- Renal Disease
- Laboratory Investigations
- Preoperative Considerations
- Complications Specific to Anaesthesiologists
- General Rules
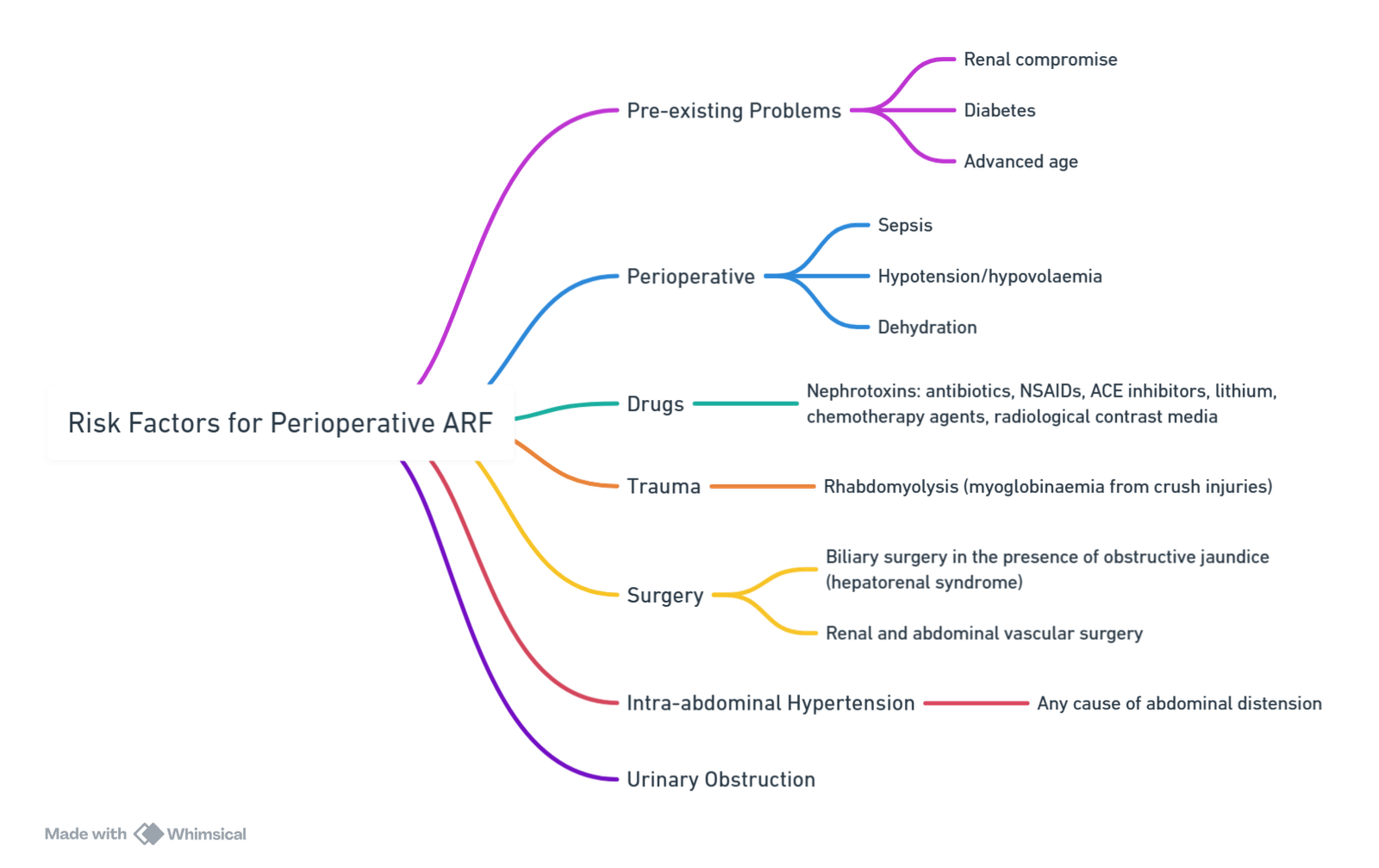
- Risk Factors for Developing AKI Perioperatively
- Indirect Anaesthesia Effects
- Drugs and Toxins Associated with Acute Kidney Injury
- Blood Workup
- Preoperative Therapy Recommendations
- Recommendations for Nephroprotective Measures
- Aetiologies of Perioperative Acute Kidney Injury
- Anaesthesia Drugs and CKD
- Management of AKI
{}
Renal Disease
Preoperative renal dysfunction is an independent risk factor for postoperative morbidity and mortality. Creatinine is a product of skeletal muscle metabolism and undergoes little renal tubular secretion, so creatinine clearance reflects the glomerular filtration rate (GFR). The normal GFR is 125 mL/min.
Rules of Thumb
- GFR must be reduced by 50% before serum creatinine starts to rise.
- Small changes in serum creatinine in the low (normal) range imply a large change in GFR, making the test very sensitive.
- GFR falls by 1% per annum after 30 years of age.
- Low muscle mass (e.g., small elderly lady) means little creatinine to clear, so normal plasma creatinine may not indicate normal renal function.
Serum creatinine levels greater than 200 µmol/L are an independent risk factor for cardiac complications and mortality.
