- Arterial Circulation
- Arterial Pressure Wave Forms
- Characteristic Waveforms
{}
Arterial Circulation
Distribution of Circulating Blood Volume:
- Arterial system: 15%
- Venous system: 65%
- Pulmonary circulation: 10%
- Cardiac chambers: 5%
- Capillaries: 5%
Blood Flow and Velocity
Blood Velocity and Flow
V=Q’/A
- V (cm/s): blood velocity (distance travelled per unit time)
- Q˙ (mL/s): blood flow (volume of blood passing a point per unit time)
- A (cm2): cross-sectional area of the vessel
Blood Flow Dynamics
-
Arterial System:
- Blood travels from large arteries to smaller arteries and arterioles.
- As vessels branch, individual cross-sectional area decreases, but total cross-sectional area at each bifurcation level increases.
-
Capillaries to Veins:
- From capillaries to venules and veins, the cross-sectional area of each vessel increases, while the total cross-sectional area decreases.
- Blood from the lower body drains into the inferior vena cava (IVC), while that from the upper body enters the superior vena cava (SVC).
-
Right Atrium Flow:
- Venous return to the right atrium approximates cardiac output, with adjustments for fluid lost to interstitial spaces and returned via lymphatics.
Distant Factors
- Direct sympathetic tone: Does not affect denervated free flaps.
- Humoral factors:
- Catecholamine release from adrenals and sympathetic nerve endings.
- Vasopressin and angiotensin.
Local Factors
- Myogenic response: Low hydrostatic pressure leads to dilatation and vice versa.
- Metabolic factors: Vasodilatation occurs secondary to raised K+, H+, osmolarity, CO2, and adenosine, and reduced PO2.
Rheology
- Deformability of RBC and haematocrit (Hct).
- Factors described by the Hagen–Poiseuille equation.
Arterial System Dynamics
Hagen–Poiseuille Equation
ΔP=8Q˙ηl/ πr4
- ΔP: pressure drop along the tube
- Q˙: flow
- η: viscosity
- l: tube length
- r: radius
Rearranged form:
Q˙=ΔPπr4/8ηl
Darcy’s Law
Pressure equals flow times resistance.
Hence, if ΔP is pressure and Q˙ is flow, then resistance to flow is 8ηl/πr4
Important Considerations
- The most important factor affecting flow is the tube radius.
- Hagen–Poiseuille equation provides only an approximation of blood flow due to:
- Pressure drop along the vessel is not continuous; it has a pulsatile component.
- Blood does not behave like a Newtonian fluid (blood viscosity varies with temperature and Hct).
- Fahraeus–Lindqvist effect: In small vessels, RBCs stream towards the centre, leaving plasma at the walls. Plasma has lower viscosity than whole blood, reducing resistance to flow, opposing the tendency for resistance to increase as vessel radius decreases, especially in arterioles and capillaries.
- Vessels are not uniform rigid tubes: Large vessels are distensible; an increase in pressure causes an increase in vessel radius, reducing resistance and increasing flow.
- Myogenic autoregulation: Intrinsic ability of an arteriole to maintain constant blood flow despite changes in intraluminal pressure.
Arteriole Function
- Convert pulsatile flow to continuous flow before reaching capillaries.
- Regulate blood distribution by modulating vascular resistance.
- Adjust capillary hydrostatic pressure to control fluid exchange between intravascular and interstitial compartments.
