- Transurethral Resection of Bladder Tumour (TURBT)
- Open Simple Prostatectomy & Radical Prostatectomy
- Nephrectomy (Partial & Radical)
{}
Transurethral Resection of Bladder Tumour (TURBT)
| Aspect | Key points (2025 update) |
|---|---|
| Surgical details | Endoscopic monopolar or bipolar diathermy under glycine (1.5 %) or normal saline irrigation; duration 10–45 min; lithotomy. |
| Anaesthetic technique | – Regional: Low-dose spinal (hyperbaric bupivacaine 6–8 mg ± opioid) plus ultrasound-guided obturator nerve block (inguinal or inter-adductor approach) to prevent obturator jerk. – General: LMA or ETT with short-acting neuromuscular blockade if ONB unavailable or tumour on lateral wall. – Avoid deep Trendelenburg to curb venous oozing. |
| Pre-operative focus | – Strong association with cigarette smoking ⇒ assess cardiopulmonary comorbidity. – Check Hb, coagulation, eGFR. – Stop anticoagulants/antiplatelets per guideline; bridge if high thrombotic risk. |
| Intra-operative priorities | – Obturator spasm: ONB more effective than lowering diathermy current and reduces recurrence in lateral-wall tumours. – Antibiotic prophylaxis: single-dose cefazolin 2 g IV (or weight-based alternative) at induction. – Continuous fluid irrigation; monitor for bladder perforation ( ↓return flow, shoulder pain, abdominal distension). |
| Post-operative care | – Continuous bladder irrigation until effluent is clear. – Analgesia: paracetamol + NSAID (if eGFR > 60 mL min⁻¹), rescue oral oxycodone or tramadol. – Warn ward staff about intravesical mitomycin C instillation within 6 h (contra-indicated if perforation suspected). – Discharge often same-day. |
Open Simple Prostatectomy & Radical Prostatectomy
| Simple (Benign) | Radical (Malignant–open, laparoscopic, or robotic-assisted (RALP)) |
|---|---|
| Patient profile: Elderly with LUTS, co‐morbid. | Fitter, often < 70 y; consider neo-adjuvant ADT. |
| Surgical time: 1–2 h. | Open 2–3 h; RALP 2–3 h (steep Trendelenburg, pneumoperitoneum ≥ 15 mm Hg). |
| Blood loss: 300–1000 mL (open). | Open 500–2000 mL; RALP < 300 mL on average. Cell salvage & low-dose tranexamic acid 1 g reduce transfusion. |
| Lines/monitoring | Large-bore IV, arterial line if cardiac disease or RALP (CO₂ insufflation + head-down ↑ after-load). |
| Anaesthesia | GA + ETT; consider balanced opioid/volatile or TIVA with remifentanil. Avoid excessive PEEP in RALP to maintain venous return. |
| Analgesia | Rectus sheath catheters (open) or bilateral TAP block (lap/robotic); IV PCA if blocks not used. |
| Complications | – Venous thrombo-embolism (VTE) risk high ⇒ LMWH + graduated stockings. – RALP: facial/laryngeal oedema from steep Trendelenburg; check leak before extubation. – Air embolism rare but possible with open dorsal venous plexus. |
Nephrectomy (Partial & Radical)
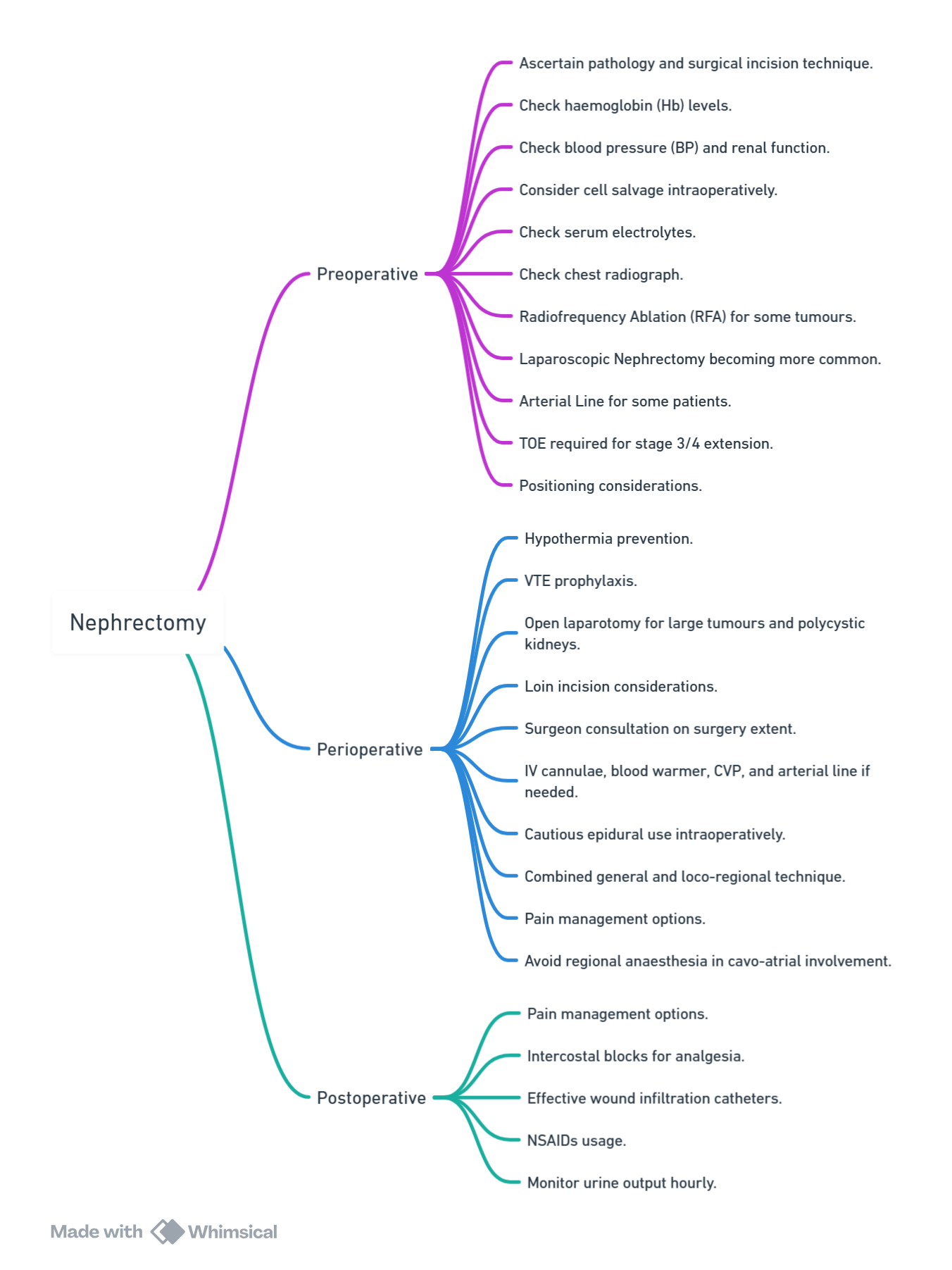
View or edit this diagram in Whimsical.
Pre-operative Optimisation
| Consideration | Details |
|---|---|