Laboratory Investigations
Summary
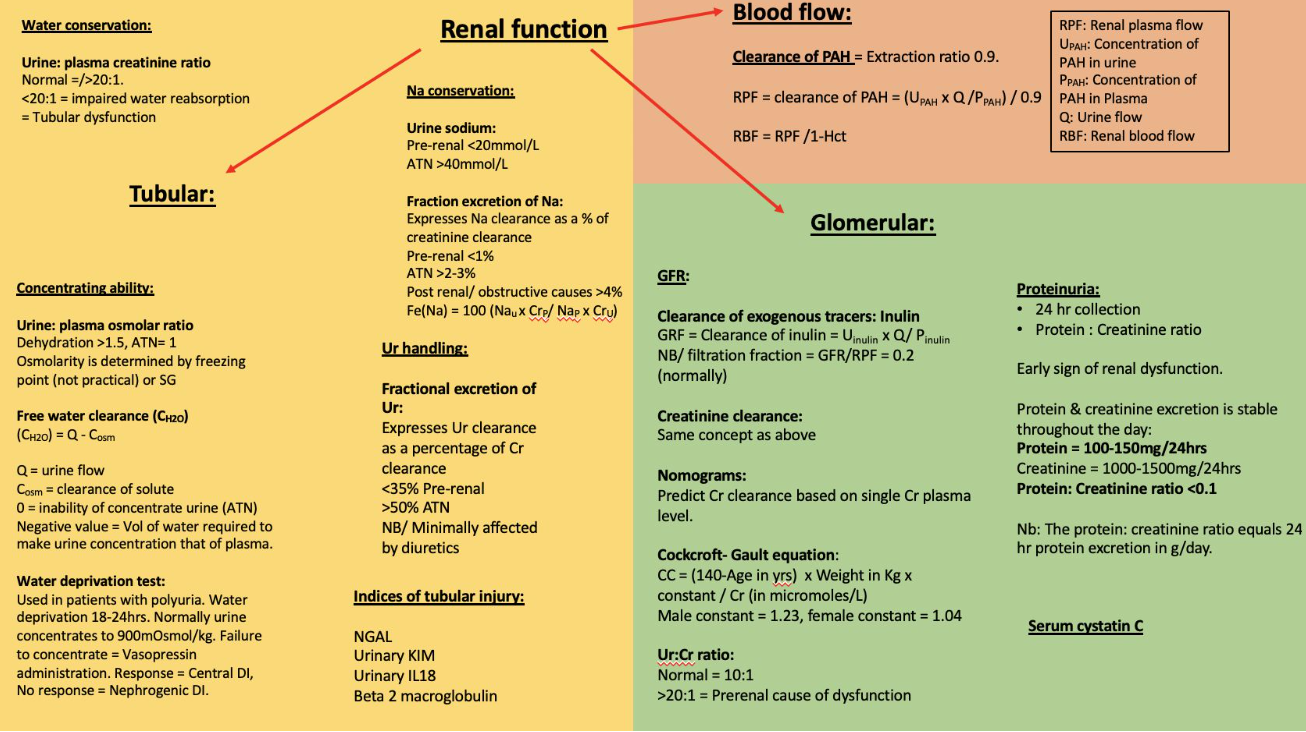
Renal Function Parameters
| Parameter | Normal Values |
|---|---|
| Renal blood flow | 1200 ml/min |
| Renal plasma flow | 650 ml/min |
| Haematocrit | 40% |
| Filtration fraction | 20% |
| Glomerular filtration rate | 125 ml/min |
| Urine flow rate | 1 ml/min |
| Urinary protein | < 150 mg/day |
| Urinary creatinine | 1000 – 1500 mg/day (88,000 – 132,000 µmol/day) |
| Urine protein: creatinine ratio | < 0.1 |
| Serum urea: creatinine ratio | 10: 1 |
| Serum urea | 2.5 – 6.7 mmol/l |
| Serum creatinine | 70 – 130 µmol/l |
| Creatinine clearance | 80 – 140 ml/min |
| Urine osmolality | 500 – 800 mOsm/kg |
| Serum osmolality | 282 – 295 mOsm/kg |
| Urine specific gravity | 1.002 – 1.028 |
| Urine: plasma osmolar ratio | ~ 1.3: 1 |
| Free water clearance | -8 to +18 litres/day |
| Urine: plasma creatinine ratio | > 20: 1 |
| Fractional excretion of sodium | 1 – 2% |
| Fractional excretion of urea | 35 – 50 |
| Conversion of mg/dl creatinine to µmol/l | x 88 |
Diagnostic Tests in Renal Function
| Diagnostic Test | Strengths | Weaknesses |
|---|---|---|
| Serum creatinine | Easily available Low cost |
Not renal specific Late marker after renal injury Confounded by muscle mass, drugs, technique, fluid status |
| Blood urea nitrogen (BUN) | Easily available Low cost |
Not renal specific Confounded by liver disease, gastrointestinal bleed, hypovolemia |
| FeNa (Fractional excretion of sodium) | Easily available Low cost |
Difficult to interpret in chronic kidney disease Confounded by diuretic treatment |
| Urine microscopy | Noninvasive Low cost Provides valuable information if done properly (e.g., red cell casts in glomerulonephritis) |
Operator dependent Requires training and experience |
| Renal histology | Provides valuable information about cause of AKI and degree of chronic changes | Invasive Requires competency Bleeding complications |
| Novel AKI biomarkers | Diagnose AKI before creatinine rise Additional diagnostic and prognostic information |
Costs Significant confounders |
| Techniques to measure real-time GFR | Monitor GFR in real-time Early diagnosis of AKI |
Costs Not yet available in clinical practice Requires training and experience |
Tests for Aetiology
| Laboratory Test | Pre-renal | Acute Tubular Necrosis | Function of Test |
|---|---|---|---|
| Urine osmolality (mOsm/kg) | > 500 | ~ 300 | Urine concentrating ability |
| U/P osmolality ratio | > 1.5 | < 1.1 – 1.2 | Urine concentrating ability |
| Urine specific gravity | > 1.020 | 1.010 | Urine concentrating ability |
| Urine sodium (mEq/l) | < 10 – 20 | > 40 | Sodium conservation |
| FeNa (%) | < 1 | > 2 | Sodium conservation |
| Urine: Plasma creatinine ratio | > 40 | < 20 | Water conservation |
| FEU (%) | < 35 | > 50 | Urea handling |
| Serum Urea: Creatinine ratio | > 20 | < 10-15 | Urea handling |
| Urinary sediment | Normal, occasional hyaline or finely granular casts | Renal tubular epithelial cells, coarse, granular and muddy brown casts | Urine analysis |
Blood Urea Nitrogen (BUN)
- Protein catabolism: Ammonia is produced from the deamination of amino acids.
- Hepatic conversion: Conversion of ammonia to urea by the liver prevents the build-up of toxic ammonia levels.
- Relationship to protein catabolism and filtration: BUN levels are directly related to protein catabolism and inversely related to glomerular filtration.
- Indicator of GFR: BUN is not a reliable indicator of GFR unless protein catabolism is normal and constant. Normally, 40% to 50% of the urea filtrate is passively reabsorbed by the renal tubules. Hypovolemia increases this reabsorption fraction.
Creatinine
- Daily production: Men produce 20 to 25 mg/kg of creatinine daily; women produce 15 to 20 mg/kg.
- Renal handling: Creatinine is filtered and minimally secreted, but not reabsorbed in the kidneys. Serum creatinine concentration is directly related to body muscle mass and inversely related to glomerular filtration.
- Limitations in critical illness: A single serum creatinine measurement may not accurately reflect GFR in critically ill patients due to abnormal creatinine production and volume distribution.
- Postoperative increases: Even small postoperative increases in serum creatinine are associated with increased morbidity and mortality.
- GFR and serum creatinine: Doubling of serum creatinine indicates a 50% reduction in GFR.
- Age-related changes: GFR declines by 5% per decade after age 20, but because muscle mass also declines, serum creatinine levels remain relatively normal. Creatinine production may decrease to 10 mg/kg.
- Older adults: Small increases in serum creatinine may indicate significant changes in GFR. The Cockcroft-Gault formula is recommended for accurate measurement.
- Equilibration time: Serum creatinine requires 48 to 72 hours to equilibrate at a new level following acute changes in GFR.
Cockcroft–Gault Formula
Creatinine clearance (mL/min)
(140 − age in years) × (weight in Kg) × 1.23 if male (1.04 if female) / SCr in μ mol / L .