Control of Vasoconstriction and Dilation
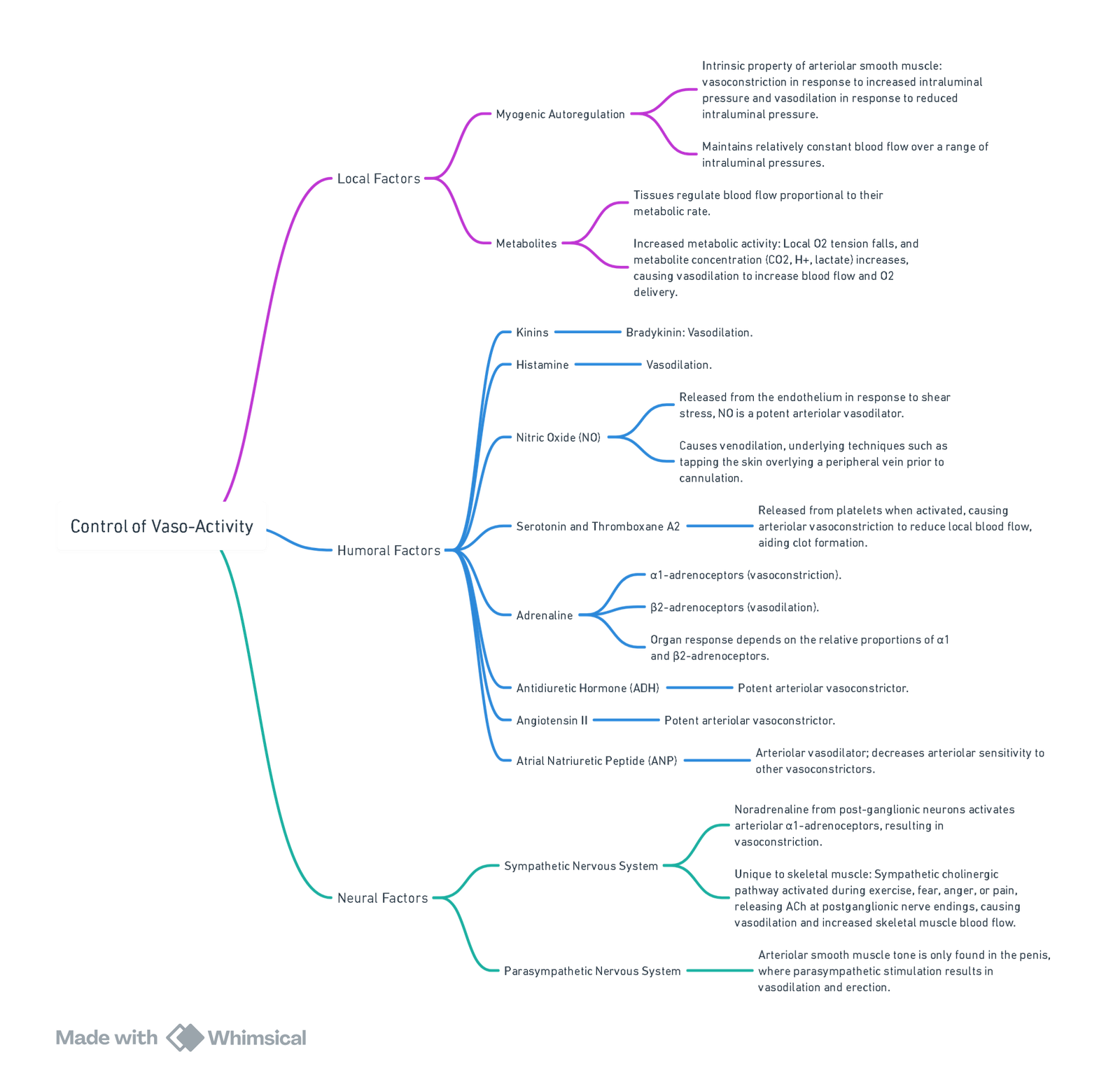
View or edit this diagram in Whimsical.
Differences between the Systemic and Pulmonary Circulations
| Feature | Systemic Circulation | Pulmonary Circulation |
|---|---|---|
| Arteries | ||
| Typical pressure | 140/80 mmHg | 25/8 mmHg |
| Typical mean pressure | 100 mmHg | 15 mmHg |
| Vessel wall | Thick-walled, elastic | Thin-walled, distensible |
| Resting vasoconstrictor tone | Highly constricted at rest | No vasoconstrictor tone at rest |
| Arterioles | ||
| Vessel wall | Thick walls, small lumen, muscular | Thin walls, large lumen |
| Vessel resistance | High resistance, typical SVR 1600 dyn s cm5 | Low resistance, typical PVR 160 dyn s cm5 |
| Response to hypoxia | Vasodilatation | Vasoconstriction |
| Capillaries | ||
| Wall thickness | Thin, to allow exchange of O2, CO2 , and nutrients | Extremely thin, to allow efficient gas exchange |
| Blood flow | Continuous, high resistance in arterioles | Pulsatile, low resistance in arteries and arterioles |
| Distensibility/compressibility | Little change in radius | Compressible with increased alveolar pressure; distensible with increased pulmonary venous pressure |
| Veins | ||
| Typical mean pressure | 2 mmHg | 5 mmHg |
| Venous reservoir | High venous capacitance, holding >1000 mL of blood which can be released back into the circulation if required | Holds around 500 mL of blood which can be released back into the circulation if required |
