- Awake Craniotomy
- Anaesthesia for Awake Craniotomy
- Scalp Block
- Overview
- Local Anesthetic and Equipment
- Target Nerves and Injection Sites
- Supraorbital Nerve (Trigeminal Nerve, V1 Distribution)
- Supratrochlear Nerve (Trigeminal Nerve, V1 Distribution)
- Zygomaticotemporal Nerve (Trigeminal Nerve, V2 Distribution)
- Auriculotemporal Nerve (Trigeminal Nerve, V3 Distribution)
- Lesser Occipital Nerve (Second or Third Cervical Spinal Nerve)
- Greater Occipital Nerve (Second Cervical Spinal Nerve)
- Greater Auricular Nerve (Second and Third Cervical Spinal Nerves)
- Adverse Events and Management
- Monitoring Cerebral Perfusion
- Mapping Options
- Overview
- Craniotomy
- Links
- Past Exam Questions
{}
Awake Craniotomy
Introduction
Awake craniotomy is gaining popularity among neurosurgeons and is increasingly recommended for all brain tumor excisions. This technique is crucial for maximizing lesion removal while minimizing damage to the eloquent cortex.
Goals and Objectives
- Tumor Excision: While complete excision is often not feasible due to the widespread migration of tumor cells, the primary goals are to reduce tumor bulk, relieve symptoms, and enhance the efficacy of adjuvant therapies (chemoor radiotherapy).
- Neurological Preservation: Preventing iatrogenic neurological deficits is critical. This requires identifying and preserving brain areas near the tumor that are essential for functions such as speech and motor control.
Functional Brain Mapping
Functional mapping helps achieve a balance between tumor resection completeness and function preservation.
Gold Standard: Direct Cortical Electrical Stimulation
- Conducted while the patient is awake and performing tasks to assess the impact of cortical stimulation.
Preoperative Techniques
These techniques do not measure functionality directly and may be affected by edema or mass effect:
- Functional MRI (fMRI): Measures cortical activity.
- Diffusion Tensor Imaging (DTI): Maps important subcortical fiber pathways but does not assess function.
- Navigated Repetitive Transcranial Magnetic Stimulation (rTMS): Can potentially overcome limitations of fMRI and DTI, though it is limited to cortical mapping only.
Perioperative Techniques
- Motor Evoked Potentials (MEPs) and Somatosensory Evoked Potentials (SSEPs): Allow reliable motor and sensory mapping without the patient being awake. However, they do not assess language and higher functions.
Advantages of Awake Craniotomy
- Increased Lesion Removal: There is growing evidence of improved survival rates with awake craniotomy due to more extensive lesion removal.
- Minimized Neurological Dysfunction: Reduces postoperative neurological deficits.
- Shorter Hospitalization: Results in reduced costs and lower incidence of postoperative complications such as nausea and vomiting.
Contraindications for Awake Craniotomy
- Patient Refusal: Patients must consent to the procedure.
- Inability to Lay Still: Patients who cannot remain still for extended periods.
- Inability to Cooperate: Patients who cannot follow instructions or cooperate during the procedure.
- Severe cognitive impairment or psychiatric illness
- Raised intracranial pressure
- Difficult airway or high aspiration risk
Postoperative Care
- Monitoring: Close neurological monitoring is essential, especially in the first 6 hours post-operation, to detect and manage potential haematomas.
- Hospital Stay: Typically, patients remain in the neurosurgical ward or a high-dependency unit bed for 1-2 days post-operation.