80 to 140 ml/min
Factors Affecting Creatinine Levels
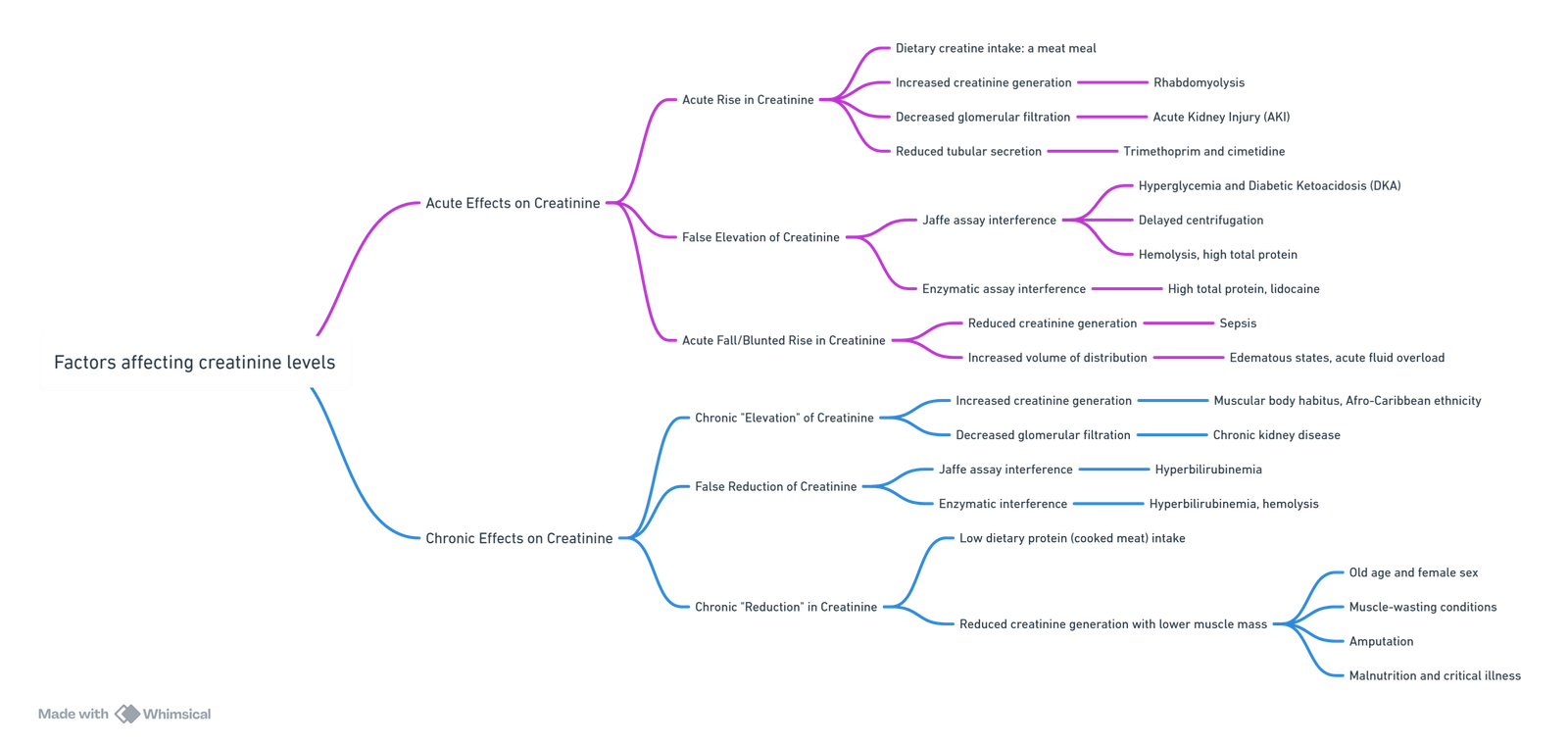
View or edit this diagram in Whimsical.
Creatinine Clearance
Clearance
- Definition: The renal clearance of a substance is defined as the volume of blood that is completely cleared of that substance per unit of time.
- Assessment of GFR: It is the most accurate method available for clinically assessing GFR. The test usually takes 24 hours, though a 2-hour creatinine clearance test is also accurate.
- Levels of creatinine clearance:
- Mild: 40 to 60 mL/min.
- Moderate: 25 to 40 mL/min, always causes symptoms.
- Overt kidney failure: Less than 25 mL/min.
- Effect of later-stage kidney disease: In later-stage kidney disease, increased creatinine secretion in the proximal tubule leads to creatinine clearance progressively overestimating the true GFR as kidney function declines.
GFR Measurement
Clearance of Exogenous Tracers
- Inulin:
- Inulin is filtered but not secreted or reabsorbed, making it the gold standard for GFR measurement.
- Procedure: Administer a bolus and infusion, then wait for equilibration prior to sample taking.
- Calculation: GFR = Clearance of inulin = Uinulin×Q/Pinulin
- Filtration fraction = GFR/RPF = 0.2 (normally).
Creatinine Clearance
- Concept: Same as above.
- Endogenous: Creatinine is endogenous, but a small amount is secreted and reabsorbed, making it not completely accurate.
- Clinical stability: It is also inaccurate in a clinically unstable environment or if creatinine levels are very low.
Nomograms
- Purpose: Predict creatinine clearance based on a single creatinine plasma level.
- Cockcroft-Gault Equation:
- (140 − age in years) × (weight in Kg) × 1.23 if male (1.04 if female) / SCr in μ mol / L .
Urine to Creatinine Ratio
- Normal: 10:1.
- Prerenal cause: More than 20:1 indicates a prerenal cause of dysfunction.
AKI
Definition
- AKI: A syndrome characterized by a rapid (hours to days) deterioration of kidney function.
- Duration: AKI is defined as occurring over 7 days, whereas chronic kidney disease (CKD) starts when kidney disease persists for more than 90 days.
- Incidence: AKI is a common and underappreciated perioperative problem, occurring in 1% to 5% of all hospitalized patients and in approximately 50% of all ICU patients.
Acute Kidney Injury (AKI) Classification Criteria
| Criteria | RIFLE Classification | AKIN Classification | KDIGO Classification | Urine Output Criteria of All Classifications |
|---|---|---|---|---|
| Definition of AKI | Increase in serum creatinine of either ≥0.3 mg/dL (≥26.4 µmol/L) or a percentage increase of ≥50% (1.5-fold from baseline) in 48 h | Rise in serum creatinine by ≥26 µmol/L over ≤48 h, or to ≥1.5-fold from baseline that is known or presumed to have occurred in the preceding 7 days | <0.5 mL/kg/h for >6 h | |
| Stage I or RIFLE Risk | Increase in serum creatinine to ≥1.5 to 2-fold from baseline, or GFR decrease by >25% | Increase in serum creatinine by ≥26 µmol/L (≥0.3 mg/dL) or increase to more than or equal to 1.5-fold to 2-fold from baseline | Rise in serum creatinine by ≥26.5 µmol/L in 48 h, or rise to 1.5–1.9 times from baseline | <0.5 mL/kg/h for >6 h |
| Stage II or RIFLE Injury | Increase in serum creatinine to ≥2-fold to 3-fold from baseline, or GFR decrease by >50% | Increase in serum creatinine to more than 2-fold to 3-fold from baseline | Rise in serum creatinine 2.0–2.9 times from baseline | <0.5 mL/kg/h for >12 h |
| Stage III or RIFLE Failure | Increase in serum creatinine to >3-fold from baseline, or to ≥354 µmol/L with an acute rise of at least 44 µmol/L, or GFR decrease by >75% | Increase in serum creatinine to more than 3-fold from baseline, or to ≥354 µmol/L with an acute rise of at least 44 µmol/L, or treatment with RRT irrespective of the stage at the time of RRT | Rise in serum creatinine three times from baseline, or increase in serum creatinine to ≥353.6 µmol/L, or initiation of RRT irrespective of serum creatinine | <0.3 mL/kg/h for 24 h or more, or anuria for 12 h |
| RIFLE Loss | Complete loss of kidney function for >4 wk | |||
| End-stage kidney disease | End-stage kidney disease for >3 mo |
Limitations of KDIGO Criteria
- Lack of GFR Reliance: KDIGO criteria do not rely on changes in GFR for staging, except in children under the age of 18 years.