Arterial Pressure Wave Forms
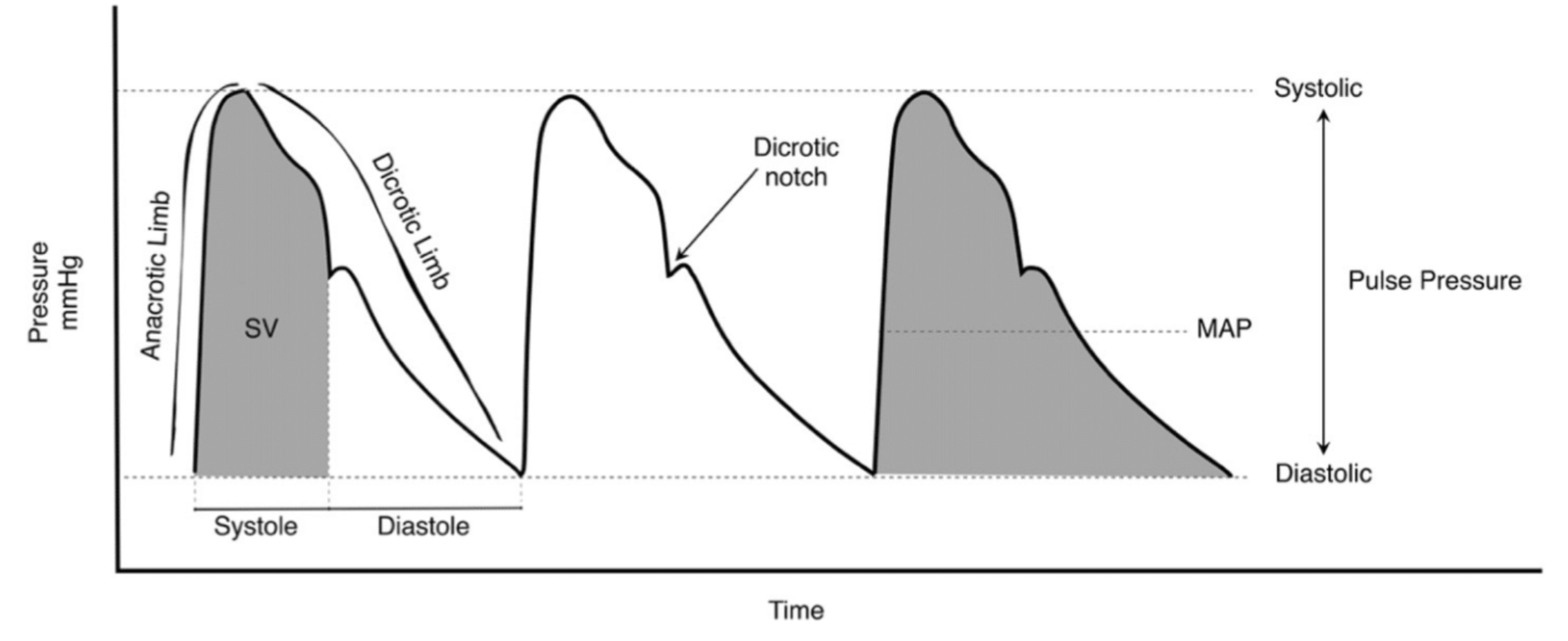
- The arterial pressure wave, not the blood flow wave, creates the palpable ‘radial pulse.’ Pressure waves travel faster than blood flow.
Changes Along the Arterial Tree
- Distal Movement Effects:
- Increased steepness in the upstroke.
- Elevated systolic blood pressure (SBP) and decreased diastolic blood pressure (DBP).
- Mean arterial pressure (MAP) remains constant.
- The dicrotic notch shifts lower on the pressure curve, evolving into a dicrotic wave.
Characteristic Waveforms
Myocardial Contractility
-
Waveform Upstroke:
- Slope reflects myocardial contractility.
- A steeper upstroke indicates greater pressure generated over time.
- A reduced slope is characteristic of conditions like aortic stenosis.
-
Systemic Vascular Resistance (SVR):
- The waveform downstroke reveals SVR.
- A steep downstroke and low dicrotic notch imply low SVR, producing a thin and pointed waveform.
- A high dicrotic notch corresponds to elevated SVR.
- The waveform downstroke reveals SVR.
Systemic Vascular Resistance (SVR)
- The downstroke of the arterial pressure waveform provides information about SVR:
- A steep downstroke with a low dicrotic notch indicates a low SVR, resulting in a thin and pointed arterial waveform.
- A high dicrotic notch implies a high SVR.
