{}
Compartment Syndrome
General
- Fascial membranes in the human body surround muscle groups.
- Compartment syndrome (CS): Increased pressure in fascial compartments compromises circulation and function of tissue within these compartments.
- Positive feedback: ischemia → necrosis → edema → further increase in compartment pressure.
- Epidemiology:
- Most commonly occurs after trauma, especially long bone fractures.
- Incidence: 7.3/100k in men and 0.7/100k in women.
- Common sites: fibular and extensor compartments in the lower leg, extensor compartment in the forearm.
Definition
- CS is a condition where increased pressure within a closed compartment compromises the circulation and function of tissues within that space.
- Acute limb CS: Acutely raised pressures in an osseofascial compartment of a limb, most commonly seen in the calf or forearm, occasionally in the upper arm, thigh, buttock, foot, or hand.
- Other clinically relevant compartments include the cranium, eye, spinal column, abdomen, chest, and pericardium.
Aetiology
- Commonest cause: Trauma, usually after a fracture, in male patients less than 35 years old.
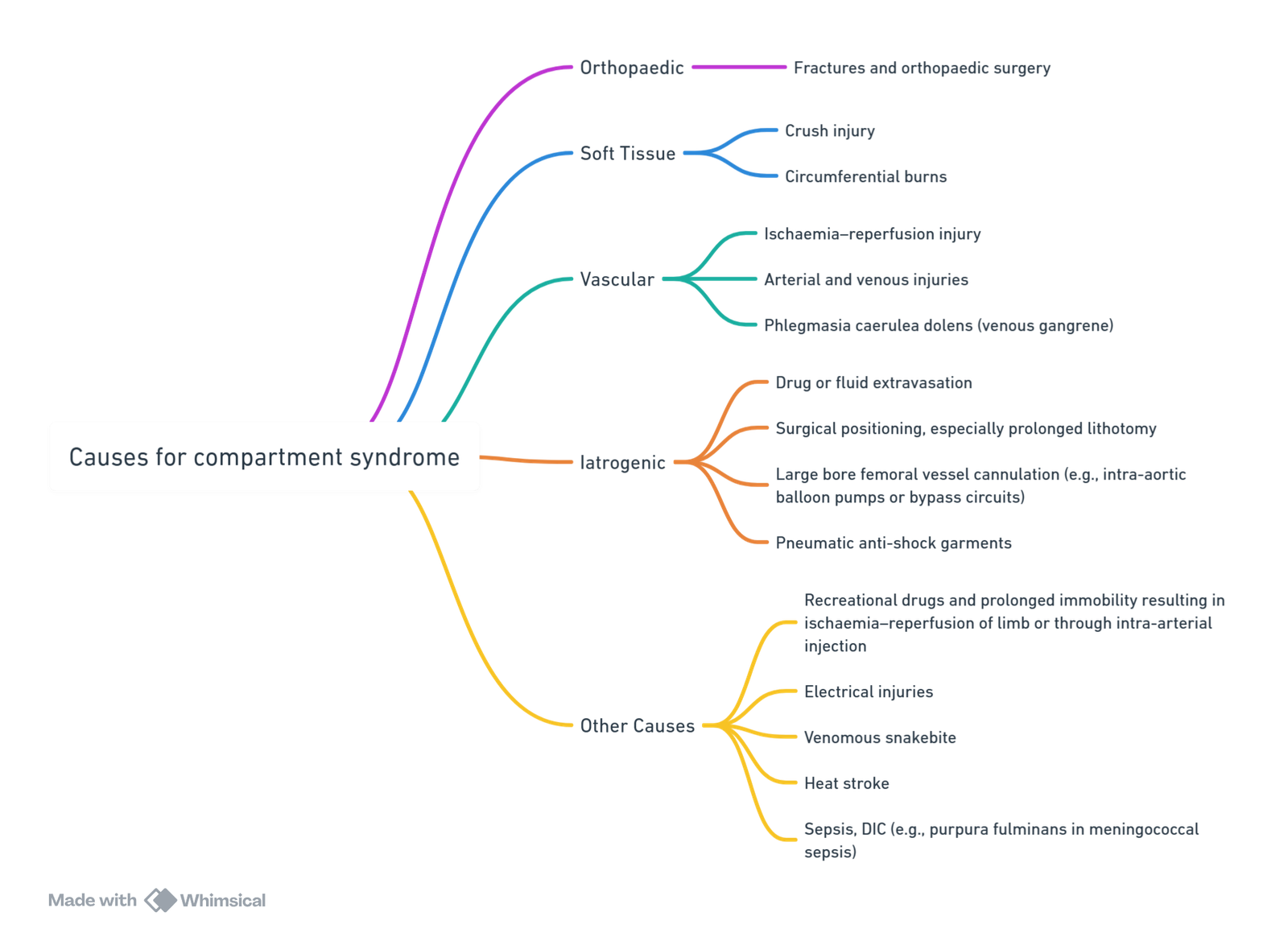
View or edit this diagram in Whimsical.