- Misclassification Risk:
- AKI misclassification may result from the lack of a uniform approach to estimate baseline serum creatinine (SCr).
- Changes in SCr concentrations can result from acute severe illness and altered fluid balance.
- Urine Output Data: Exact data on urine output are not always available, leading to underutilization of the urine output criteria.
- Serum Creatinine Influences: Serum creatinine is affected by several factors other than renal function, which can affect its reliability as a marker.
Potential Pitfalls of AKI Diagnosis Based on Creatinine and Urine Criteria
| Clinical Scenario | Consequence |
|---|---|
| Administration of drugs which interfere with tubular secretion of creatinine (e.g., cimetidine, trimethoprim) | Misdiagnosis of AKI (rise in serum creatinine without change in renal function) |
| Reduced production of creatinine (e.g., muscle wasting, liver disease, sepsis) | Delayed or missed diagnosis of AKI |
| Ingestion of substances which lead to increased generation of creatinine (e.g., creatine, cooked meat) | Misdiagnosis of AKI |
| Obesity | Overdiagnosis of AKI if using actual weight when applying urine output criteria |
| Conditions associated with physiologically increased GFR (e.g., pregnancy) | Delayed diagnosis of AKI |
| Interference with analytical measurement of creatinine (e.g., 5-fluorocytosine, cefoxitin, bilirubin) | Misdiagnosis and delayed diagnosis of AKI (depending on the substance) |
| Fluid resuscitation and overload | Delayed diagnosis of AKI (dilution of serum creatinine concentration) |
| Progressive CKD with gradual rise in serum creatinine | Misdiagnosis of AKI |
| Extrinsic creatinine administration as a buffer in medications (e.g., in dexamethasone, azaseron) | Pseudo-AKI |
| Oliguria due to acute temporary release of ADH (e.g., post-operatively, nausea, pain) | Misdiagnosis of AKI (enhanced by maximal sodium reabsorption in the setting of volume/salt depletion) |
Diagnostic Workup for Acute Kidney Injury (AKI)
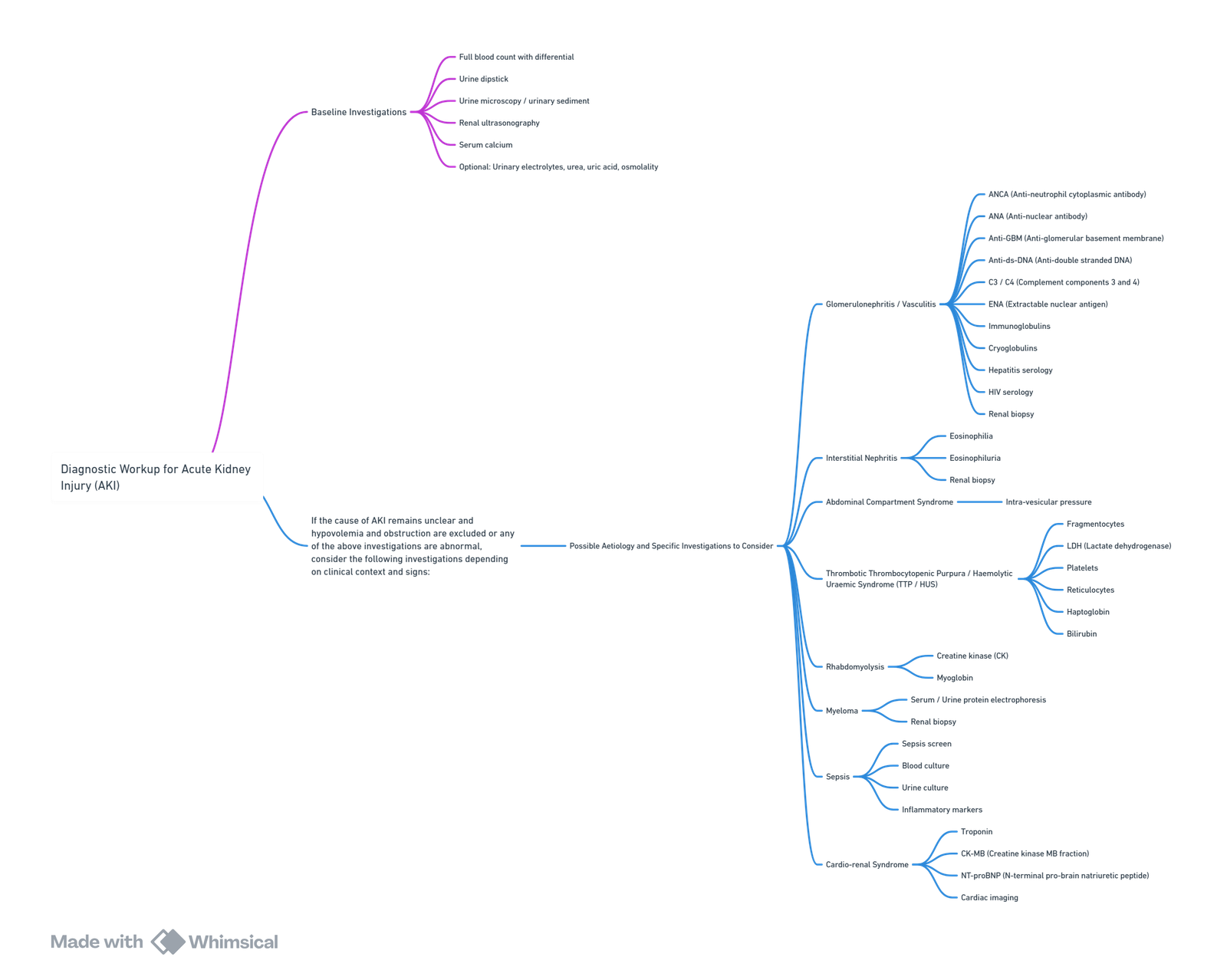
View or edit this diagram in Whimsical.