Windkessel Effect
- The elastic aorta accommodates stroke volume (SV), buffering the rise in intra-aortic pressure.
- During diastole:
- Aortic wall recoil converts stored potential energy into kinetic energy, sustaining diastolic blood pressure (DBP) and maintaining blood flow.
Ageing And Loss of Windkessel Effect
- Elastin degradation reduces compliance.
- Impaired aortic expansion leads to higher SBP, contributing to systolic hypertension in older adults.
Capillaries
Functional Anatomy
- Capillaries deliver nutrients to and remove metabolites from tissues.
- They help distribute body water between intravascular and interstitial fluid compartments.
- The capillary wall, composed entirely of endothelium and supported by a basement membrane, is only one cell thick.
Mechanisms of Exchange
- Simple Diffusion: Movement of gases (O₂, CO₂) and small lipophilic molecules (e.g., anaesthetic agents) per Fick’s law.
- Bulk Flow: Water and dissolved solutes move along hydrostatic pressure gradients.
- Pinocytosis: Energy-dependent transport of substances via vesicles, with minimal contribution to exchange.
Starling Law
Forces Influencing Fluid Movement
-
Forces moving fluid out of the capillary:
- Capillary hydrostatic pressure Pc (Arterial: 36 mmHg; Venous: 10 mmHg)
- Interstitial fluid oncotic pressure πi (3 mmHg)
-
Forces moving fluid into the capillary:
- Interstitial fluid hydrostatic pressure Pi (2 mmHg)
- Plasma oncotic pressure πc(24 mmHg)
Starling Filtration Equation
Net fluid filtration across capillary wall=Kf[(Pc−Pi)−σ(πc−πi)]
- Kf is the filtration coefficient, a constant related to the permeability of the capillary wall (high Kf indicates high water-permeability, whilst low Kf indicates low water-permeability)
- σ is the reflection coefficient, a constant that represents the permeability of the capillary to proteins (σ = 1 implies that the capillary wall is 100% impermeable)
- Capillary walls normally impermeable to proteins and formula can be simplify as: (Pc–Pi)–(πc–πi).
- Pi; πc; πi usually constant. Pc is therefore the main determinant of whether fluid is filtered or reabsorbed
Normal Conditions
-
Arterial (Filtration):
Net filtration pressure=(36−2)−(24−3)=13 mmHg
- There is bulk flow out of the capillary (filtration).
-
Venous (Absorption):
Net filtration pressure=(10−2)−(24−3)=−13 mmHg
-
Autotransfusion in haemorrhage:
500 mL of fluid can be mobilized within 30 min from the interstitial space to the intravascular space. Reduced Cp and net absorption
Endothelium
Functions
1. Transfer
- Controls the movement of gases, nutrients, and metabolites across the capillary.
2. Synthesis of Vasoactive Substances
- Vasodilators: Nitric oxide (NO), prostacyclin (PGI2)
- Vasoconstrictor: Endothelin (ET)
3. Haemostasis
- Anticoagulants:
- Endothelial cell surface receptor thrombomodulin binds thrombin. The thrombomodulin–thrombin complex activates protein C, a potent anticoagulant.
- NO and PGI2 inhibit platelet aggregation.
- Heparin sulphate activates the plasma protein antithrombin III, which inactivates thrombin and factor Xa.
- Coagulants:
- von Willebrand factor (vWF) binds to factor VIII and activates platelets.
4. Inflammation
- Interleukin 1 and tissue necrosis factor stimulate the endothelium to express adhesion molecules, attracting neutrophils and lymphocytes.
Venous System
Functions
-
Blood Storage:
- The venous system is 30× more compliant than arteries and holds ~65% of blood volume.
-
Venous Return:
- Assisted by:
- Valves: One-way flow.
- Pressure Gradient: Enhanced by venous filling and sympathetic tone.
- Respiratory Pump: Thoracic pressure changes during respiration.
- Skeletal Muscle Pump: Active muscle contractions propel blood.
- Body Position: Supine posture increases venous return.
- Assisted by:
-
Thermoregulation: Venous blood distribution assists in heat dissipation or retention.
Resistance to Flow
- Hagen–Poiseuille Equation: Resistance to flow=8ηl/πr4
- Shape of the Lumen with Intraluminal Pressure:
- High intraluminal pressure: Circular lumen, less resistance.
- Low intraluminal pressure: Elliptical lumen, more resistance.
