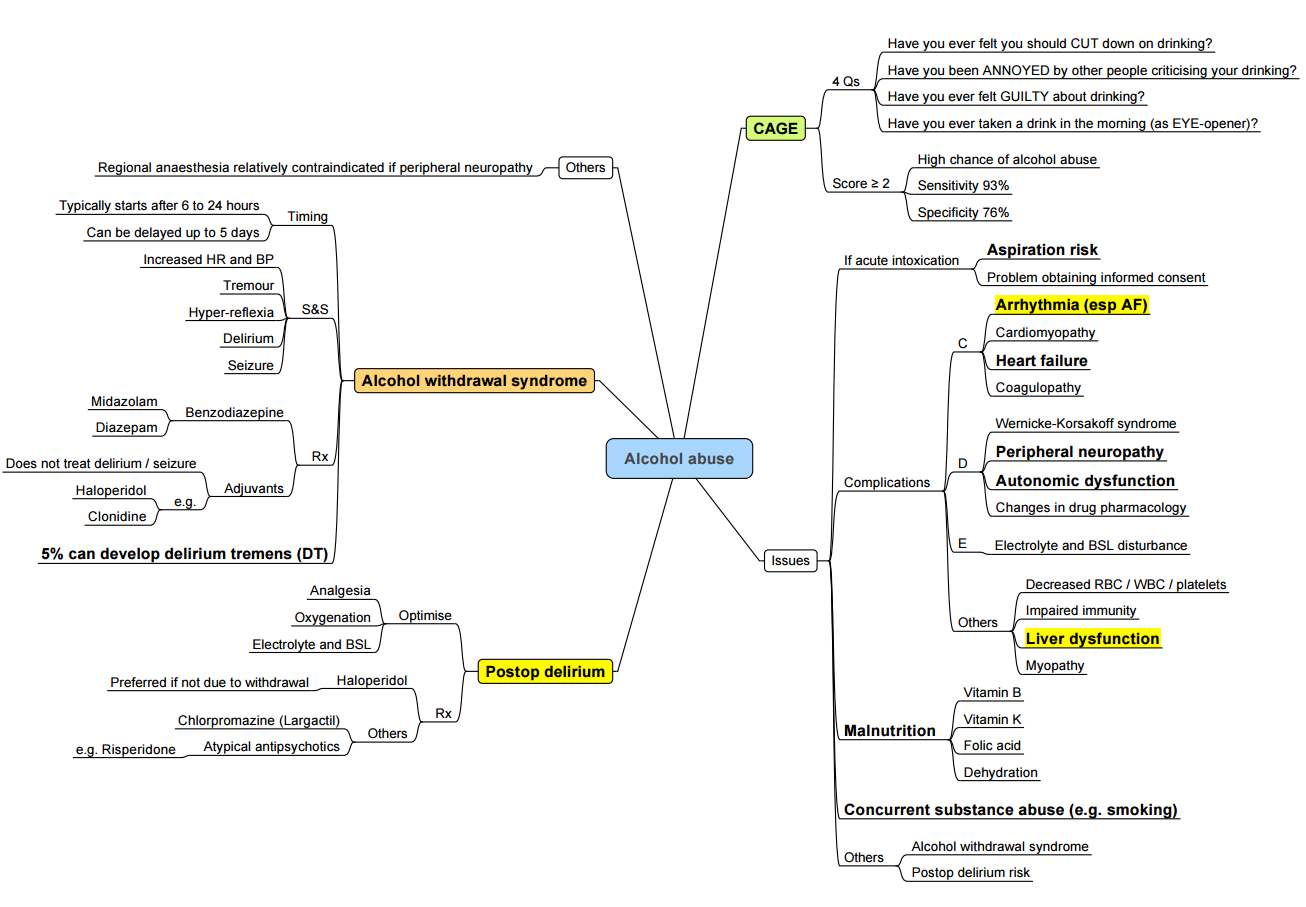
Considerations
Anaesthesia for Chronic Alcohol (ETOH) Users
Consent
- Assess for intoxication status.
Premedication
- Benzodiazepines: Prophylactic use to prevent withdrawal symptoms.
Coagulation
- Tests: Check INR and evaluate for thrombocytopenia.
Electrolytes
- Actions: Check and correct any imbalances.
Blood Sugar
- Risk: Chronic alcohol users are prone to hypoglycemia.
Aspiration Risk
- Increased risk due to potential delayed gastric emptying.
Drugs
- Withdrawal Protocol: Ensure adherence to a withdrawal management protocol.
- Pharmacodynamics/Pharmacokinetics (PD/PK):
- Chronic abusers may require increased doses of propofol, thiopentone, and opioids due to possible enzyme induction.
- Dose requirements decrease during acute intoxication.
- Hepatic impairment leads to reduced drug clearance.
- Hypoalbuminaemia can affect drug binding and efficacy.
Regional/Blocks
- Documentation: Record any existing peripheral neuropathy.
- Consideration: Evaluate coagulation status before proceeding.
Haemodynamics
- Consideration: Be aware of the potential for underlying cardiomyopathy.
Complications
- Withdrawal: Monitor and manage withdrawal symptoms.
- Postoperative Risks:
- Increased risk (2-5 times) of complications such as acute coronary syndrome, arrhythmias, prolonged ICU stays, and increased risk of delirium.
Multisystem Disease
Central Nervous System (CNS)
- Conditions: Peripheral neuropathy, Wernicke-Korsakoff syndrome (ocular abnormalities, ataxia, confusion), cerebral atrophy/dementia.
Cardiovascular System
- Conditions: Cardiomyopathy, palpitations, arrhythmias.
Gastrointestinal System
- Conditions: Liver dysfunction/cirrhosis, esophagitis, gastritis, pancreatitis, malnutrition.