AKI Risk Index for Patients Undergoing Surgery
Risk Factors
- Age: ≥ 56 years
- Sex: Male
- Active Congestive Heart Failure
- Ascites
- Hypertension
- Emergency Surgery
- Intraperitoneal Surgery
- Renal Insufficiency: Mild or moderate (Preoperative serum creatinine > 1.2 mg/dL)
- Diabetes Mellitus: Oral or insulin therapy
Risk Classification
- Class I: 0–2 risk factors
- Class II: 3 risk factors
- Class III: 4 risk factors
- Class IV: 5 risk factors
- Class V: ≥ 6 risk factors
View or edit this diagram in Whimsical.
Chronic Kidney Disease (CKD)
KDIGO 2012: CKD Classification by GFR and Albuminuria
Persistent Albuminuria Categories
- A1: Normal to mildly increased (<30 mg/g, <3 mg/mmol)
- A2: Moderately increased (30-300 mg/g, 3-30 mg/mmol)
- A3: Severely increased (>300 mg/g, >30 mg/mmol)
GFR Categories (ml/min/1.73 m²)
- G1: Normal or high (≥90)
- G2: Mildly decreased (60-89)
- G3a: Mildly to moderately decreased (45-59)
- G3b: Moderately to severely decreased (30-44)
- G4: Severely decreased (15-29)
- G5: Kidney failure (<15)
Most Common Causes
- Diabetes mellitus 30%
- Hypertension 24%
- Glomerulonephritis 17%
- Chronic pyelonephritis 5%
- Polycystic renal disease 4%
- Unknown cause 20%
Staging
- Stage 1, normal GFR—other evidence of renal damage.
- Stage 2, GFR 60–90mL/min—other evidence of renal damage.
- Stage 3, GFR 30–60mL/min—moderate CRF.
- Stage 4, GFR 15–30mL/min—severe CRF.
- Stage 5, GFR <15mL/min—end-stage renal failure
Manifestations of Chronic Kidney Disease (CKD)
Neurological
- Peripheral neuropathy
- Autonomic neuropathy
- Muscle twitching
- Encephalopathy
- Asterixis
- Myoclonus
- Lethargy
- Confusion
- Seizures
- Coma
Cardiovascular
- Fluid overload
- Congestive heart failure
- Diastolic dysfunction
- Hypertension
- Pericarditis
- Arrhythmia
- Conduction blocks
- Vascular calcification
- Accelerated atherosclerosis
Pulmonary
- Hyperventilation
- Interstitial and alveolar edema
- Pleural effusion
Gastrointestinal
- Anorexia
- Nausea and vomiting
- Delayed gastric emptying
- Hyperacidity
- Mucosal ulcerations and hemorrhage
- Adynamic ileus
Metabolic
- Metabolic acidosis
- Hyperkalemia
- Hyponatremia
- Hypermagnesemia
- Hyperphosphatemia
- Hypocalcemia
- Hyperuricemia
- Hypoalbuminemia
Hematological
- Anemia
- Platelet dysfunction
- Leukocyte dysfunction
Endocrine
- Glucose intolerance
- Secondary hyperparathyroidism
- Hypertriglyceridemia
Skeletal
- Osteodystrophy
- Periarticular calcification
Skin
- Hyperpigmentation
- Ecchymosis
- Pruritus
Pharmacological Considerations in CKD
- Drug Accumulation:
- Drugs reliant on renal excretion will accumulate in renal failure.
- Volume of Distribution (Vd):
- If Vd is unchanged, loading doses remain the same, but subsequent doses and intervals must be adjusted.
- Fluid retention can increase Vd, requiring higher doses.
- Dose Modifications:
- Dosing adjustments calculated using:
- Current CrCl / Normal CrCl × Normal Dose
- Dosing adjustments calculated using:
Specific Drugs
- Volatiles:
- Sevoflurane is safe despite potential compound A production.
- Opioids:
- Morphine’s active metabolite is renally excreted, leading to prolonged effects.
- Fentanyl: 7% is renally excreted unchanged.
- Alfentanil: Increased free fraction necessitates dose reduction.
- NSAIDs:
- Nephrotoxic. Aspirin is safe in renal patients.
- Neuromuscular Blockers:
- Succinylcholine is not contraindicated but consider potassium levels; effects may be prolonged.
- Atracurium and cisatracurium are preferred.
Pharmacokinetics/Pharmacodynamics (PK/PD) In CKD
Absorption
- Gastroparesis, delayed gastric emptying, and gut edema.
- Raised gastric pH.
- Time since dialysis can affect drug absorption.
Distribution
- Albumin is reduced; organic acids compete for binding sites.
- Alpha-1 acid glycoprotein is increased.
Elimination
- Renal Clearance:
- Significantly reduced.
- Hepatic Clearance:
- Potentially affected due to altered gene transcription or depletion of cofactors.
Renal and Anaesthesia Implications
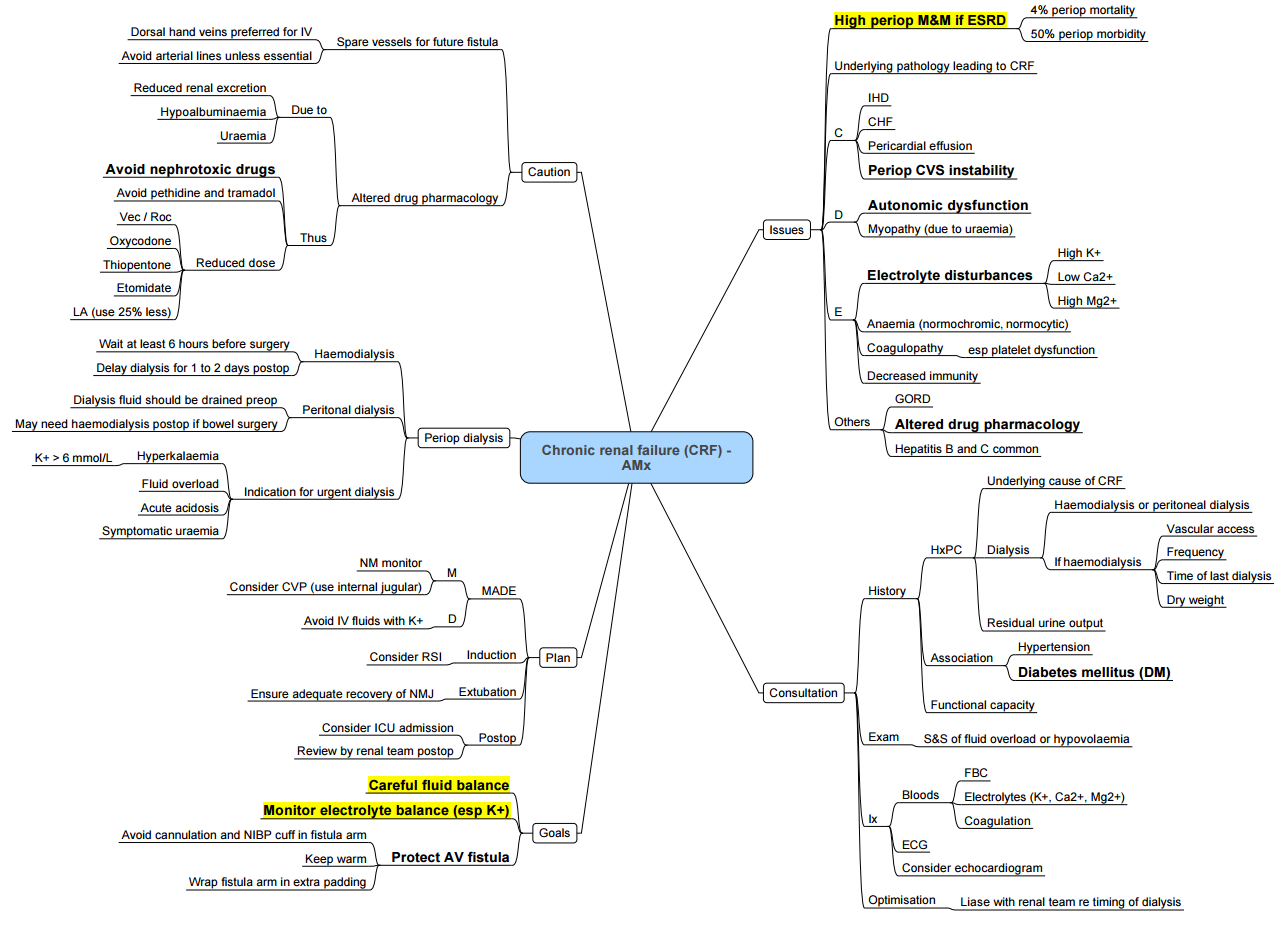
View or edit this diagram in Whimsical.