- Intraluminal pressure decreases along the venous system: Venules: 10–15 mmHg; veins: 4–8 mmHg; inferior vena cava (IVC): 0–2 mmHg. Venules, therefore, have a circular lumen, providing minimal resistance to blood flow. A collapsed IVC can significantly increase flow resistance.
CVP Waveform
- Normal CVP: 2–8 mmHg
Components
- a wave: Increase in pressure during right atrial contraction.
- c wave: Coincides with carotid pulsation. During early systole, right ventricular contraction causes the tricuspid valve to bulge into the right atrium, leading to a small increase in CVP.
- x descent: Atrial relaxation and downward movement of the right atrium during right ventricular contraction, leading to rapid right atrial filling.
- v wave: Continued venous return to the right atrium during ventricular systole; right atrial filling with a closed tricuspid valve.
- y descent: Decrease in CVP after the tricuspid valve opens, allowing blood flow from the right atrium into the right ventricle.
Abnormal Shapes
- Atrial Fibrillation (AF): Loss of a waves.
- Third-degree Heart Block: Independent atrial and ventricular contraction results in occasional large a waves (‘cannon a waves’) when atria contract with a closed tricuspid valve.
- Tricuspid Regurgitation: Ventricular systole ejects blood into the right atrium, increasing CVP. The CVP waveform has a ‘giant v wave’, replacing the c wave, x descent, and v wave.
Physiological Changes During Haemorrhage
Stages of Compensation
Immediate (Seconds)
- Reflex activation of sympathetic outflow:
- Tachycardia and increased myocardial contractility.
- Vasoconstriction prioritizes blood flow to vital organs (brain, heart, kidneys).
- Respiratory compensation for lactic acidosis (tachypnoea).
Early (Minutes to Hours)
- Transcapillary Refill:
- Fluid moves from interstitial to intravascular compartments.
- Renal Conservation:
- Reduced renal perfusion activates the RAAS and ADH secretion.
- Hormonal Adjustments:
- Increased cortisol promotes fluid retention.
Late (Days)
- Plasma volume restoration:
- Water and electrolytes normalized within 48 hours.
- RBC mass recovery via erythropoiesis (8 weeks).
- Albumin synthesis restored in 4–6 days.
Decompensated Shock
- Persistent hypovolemia leads to vasodilatation, myocardial depression, and hypotension, culminating in circulatory collapse.
Haemorrhagic Shock Classification
| Class 1 | Class 2 | Class 3 | Class 4 | |
|---|---|---|---|---|
| Blood loss (%) | <15 | 15–30 | 30–40 | >40% |
| Blood loss (mL, 70 kg adult) | <750 | 750–1500 | 1500–2000 | >2000 |
| HR (bpm) | <100 | >100 | >120 | >140 |
| SBP (mmHg) | Normal | Normal | Reduced | Very low |
| DBP (mmHg) | Normal | Raised | Reduced | Very low |
| RR (breaths/min) | <20 | 20–30 | 30–40 | >40 |
| Urine output (mL/h) | >30 | 20–30 | 5–15 | <10 |
| Mental status | Normal | Anxious | Confused | Unconscious |
Class 1 and 2 haemorrhagic shock are referred to as compensated shock, where blood pressure is maintained. Class 3 and 4 haemorrhagic shock are decompensated, characterized by hypotension. Decompensated shock is associated with >50% mortality.
Note: ‘Pure’ haemorrhagic shock is unusual. Haemorrhage usually occurs in conjunction with trauma. Following trauma, tissue damage triggers a cascade of inflammatory mediators, resulting in systemic inflammatory response syndrome (SIRS) and organ dysfunction, further increasing mortality.
Links
- Endovascular Abdominal Aortic Aneurysm Repair (EVAR)
- Vascular physiology
- Peripheral Vascular Disease (PVD) and Risk Stratification
References:
- Glover, W. E. (1978). Cardiovascular physiology. Medical Journal of Australia, 2(SP7), 6-6. https://doi.org/10.5694/j.1326-5377.1978.tb116046.x
- Chambers D, Huang CLH, Matthews G. Basic physiology for anaesthetists. Cambridge, United Kingdom: Cambridge University Press; 2015.
- Macdonald, D. (1985). Anaesthesia for microvascular surgery. British Journal of Anaesthesia, 57(9), 904-912. https://doi.org/10.1093/bja/57.9.904
- LITFL Arterial line and pressure transducer. Retrieved October 2023, from https://litfl.com/arterial-line-and-pressure-transducer/
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “104c5813-5d46-488e-aff6-214102fdaddb”