Pathophysiology
- Muscles, nerves, and blood vessels lie within fascial compartments.
- After direct injury, ischaemia–reperfusion, or fluid extravasation, the pressure within these compartments may rise, reducing perfusion and leading to local ischaemia of muscles and nerves.
- Ischaemia results in tissue membrane damage and fluid leakage, increasing tissue pressure.
- Raised tissue pressure causes venous outflow obstruction and increased venular pressure.
- Increased capillary pressure induces a cycle of fluid transudation, swelling, and rising intracompartmental pressure.
- If intracompartmental pressure approaches capillary pressure, microcirculatory perfusion ceases, leading to tissue infarction unless pressure is relieved.
- Reperfusion can continue tissue damage initiated in the ischaemic phase.
- Without relief within a few hours, irreversible changes occur with muscle necrosis, contracture, and nerve and vessel damage.
- Irreversible injury in the leg may occur as early as 4 hours after injury onset.
Risk Factors
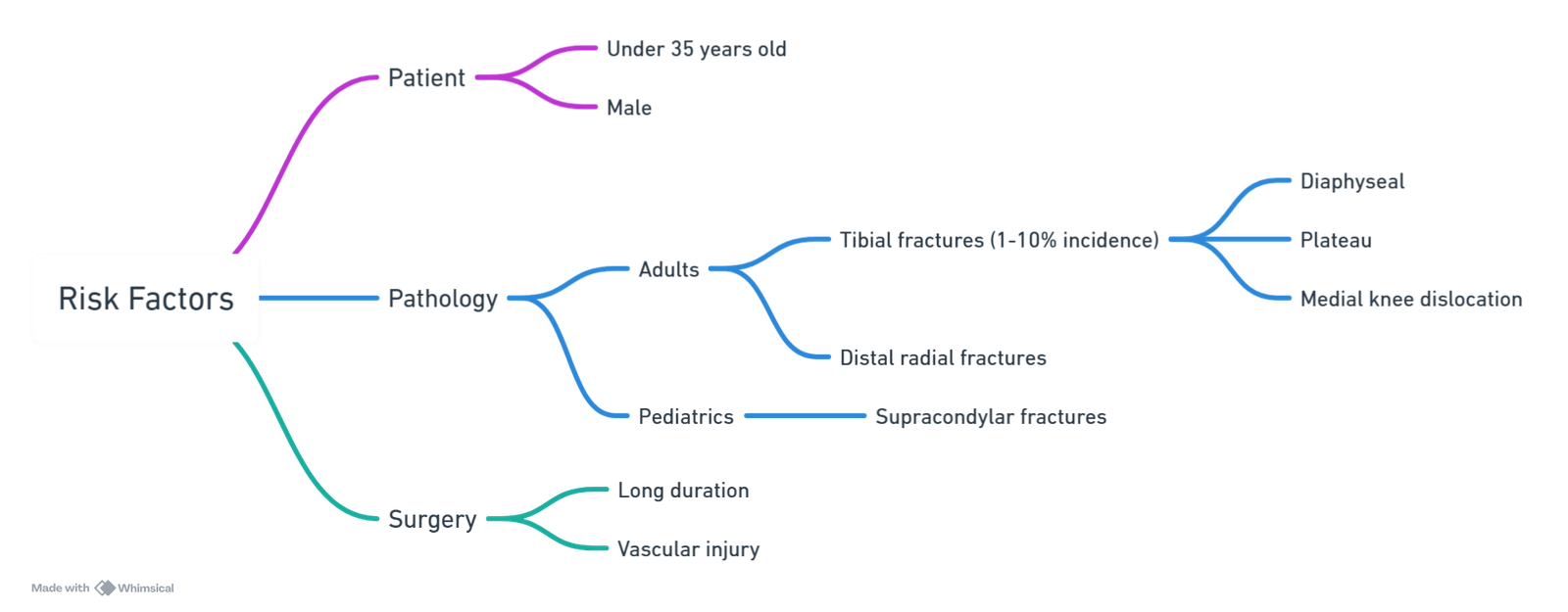
View or edit this diagram in Whimsical.