Anaesthesia for Awake Craniotomy
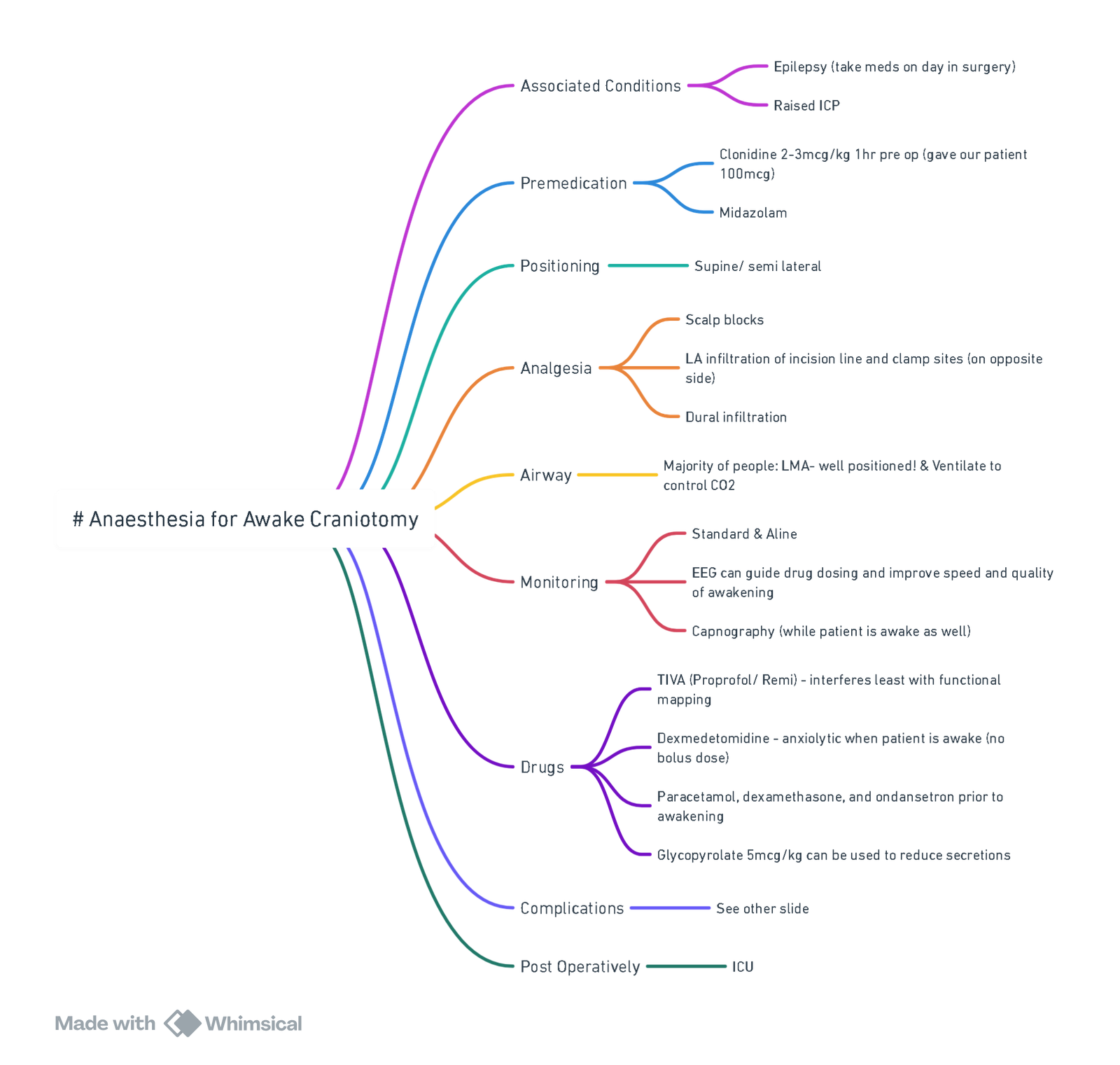
View or edit this diagram in Whimsical.
Preoperative Preparation
- Patient Preparation:
- Discuss preoperative preparation and mapping requirements.
- Assess patient’s presenting problem, including seizure type and frequency, and preoperative neurological deficits.
- Ensure comfort and haemodynamic stability during painful phases (skull pin placement, craniotomy, dural opening) using local anaesthesia, typically provided by a scalp block with bupivacaine, levobupivacaine, or ropivacaine.
- Administer anticonvulsant prophylaxis, ensure adequate plasma levels of chronic medications, and use dexamethasone for tumor surgery.
- Routine administration of antiemetic and antibiotic prophylaxis. Dexamethasone may aid in maintaining brain condition intra-operatively. Avoid NSAIDs.
- Secure large-bore intravenous access and insert an arterial line, usually under sedation or while the patient is asleep.
- Consider Bispectral Index (BIS) monitoring.
- Decide whether to use local anaesthesia, sedation, or general anaesthesia for phases before and after mapping.