Haematology
- Conditions: Pancytopenia.
Endocrine/Metabolic System
- Conditions: Hypoglycemia, hypoalbuminemia, electrolyte abnormalities (hypokalemia, hypomagnesemia).
Musculoskeletal System
- Conditions: Myopathies, osteoporosis.
Other Considerations
- Addictions: Monitor for other substance dependencies.
- Alcohol Withdrawal Syndromes: Implement CIWA protocol for management (tremors, autonomic hyperactivity, delirium tremens).
Altered Pharmacology
- Liver Enzyme Induction: May increase the minimum alveolar concentration (MAC) of anesthetics.
Alcohol Withdrawal & Syndromes
Earliest & Most Common Symptoms
- General Symptoms: Generalized tremors, perceptual disturbances (nightmares, hallucinations), autonomic hyperactivity (tachycardia, hypertension, cardiac dysrhythmias), nausea, vomiting, insomnia, mild confusion, and agitation.
- Onset: Symptoms usually begin within 6 to 8 hours after a substantial decrease in blood alcohol concentration and peak at 24 to 36 hours.
- Management: Symptoms can be suppressed by resumption of alcohol ingestion or administration of benzodiazepines.
Delirium Tremens
- Incidence: Occurs in approximately 5% of those experiencing withdrawal.
- Symptoms: Hallucinations, combativeness, hyperthermia, tachycardia, hypertension or hypotension, grand mal seizures.
- Onset: Symptoms begin 2 to 4 days after alcohol cessation.
- Treatment:
- First Line: Benzodiazepines titrated to effect without loss of respiration.
- Additional Treatments: Beta blockers to reduce tachycardia and hypertension, correction of metabolic abnormalities (potassium, magnesium, thiamine).
- Severe Cases: ICU admission, propofol infusion/dexmedetomidine, and possible intubation.
- Mortality Rate: Approximately 10%, usually due to hypotension, dysrhythmias, or seizures.
Wernicke-Korsakoff Syndrome
Wernicke’s Encephalopathy
- Pathology: Loss of neurons in the cerebellum.
- Nature: Acute syndrome requiring emergent treatment to prevent death and neurologic morbidity.
Korsakoff’s Psychosis
- Nature: Chronic neurologic condition.
- Cause: Loss of memory resulting from the lack of thiamine (vitamin B1), which is required for the intermediary metabolism of carbohydrates.
Links
Past Exam Questions
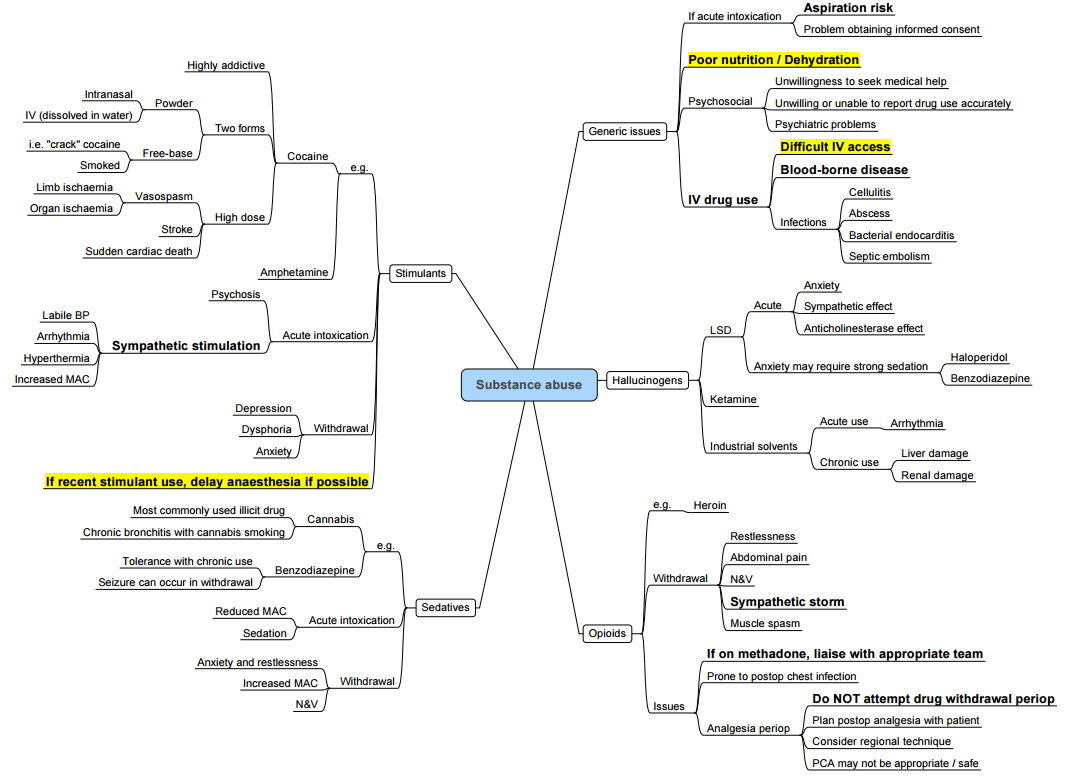
Substance Abuse and Emergency Anaesthesia
A patient presents on the emergency list with a stab wound to the abdomen for an exploratory laparotomy. His brother mentions that he is known to be a substance abuser, but he does not know any further details.
How does this history of substance abuse impact your anaesthetic plan? (10)
References:
- The Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- ICU One Pager. (2024). Retrieved June 5, 2024, from https://onepagericu.com/
Summaries:
Alcohol withdraw
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “62b17f32-aef8-4717-9e34-73c0ae97b409”