Prevention
- Limb ischaemia prevention by restricting elevated leg time in lithotomy position, or tourniquet release.
- Lower legs from lithotomy and deflate tourniquet intermittently (every 2–3 hours).
- Careful patient positioning and avoidance of perioperative hypotension can reduce CS risk.
Diagnosis
ACS Definition
- Elevated pressure within a compartment leads to impaired circulation and tissue function.
Diagnostic Indicators
- Pain with passive stretch
- Pain out of proportion
- Increasing analgesic requirement
- Tenderness/firmness
- Sensory loss
- Motor weakness
Pressure Measurements
- Absolute Pressure (P)
- Delta Pressure (ΔP): ΔP = Diastolic Pressure (DP) – Compartment Pressure (CP)
- Severe pain over the affected compartment, often disproportionate to the apparent injury, is the cardinal symptom of a CS.
- Aggravated by passive stretching of involved muscles.
- Paraesthesia, especially loss of two-point discrimination in the nerves traversing the compartment, is characteristic.
- 3 P’s (low sensitivity, high specificity):
- Pain – main clinical sign, classically “out of proportion” to injury
- Paresthesia – late clinical sign
- Paresis – even later clinical sign
Diagnosis
- Clinical signs/symptoms (3 P’s)
- Measure compartment pressure, where normal compartment pressure ~8 mmHg
- Calculate Critical Δ Tissue pressure = Diastolic BP – compartment pressure
- more than 30 mmHg = normal
- <30 mmHg = indication for fasciotomy (100% sensitivity and specificity)
Common Causes for Diagnostic Confusion
Patient-related
- Extremes of age
- Acute confusional state
- Spinal cord injury
- Multiple injuries
- Drug or alcohol overdose
Critical Care-related
- Sedation/analgesia
Anaesthetic-related
- Recovery from general anaesthesia
- Regional anaesthesia
- Analgesia (e.g., PCA)
Pressure Monitoring
- Diagnosis is usually clinical, though compartmental pressure monitoring is recommended for high-risk patients.
- Normal muscle compartment pressure (absolute): >10–12 mmHg.
- Diagnosis and fasciotomy are required if compartmental perfusion pressure (delta) <30 mmHg.
Treatment
- Urgent Treatment: Surgical decompression is the mainstay of therapy.
- Goals: Decrease tissue pressure, restore blood flow, minimize tissue damage and functional loss.
- Keep the limb at heart level; avoid elevation to prevent critical perfusion decrease.
- Monitor for systemic effects of massive rhabdomyolysis: hyperkalemia, myoglobinuria, acute renal failure, and systemic inflammatory response syndrome with cardiovascular and respiratory failure.
- Achieve adequate pain control with the lowest possible dose to avoid delayed CS diagnosis.
- Sudden pain increase should be considered CS until proven otherwise.
- Avoid epidurals in high-risk patients to prevent delayed CS diagnosis; if used, employ low-concentration solutions.
- Peripheral regional anesthesia is safe and does not delay CS diagnosis; use dilute concentrations and minimal adequate dose.
- Liberal indication for fasciotomy.
Links
References:
- Farrow, C., Bodenham, A., & Troxler, M. (2011). Acute limb compartment syndromes. Continuing Education in Anaesthesia Critical Care &Amp; Pain, 11(1), 24-28. https://doi.org/10.1093/bjaceaccp/mkq041
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “52395ba8-890e-48c8-884e-403865bb903e”