Goals
- Ensure patient comfort, wakefulness, and cooperation during the mapping phase.
- Facilitate reliable neurophysiological monitoring signals.
- Maintain a soft and slack brain during resection.
Anesthetic Techniques
GA-Awake-GA Technique
- First Phase (Pre-Mapping):
- General anaesthesia with intermittent positive ventilation via a laryngeal mask airway (LMA).
- Use propofol-remifentanil technique for adequate mechanical ventilation and smooth, fast transition to awake state. Remove LMA once airway reflexes return but before coughing occurs.
- Mapping Phase:
- The patient is awake and cooperative.
- Final Phase (Post-Mapping):
- General anaesthesia resumed for haemostasis, dural, skull, and skin closure.
- Consider this technique if the procedure is expected to last more than four hours.
- Advantages:
- Control ventilation and carbon dioxide concentrations.
- Prevent airway obstruction and hypoventilation.
- Greater depth of anaesthesia during painful parts of surgery.
- Neuromuscular Blocking Agents: Can be used if necessary.
Awake Neuroleptanalgesia
- Initial Sedation: Deep sedation during Mayfield pin application, skin incision, bone flap removal, and dura mater opening.
- Mapping Phase: Decrease or stop sedation for neurocognitive testing and mapping.
- Final Phase: Increase sedation for closure.
- Drug Choices:
- Droperidol and alfentanil or propofol-fentanyl or propofol-remifentanil for intermittent general anaesthesia or sedation.
- Dexmedetomidine: Provides rousable, sleep-like sedation, some analgesia, and maintained respiratory drive.
- Advantages:
- Avoid airway manipulation and its inherent risks.
- Reduce postoperative nausea and vomiting (PONV).
- Accurate mapping.
- Disadvantages:
- Risks of airway obstruction if sedation level is not titrated correctly, leading to hypercapnia, hypoxia, and increased intracranial pressure.
- Inadequate sedation can cause patient discomfort and anxiety.
Drug Selection Principles
- Maximize patient comfort.
- Prevent PONV to avoid increasing intracranial pressure.
- Maintain haemodynamic stability.
- Use short-acting drugs for acute control of the patient’s conscious level.
Comparison of Propofol-Remifentanil vs. Dexmedetomidine
- Propofol-Remifentanil:
- Target-controlled infusion (TCI) of propofol and remifentanil infusion (0.05–1 μg/kg/min).
- Reduce remifentanil to 0.005–0.01 μg/kg/min when tumor is exposed to allow return of spontaneous ventilation.
- Remove LMA and stop propofol once spontaneous ventilation returns.
- Re-anaesthetize and reinsert LMA post-resection until the end of the procedure.
- Dexmedetomidine:
- Loading dose of 0.5–1.0 μg/kg over 20 minutes.
- Followed by an infusion rate of 0.2–0.7 μg/kg/h depending on sedation level required.
Both techniques are acceptable and can be tailored to the patient’s needs and the duration of the procedure.
Theatre Layout
- Ensure communication with the patient is maintained.
- Maintain access to the patient during adverse incidents.
- Position the patient based on the lesion location, typically lateral or supine, or sitting for occipital lesions.
Scalp Block
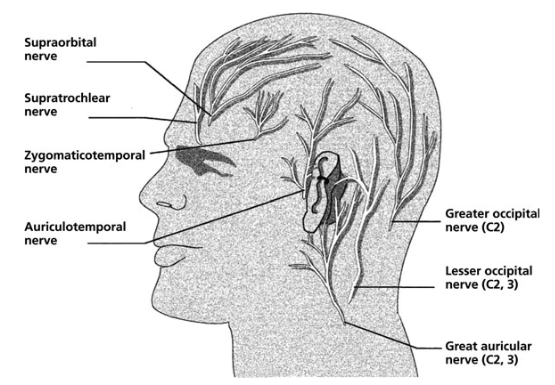
Overview
Scalp blocks are essential for providing analgesia during awake craniotomy. The following information outlines the key nerves targeted in a scalp block, the agents used, and the procedure for administering the block.
Local Anesthetic and Equipment
- Local Anesthetic: Bupivacaine 0.25% with 1:400,000 adrenaline.
- Needle: 22/23G needle.
- Technique: Aseptic.