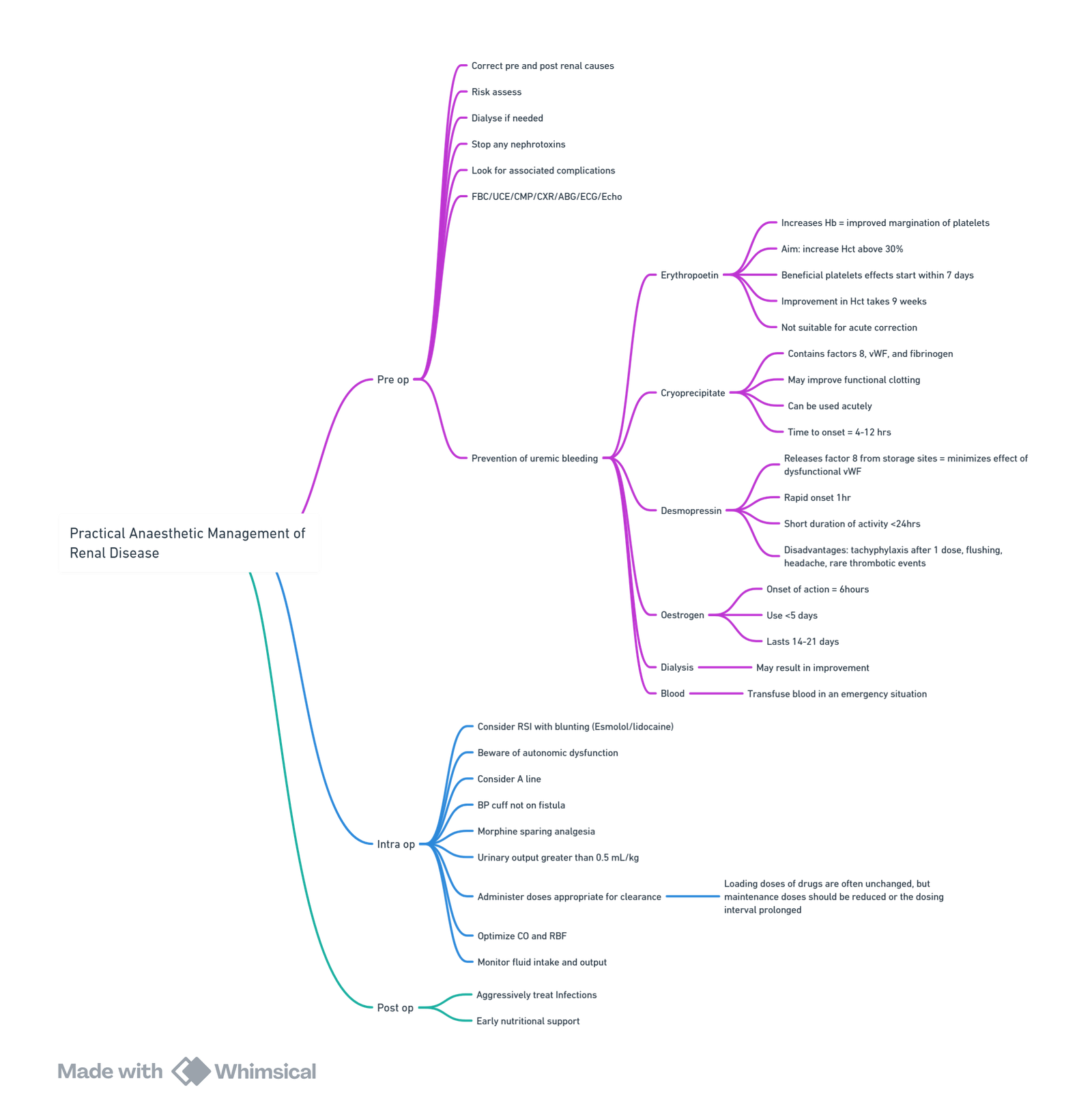
Preoperative Considerations
- Allow 4–6 hours to elapse after haemodialysis before surgery to permit fluid compartment equilibration and metabolism of residual heparin.
Complications Specific to Anaesthesiologists
- Cardiovascular Dysfunction: Tailoring of blood pressure, cardiac risk assessment, management of heart failure.
- Electrolyte and Metabolic Disorders: Hypokalemia, calcium salt management, adequate solution monitoring.
- Coagulopathy: Management includes transfusion, erythropoiesis-stimulating agents (ESA), heparin-free haemodialysis, and discontinuation of antiplatelet therapy.
- Disturbance of Equilibrium: Goal-directed therapy, stroke volume variation (SVV), central venous oxygen saturation (ScvO₂), fluid therapy management.
- Pharmacologic Issues: Appropriate drug choice.
- Renal Anemia: ESA, transfusion, prevention of alloimmunization.
General Rules
- Reversible decreases in renal blood flow (RBF), glomerular filtration rate (GFR), urinary flow, and sodium excretion occur during both neuraxial and general anaesthesia.
- These changes are usually less pronounced during neuraxial anaesthesia.
- Most changes are indirect and mediated by autonomic and hormonal responses to surgery and anaesthesia.
- Acute kidney injury (AKI) is less likely when adequate intravascular volume and normal blood pressure are maintained.
