{}
Summary
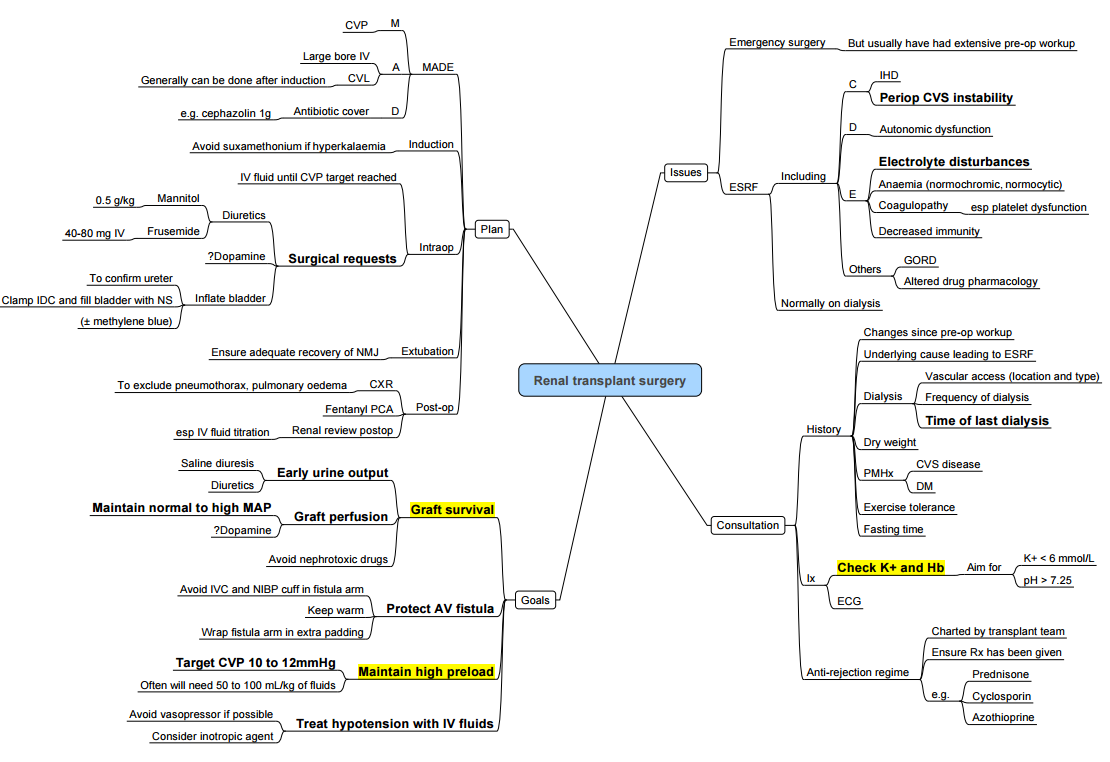
Anaesthesia for Renal Transplants
Preoperative Assessment
- Aim to limit cold ischaemic time.
- Important considerations:
- Associated comorbidities.
- Cardiovascular risk.
- Fluid status.
- IV access history (including AV fistulas, dialysis lines, previously stenosed or thrombosed vessels).
Anaesthesia
- Induction: Propofol with alfentanil or fentanyl.
- RSI may be indicated if delayed gastric emptying is a concern.
- Maintenance: Volatile or TIVA.
- Muscle relaxant:
- Atracurium.
- Suxamethonium provided K+ < 5 mmol/L or high dose rocuronium as part of RSI.
- Sugammadex (not licensed in severe renal impairment but appears safe and to provide complete reversal of blockade).
Targets
- Warm and well perfused.
- Adequate MAP (ideally within 20% of baseline).
- Euvolaemia.
- CVP 10-15 mmHg.
Monitoring and Access
- Monitoring as per AAGBI/ SASA guidelines.
- Arterial line not essential unless indicated by comorbidities.
- NIBP on opposite side to AV fistula.
- 20G IV access is sufficient.
- Central venous access (dialysis line if no previous fistula).
- Oesophageal temperature probe and urinary catheter.
Analgesia
- IV paracetamol.
- Fentanyl boluses titrated to effect (usually 200-300 mcg).
- TAP blocks or local infiltration by surgeons.
- Fentanyl PCA postoperatively.
Fluid Management
- Important factor in post-transplant renal function.
- Typically require ~40 ml/kg crystalloid
- Colloid and blood rarely required.
- Caution regarding overzealous filling which can strain the myocardium.