Target Nerves and Injection Sites
Supraorbital Nerve (Trigeminal Nerve, V1 Distribution)
- Innervation: Forehead, anterior scalp, top part of the head.
- Injection Site: Palpate the supraorbital notch, insert the needle perpendicularly, and inject.
Supratrochlear Nerve (Trigeminal Nerve, V1 Distribution)
- Innervation: Forehead, anterior scalp.
- Injection Site: Just medial to the supraorbital nerve injection site, above the eyebrow line. Inject local anesthetic to spread the block medially.
Zygomaticotemporal Nerve (Trigeminal Nerve, V2 Distribution)
- Innervation: Small area of the forehead, temporal area.
- Injection Site: Infiltrate deep and superficial to the temporalis muscle. Start at the lateral edge of the supraorbital margin and continue to the distal aspect of the zygomatic arch.
Auriculotemporal Nerve (Trigeminal Nerve, V3 Distribution)
- Innervation: Temporal areas, lower lip, lower face, auricle, scalp above the auricle.
- Injection Site: Inject about 1 cm anterior to the auricle, above the level of the temporomandibular joint. Palpate the superficial temporal artery to avoid intra-arterial injection.
Lesser Occipital Nerve (Second or Third Cervical Spinal Nerve)
- Innervation: Lateral scalp area posterior to the auricle.
- Injection Site: Infiltrate subcutaneously behind the auricle, starting from the top down to the auricular lobule. Continue along the superior nuchal line to the greater occipital nerve.
Greater Occipital Nerve (Second Cervical Spinal Nerve)
- Innervation: Posterior scalp, top of the head, over the auricle.
- Injection Site: Palpate the occipital artery (3-4 cm lateral to the external occipital protuberance along the superior nuchal line) and inject medial to the artery.
Greater Auricular Nerve (Second and Third Cervical Spinal Nerves)
- Innervation: Skin over the parotid gland, mastoid process, auricle.
- Injection Site: Inject about 2 cm posterior to the auricle at the level of the tragus.
Adverse Events and Management
- Seizures: Occur during cortical mapping. Treated with ice-cold saline irrigation. If persistent, use benzodiazepines, anti-epileptic drugs, or re-sedation with airway control.
- Patient Intolerance: Often due to urinary catheter, prolonged positioning, or intraoperative seizures.
- Airway Obstruction: If reintubation is required, the surgeon should declamp the head, cover the surgical site, and move the head to an appropriate intubating position. Ensure airway equipment is ready.
- Anxiety/Agitation: Causes include pain, catheter, or temperature. Manage with reassurance and excellent preoperative counseling.
- Pain: Often due to catheter insertion or neck stiffness. Use local anesthetics for catheter insertion.
- Hypertension: Caused by pain or anxiety. Treat with remifentanil, dexmedetomidine, labetalol, esmolol, or verapamil.
- Nausea and Bradycardia: Associated with deep cortical resections near the midline. Anticholinergics are more effective than antiemetics.
- Brain Edema: Due to hypercapnia. Ask the patient to hyperventilate or use mannitol.
Monitoring Cerebral Perfusion
- Awake Patient:
- Transcranial Doppler: Detects cerebral emboli, reduced middle cerebral artery velocity (<25 cm/sec or reduction by 50% is significant).
- NIRS: A 20% drop in reading indicates increased risk of stroke.
- EEG Processing: Strong correlation with cerebral ischaemia; EEG becomes isoelectric before irreversible damage.
- Somatosensory Evoked Potentials: A >50% decrease is significant.
- Carotid Stump Pressure Measurement: (Old technique, <40 mmHg is significant).
- Changes in monitoring can indicate the need for augmenting BP, supplemental oxygen, and shunt placement (if not already present).
Mapping Options
- Speech and Language Mapping: Naming objects, counting, reading, repeating complex sentences.
- Motor Mapping: Involuntary movements and difficulty with motor tasks.
- Sensory Mapping: Ask the patient to report abnormal sensations.
- Visual Mapping: Abnormal visual phenomena or visual field defects.
Note: Sensory and motor mapping can be done via SSEPs and MEPs, but speech, language, and visual mapping cannot.
Craniotomy
Considerations
Common Procedures
- Traumatic brain injury (TBI)
- Intracranial tumors
- Brain neurovascular surgery
Key Points
- Limited airway access during the procedure.