- Currently utilized volatile anesthetic agents do not cause AKI in humans.
Risk Factors for Developing AKI Perioperatively
Patient Factors
- Chronic diseases: Kidney disease, heart failure, hypertension, peripheral arterial disease, chronic obstructive pulmonary disease, diabetes mellitus, alcoholism.
- Male gender.
- Obesity.
- Age > 65 years.
Surgery Factors
- Emergency surgery.
- Non-renal solid organ transplant.
- Cardiac bypass time.
- Aortic cross-clamp.
Other Factors
- Acute illness.
- Sepsis.
- Multi-organ dysfunction.
- Nephrotoxic drugs (ACE inhibitors, ARBs, diuretics, radio-opaque intravenous contrast).
Indirect Anaesthesia Effects
Cardiovascular System (CVS)
- Decreased mean arterial pressure (MAP), decreased venous tone leading to venous pooling, decreased systemic vascular resistance (SVR), heart rate (HR), contractility, and cardiac output (CO).
- Blood pressure decreases below the limits of autoregulation reduce RBF, GFR, urinary flow, and sodium excretion, adversely impacting kidney function.
Neurological
- Increased sympathetic tone (anxiety, pain, light anaesthesia, surgical stimulation).
- Increases renal vascular resistance and activates several hormonal systems, reducing RBF, GFR, and urine output.
Endocrine
- Stress response: Increases in epinephrine, norepinephrine, renin, angiotensin II, aldosterone, antidiuretic hormone (ADH), adrenocorticotropic hormone (ACTH), and cortisol.
- Catecholamines, ADH, and angiotensin II reduce RBF by inducing renal arterial constriction.
- Nonosmotic release of ADH favors water retention and may result in hyponatremia.
- The endocrine response to surgery and anaesthesia contributes to transient fluid retention postoperatively.
Drugs and Toxins Associated with Acute Kidney Injury
Decreased Renal Perfusion
- NSAIDs, ACE inhibitors, radiocontrast agents, amphotericin B, cyclosporine, tacrolimus.
Direct Tubular Injury
- Aminoglycosides, radiocontrast agents, amphotericin B, methotrexate, cisplatin, foscarnet, pentamidine, heavy metals, myoglobin, hemoglobin, intravenous immunoglobulin, HIV protease inhibitors.
Intratubular Obstruction
- Radiocontrast agents, methotrexate, acyclovir, sulfonamides, ethylene glycol, uric acid, cocaine, lovastatin.
Immunological-Inflammatory
- Penicillin, cephalosporins, allopurinol, NSAIDs, sulfonamides, diuretics, rifampin, ciprofloxacin, cimetidine, proton pump inhibitors, tetracycline, phenytoin.
Blood Workup
- FBC: Normochromic normocytic anaemia due to decreased erythropoiesis. Maintain hemoglobin (HB) at 8-10 g/dL.
- UCE and CMP: Hyperkalemia, hyponatremia due to water retention, hypocalcemia, and hyperphosphatemia.
- ABG: Mild metabolic acidosis with poor compensatory ability.
- Coagulation: INR, APTT, and platelet count usually normal. Uremia affects platelet function and prolongs bleeding time. Dialysis improves coagulation once heparin wears off. Thrombocytopathy is not corrected by platelet transfusion but may be improved by cryoprecipitate or desmopressin (0.3 micrograms/kg in 30 mL of saline over 30 min).
Preoperative Therapy Recommendations
Continue
- β-blockers
- Calcium channel blockers
- Digoxin
- Statins
- H₂-blockers and proton pump inhibitors
- Inhaled β-agonists
- Glucocorticoids
- Leukotriene inhibitors
Discontinue
- α₂-agonists
- Non-statin hypolipidemic agents
- Theophylline
Recommendations for Nephroprotective Measures
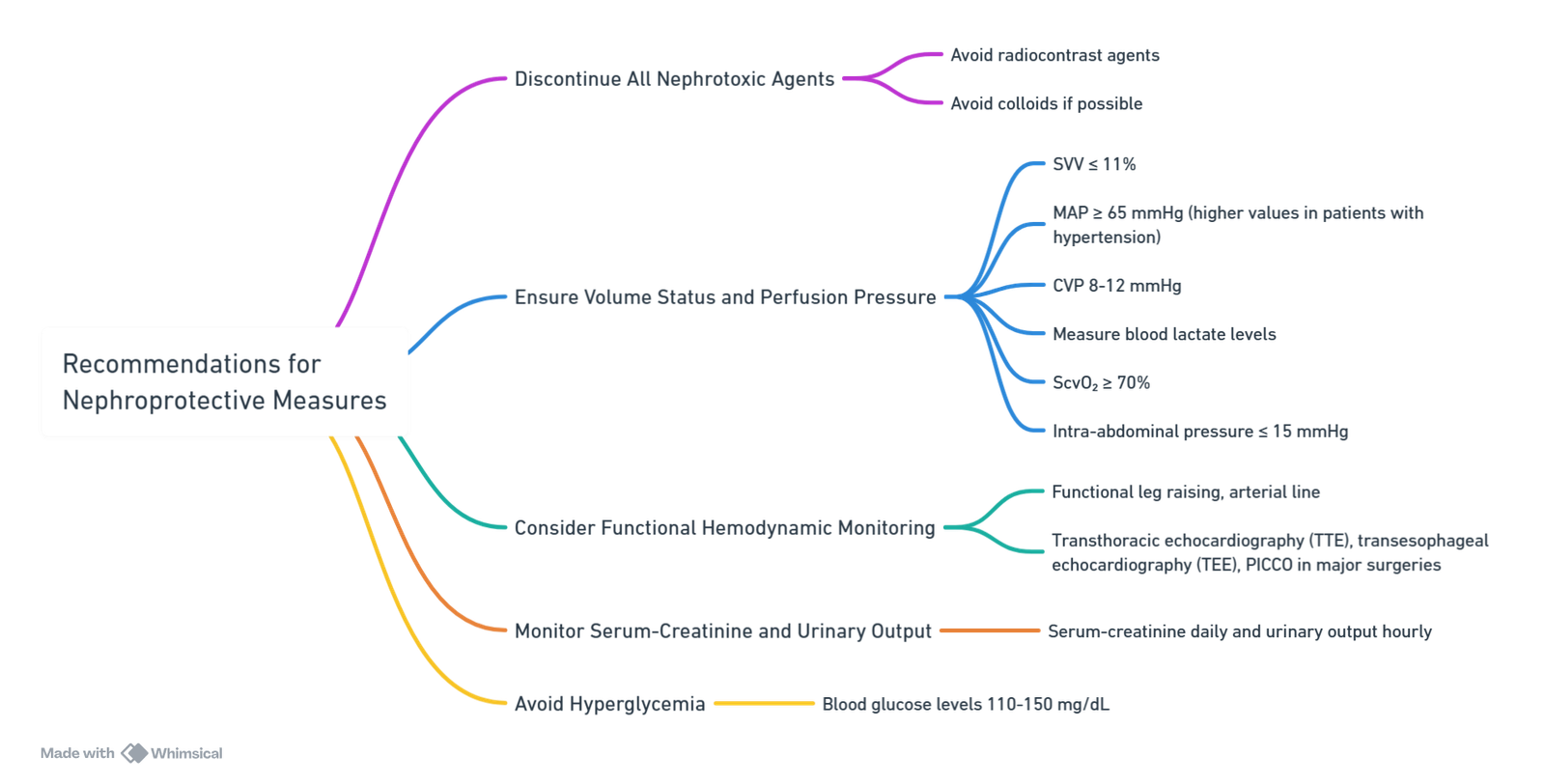
View or edit this diagram in Whimsical.