- Transfusion trigger of 7 → may cause autoimmune activation and early graft rejection
Suitability of Drugs Commonly Used During Transplantation Surgery
| Use | Avoid |
|---|---|
| Volatile anaesthetics: Iso/Sevo/Desflurane | Enflurane |
| Neuromuscular blocking drugs: Cis/atracurium | Pancuronium, Sugammadex |
| Rapid sequence induction: Rocuronium (1.2mg/kg), Succinylcholine (if K+ < 5mmol/l) or Cisatracurium (1.5mg/kg) | – |
| Analgesics: All fentanyl analogues | NSAIDS Morphine |
| Diuretics: Mannitol, Furosemide |
Immunosuppressive Medications in Renal Transplantation
- Calcineurin Inhibitors:
- Tacrolimus
- Cyclosporine
- Antiproliferative Agents:
- Mycophenolate Mofetil
- Mycophenolate Sodium
- Azathioprine
- mTOR Inhibitor:
- Sirolimus
- Steroids:
- Prednisone
- Sequence of drugs before reperfusion:
- Promethazine, Hydrocortisone (or methylprednisolone)
- Natalizumab or Grafalon (Monoclonal antibodies T-Cell). Given over 30 min via CVP
Anaesthetic Considerations in Recipients of Renal Transplants Presenting for Non-transplant Surgery
Summary
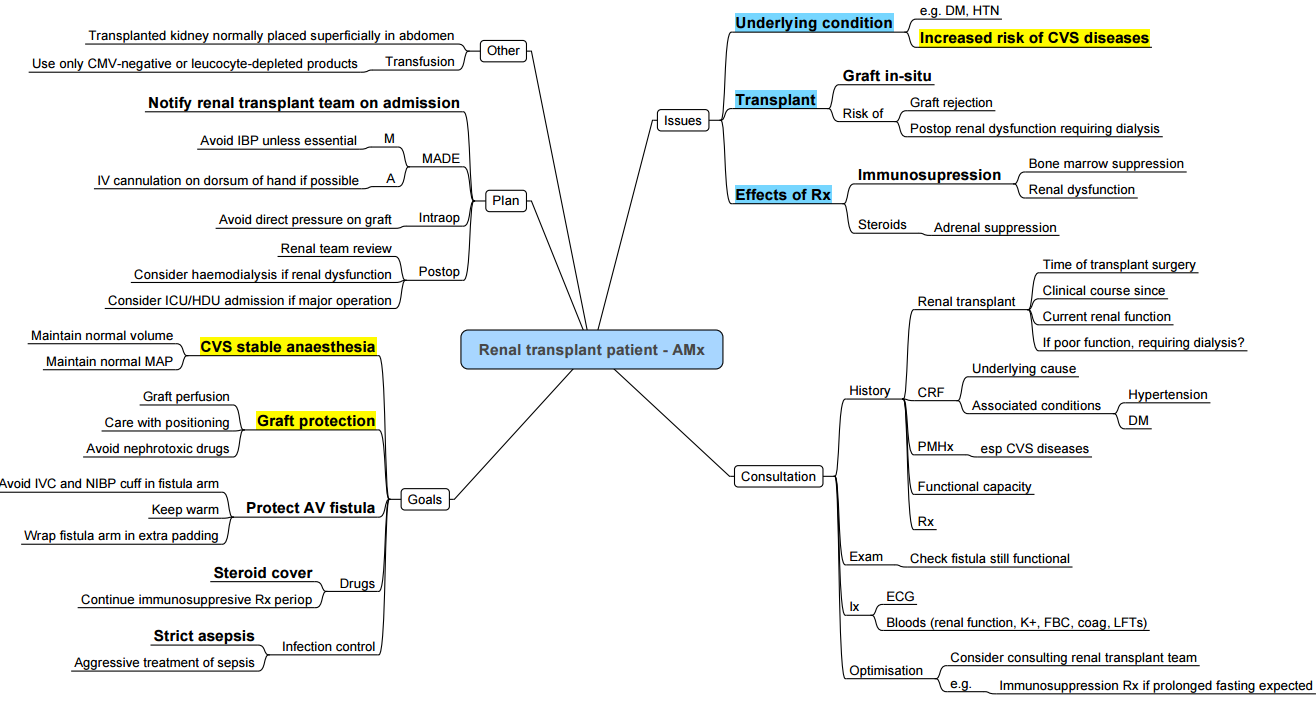
Ongoing Management of Comorbidities
- Diabetes Mellitus (DM)
- Hypertension (HPT)
- Ischemic Heart Disease (IHD)
- Dyslipidemia
- Vasculitis
Effects of Steroids and Immunosuppressants
- Consider potential side effects and interactions (source required for specific details).