- Need to manage increased intracranial pressure (ICP) and optimize surgical exposure.
Intraoperative Fluid Management
- Fluid and electrolyte balance is significantly affected by diuretics used to decrease ICP and facilitate intracranial dissection.
Maintenance of Cerebral Perfusion Pressure (CPP)
- Cardiac rhythm disturbances, including asystole and bradycardia, can occur due to parasympathetic stimulation, ICP-mediated vagus nerve stimulation, or trigeminal cardiac reflex (TCR).
- Retractor pressure and clipping/flow interruptions can impact CPP.
Perioperative Blood Loss
- Blood loss can lead to intraoperative coagulopathy and anemia, which are particularly dangerous in neuroanesthesia.
Neuromonitoring
- Essential for monitoring brain function during surgery.
Emergence
- Smooth and controlled emergence is necessary for postoperative neurological assessment.
Complications
- Venous air embolism
- Hemorrhage
- Arrhythmias and hemodynamic instability
Predicting Intraoperative Arterial Hypotension
- Multiple brain lesions and the presence/thickness of hemorrhage on a CT scan can predict intraoperative arterial hypotension.
Goals
Cerebral Protection
- Minimize increased ICP.
- Maintain CPP.
- Neuroprotection strategies, including temperature management and barbiturates.
Facilitation of Postoperative Neurological Evaluation
- Minimize the use of long-acting sedatives.
- Ensure clear and accurate intraoperative neurological monitoring.
Anaesthetic Technique
Induction
- Propofol: 2–3 mg/kg combined with remifentanil (0.2–0.5 μg/kg/min).
- Alternative to remifentanil: Fentanyl 5 μg/kg at induction, followed by top-up doses or an alfentanil infusion (25–50 μg/kg/hr).
- Consider lidocaine 1.5 mg/kg or a β-blocker (labetalol 5 mg increments) to blunt response.
- Administer IV induction agents slowly to avoid reducing BP and CPP.
- Use a non-depolarizing muscle relaxant to facilitate intubation.
- Use an armoured endotracheal tube (ETT) to prevent kinking, secured with tapes to avoid venous obstruction.
- Protect the eyes during the procedure.
Maintenance
- Avoid nitrous oxide (N2O).
- Maintain anesthesia with either a volatile agent (sevoflurane/isoflurane <1 MAC) or target-controlled infusion (TCI) of propofol (3–6 μg/mL).
- Continue remifentanil infusion at a lower rate (0.15–0.25 μg/kg/min).
- Aim for a PaCO2 of 4.0–4.5 kPa.
- Avoid extreme neck flexion or rotation to prevent impairment of cerebral venous return; maintain a head-up tilt.
- Support the shoulder if the head is turned to reduce neck vein compression.
Specific Considerations
- Application of the Mayfield 3-point fixator can cause a hypertensive response.
- Pin sites can be infiltrated with local anesthetic.
- If necessary, administer additional remifentanil (0.5–1 μg/kg) or propofol (0.5–1 mg/kg).
Links
Past Exam Questions
Awake Craniotomy Techniques
a) List the advantages and disadvantages of performing an awake craniotomy under:
- Sedation-only technique. (4) – General anaesthesia with wake-up technique. (4)
b) Write down the loading dose and infusion regimen range when using dexmedetomidine as a single sedation agent for awake craniotomy. (2)
Awake Craniotomy
a) What are the absolute contraindications to awake craniotomy? (5)
b) What nerves need to be blocked to provide analgesia for a scalp block? (3)
c) What are the potential complications of a scalp block? (2)
References:
- Burnand, C. and Sebastian, J. (2014). Anaesthesia for awake craniotomy. Continuing Education in Anaesthesia Critical Care &Amp; Pain, 14(1), 6-11. https://doi.org/10.1093/bjaceaccp/mkt024
- Bilotta, Federico; Guerra, Carolina; Rosa, Giovanni. Update on anesthesia for craniotomy. Current Opinion in Anaesthesiology 26(5):p 517-522, October 2013. | DOI: 10.1097/01.aco.0000432513.92822.c2
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries:
Awake craniotomy
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “0687edca-0ca9-4816-9477-f7c51d410252”