Aetiologies of Perioperative Acute Kidney Injury
Pre-renal
- Preoperative: Hypovolemia (gastrointestinal losses, hemorrhage, third spacing), sepsis, cardiac failure, increased intra-abdominal pressure, cirrhosis, hepatorenal syndrome.
- Intraoperative: Hypovolemia (insensible losses, hemorrhage, over diuresis), hypotension (low SVR, anesthesia-induced), low CO (heart failure, anesthesia and cardiopulmonary bypass CPB-induced), increased intra-abdominal pressure, aortic cross-clamp.
Intrinsic
- Preoperative and Perioperative: Inflammation (patient comorbidities: chronic kidney disease, diabetes mellitus, obesity, atherosclerosis), drug-induced (antibiotics, aspirin, phenytoin, furosemide, NSAIDs, clopidogrel, tacrolimus), radiocontrast agents, endogenous nephrotoxins (hemoglobin and myoglobin), acidosis, infection, CPB, anemia (packed red blood cell administration), fluid solutions (hydroxyethyl starch, chloride-rich solutions).
Post-renal
- Preoperative: Tumor, prostatic enlargement, calculi, blood clots, neurogenic bladder.
- Intraoperative: Surgical intervention or damage.
Anaesthesia Drugs and CKD
Principles
- Loading doses of drugs are often unchanged, but maintenance doses should be reduced or the dosing interval prolonged.
- Hypoalbuminaemia and acidosis increase the free drug availability of highly protein-bound drugs
- Most anaesthetic drugs and techniques reduce renal blood flow, GFR, and urine output
Anaesthetic Drugs
Premedication
- Drugs safe in CRF: Lormetazepam, midazolam, temazepam
Induction
- Drugs safe in CRF: Propofol
- Drugs safe in limited or reduced doses: Ketamine, etomidate, thiopental
- Reduce the doses of benzodiazepines, thiopental, and etomidate by ~30% because of changes in protein-binding, volume of distribution, and cardiac function.
- Propofol dose needs to be increased
- Wake-up following infusion is faster
Maintenance
- Drugs safe in CRF: Isoflurane, desflurane, halothane, propofol
- Drugs safe in limited or reduced doses: Sevoflurane
- Drugs contraindicated in CRF: Enflurane
Muscle Relaxants
- Drugs safe in CRF: Suxamethonium, atracurium, cisatracurium
- Drugs safe in limited or reduced doses: Vecuronium, rocuronium
- Drugs contraindicated in CRF: Pancuronium
Opioids
- Drugs safe in CRF: Alfentanil, remifentanil
- Drugs safe in limited or reduced doses: Fentanyl, morphine, oxycodone
- Drugs contraindicated in CRF: Pethidine, codeine, tramadol
Local Anaesthetics
- Drugs safe in limited or reduced doses: Bupivacaine, lidocaine (reduce dose by 25%)
- Reduced duration of action
Analgesics
- Drugs safe in CRF: Paracetamol
- Drugs contraindicated in CRF: NSAIDs
Drugs that Accumulates in Renal Disease
- Pancuronium
- Atropine Glycopyrrolate
- Metoclopramide
- Cimetidine Ranitidine
- Digitalis
- Diuretics
- Calcium channel antagonists Diltiazem Nifedipine
- β-Adrenergic blockers:Atenolol Nadolol Pindolol Propranolol
- Antihypertensives Captopril Clonidine Enalapril Hydralazine Lisinopril Nitroprusside (thiocyanate)
- Antiarrhythmics Bretylium Disopyramide Encainide (genetically determined) Procainamide Tocainide Bronchodilators Terbutaline Psychiatric
- Lithium
- Antibiotics Aminoglycosides Cephalosporin
Penicillins Tetracycline Vancomycin - Anticonvulsants: Carbamazepine Ethosuximide Primidone
- Other: Sugammadex
Management of AKI
Acute Management
- Risk assessment, primary prevention, early diagnosis.
- Hemodynamic stabilization of CO and BP.
- Adequate volume expansion without overload/accumulation. Sepsis guidelines allow 30 mL/kg in the acute, early phase (supported by VASTT trial), continuing as long as patient is responsive to fluid challenge, followed by a conservative strategy thereafter (FACTT trial).
Further Treatment
- Assessment of the cause and volemic status.
- Avoid nephrotoxic agents.
- Rationalized exposure to contrast.
- Management of complications:
- Fluid overload: Fluid restriction, trial of diuretics, positive pressure ventilation (PPV) ± intubation.
- Hyperkalemia: Potassium shift therapies.
- Nutritional support.
- Renal replacement therapy (RRT) in the context of lab trends.
Management of AV-Fistula
- Avoid Cannulation and Non-Invasive Blood Pressure (NIBP) in This Arm: To prevent damage and maintain the integrity of the fistula.
- Cannulate the Dorsum of the Hand: This practice avoids damage to the veins in the forearm and antecubital fossa, which are needed for future fistulae.
Anaesthesia for AV Fistula Formation
- Location of Fistula Formation:
- Brachiobasilic Fistula: Local infiltration is used.
- Brachiocephalic Fistula: An axillary or supraclavicular brachial plexus block is recommended. Additional local anesthesia (LA) may be required in the axilla.
- Avoid Hypotension: Preventing hypotension is crucial to avoid fistula thrombosis.
- Usage Timeline:
- Fistula: Can be used for dialysis after 3–4 weeks.
- Synthetic Grafts: Can be used immediately but do not last as long as fistulas.
Links
- Renal Physiology
- Renal replacement therapy
- Renal transplant
- ICU and renal disease
- Renal protection
- Intra-op renal dysfunction
- ICU and liver disease
References:
- Allman K, Wilson I, O’Donnell A. Oxford Handbook of Anaesthesia. Vol. 4. Great Clarendon Street, Oxford, OX2 6DP, United Kingdom: Oxford University Press; 2016.
- Butterworth J, Mackey D, Wasnick J. Morgan and Mikhail’s Clinical Anesthesiology, 7th Edition. 7th edition. New York: McGraw Hill Medical; 2022.
- The Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- ICU One Pager. (2024). Retrieved June 5, 2024, from https://onepagericu.com/
Summaries
CRF
Renal disease and anaesthesia
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “469f9118-62c1-4ab2-9cf9-e4cfb46da2b6”