Drug Considerations (Depending on Renal Function)
- Morphine: Risk of accumulation of metabolites.
- Non-depolarizing Muscle Relaxants (NDMR): Effects can be unpredictable.
- NSAIDs: Contraindicated regardless of renal function.
Avoid Hypovolemia and Hypotension
- Important to prevent exacerbation of renal injury.
Multisystem Disease and Renal Dysfunction
- Renal dysfunction is likely due to multisystem disease.
- Important to inquire about the primary disease (e.g., DM) and associated comorbidities (e.g., HPT, hyperlipidemia, coronary artery disease (CAD).
- Renal Function: May have reduced GFR; check post-transplant baseline.
Anaesthesia for Living Donor Renal Transplant Nephrectomy
Classification of Renal Transplants by Donor Organ Source
- Deceased Donor
- Brainstem dead, heart-beating.
- Non-heart-beating.
- Living Donor
- Related: The donor is genetically related to the recipient (parent, child, sibling, half-sibling, aunt, uncle, niece, nephew, first cousin).
- Unrelated
- Emotional connection.
- No emotional connection.
- Altruistic.
- Paired.
- Pooled: Occasionally, more than two donors and two recipients will be involved in a swap. Each recipient gains from a transplant that they would not otherwise have had. The donors might not have given their kidney to the person they know, but that person will have received a kidney from one of the other pooled donors.
Surgical Techniques Used for Living Donor Nephrectomy (LDN)
- Open.
- Laparoscopic LDN.
- Hand-assisted laparoscopic LDN.
- Robot-assisted laparoscopic LDN.
Perioperative Anaesthetic Care Key Messages
- No routine prophylactic antibiotic (clean procedure).
- Comprehensive thromboembolism prophylaxis:
- LMWH, graduated stockings, pneumatic compression devices.
- Consultant Surgeon and Consultant Anaesthetist present.
- Careful positioning to prevent pressure damage.
- Combination of local and regional anaesthesia with GA:
- Epidural.
- Paravertebral block.
- Transverse Abdominal Plain Block.
- LA catheter in wound.
- Local infiltration by surgeon.
- Avoid Non-steroidal Anti inflammatory drugs.
- Wide bore IV access.
- Non-invasive monitoring, unless patient-specific indication.
- Fluid preloading (e.g. 1 litre of Normal Saline post-induction).
- Positive fluid balance throughout procedure.
- Avoid vasoconstrictors.
- Keep renal perfusion pressures / MAP at preoperative values.
- Heparin (e.g. 5000 IU) before the application of arterial clamp.
- Protamine (e.g. 50 mg) after kidney isolation.
- High normal urine output (>100 ml /h)–Mannitol 0.5 g/kg can be used.
- Fentanyl PCA.
- Avoid hypothermia.
Frequency of Complications for Donors
- Pneumonia: 9.3%.
- Pulmonary atelectasis: 7.4%.
- Urinary tract infection: 5.3%.
- Wound infection: 4.3%.
- Pneumothorax: 3.1%.
- Urinary retention: 1.0%.
- Ileus: 1.0%.
- Pleural effusion: 0.9%.
- Intra-abdominal haematoma: 0.5%.
- Pulmonary embolus: 0.4%.
- Wound herniation: 0.3%.
- Splenectomy: 0.2%.
- Deep venous thrombosis: 0.2%.
- Intra-abdominal abscess: 0.2%.
- Other unspecified: 5.3%.
Links
- Brainstem death
- Transplants and organ donation
- Renal Physiology
- ICU and renal disease
- Renal replacement therapy
References:
- O’Brien, B. and Koertzen, M. (2012). Anaesthesia for living donor renal transplant nephrectomy. Continuing Education in Anaesthesia Critical Care &Amp; Pain, 12(6), 317-321. https://doi.org/10.1093/bjaceaccp/mks040
- Rabey, P. (2001). Anaesthesia for renal transplantation. BJA CEPD Reviews, 1(1), 24-27. https://doi.org/10.1093/bjacepd/1.1.24
- Mayhew, D., Ridgway, D. M., & Hunter, J. (2016). Update on the intraoperative management of adult cadaveric renal transplantation. BJA Education, 16(2), 53-57. https://doi.org/10.1093/bjaceaccp/mkv013
- Meredith, S., Basavaraju, A., & Logan, N. (2021). Anaesthesia for renal transplantation. Anaesthesia &Amp; Intensive Care Medicine, 22(8), 500-504. https://doi.org/10.1016/j.mpaic.2021.06.012
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “5f57cc23-5fbd-44c4-9168-b2fd4a719a36”