| Pathology | RCC ≈ 90 % of solid renal masses. Up-to-25 % have venous/atrial tumour thrombus. |
| Labs | Full blood count (paraneoplastic anaemia), eGFR, electrolytes (paraneoplastic hyponatraemia), coagulation. |
| Imaging | CT/MRI to define thrombus extent (Novick Levels I–IV). TOE mandatory for Level III/IV. |
| Comorbidity | Smoking-related COPD, hypertension, obesity. Optimise BP and lung function. |
Anaesthetic Management
- Approach
- Minimally invasive (laparoscopic/robotic partial or radical) is now standard for T1–T2 tumours.
- Open/flank for > T3 tumours, caval involvement, or very large polycystic kidneys.
- Lines & monitoring
- Two large-bore IVs ± rapid infuser.
- Arterial line for expected blood loss > 500 mL or renal-vein/IVC thrombus.
- Central line when vasoactive support or CVP trending required.
- Blood conservation
- Antifibrinolytic: Tranexamic acid 15 mg kg⁻¹ at induction (safe in cancer surgery).
- Cell salvage acceptable; discard suction after tumour breach if concern for malignant cells.
- Fluid strategy
- Goal-directed therapy (stroke-volume variation or Oesophageal Doppler) reduces AKI and ileus.
- Maintain MAP > 65 mm Hg; brief permissive hypotension acceptable during venotomy.
- Renal protection _(evidence equivocal)
- Mannitol 0.5 g kg⁻¹ IV pre-clamp +/- furosemide 0.1 mg kg⁻¹ when unclamped in solitary-kidney or prolonged clamp > 30 min.
- Analgesia
- Thoracic epidural (T7–T10) remains gold standard for open flank; start low-dose local anaesthetic after haemostasis.
- Minimally invasive: ultrasound-guided erector spinae plane (ESP) or quadratus lumborum (QL) blocks as effective as epidural with fewer hypotension events.
- Regular paracetamol ± NSAID if eGFR > 45 mL min⁻¹.
- Enhanced Recovery
- Carbohydrate drink 2 h pre-op, early ambulation and oral intake within 24 h cut LOS by 1–2 days.
Cavo-atrial Tumour Thrombectomy
- Multispecialty (urology, vascular, cardiac) team.
- TOE throughout; sudden ↓ ETCO₂ or RV filling suggests embolus.
- Level IV cases may require hypothermic circulatory arrest on cardiopulmonary bypass; keep haemoglobin > 9 g dL⁻¹ for oxygen delivery.
Radical Cystectomy (± Urinary Diversion)
| Domain | Current best practice |
|---|---|
| Enhanced Recovery Pathway | Pre-habilitation, smoking cessation ≥ 4 weeks, carbohydrate loading, restricted fasting 2 h for clear fluids. |
| Anaesthesia | GA + ETT; low-dose remifentanil infusion for controlled hypotension (target MAP 60–65 mm Hg). Consider thoracic epidural (T8–L1) for open cases–start after vascular control. |
| Lines/Fluid | 2 × 14G cannulae, arterial line, ± central line/Oesophageal Doppler. Balanced crystalloids; avoid chloride load > 4 mEq kg⁻¹ to limit hyperchloraemic acidosis. |
| Blood management | Expect 700–3000 mL loss; cell salvage until bowel is opened; TXA 1 g at induction. |
| Temperature & VTE | Forced-air warming; LMWH within 6 h post-op and continue ≥ 28 d. |
| Analgesia | Dual rectus-sheath catheters with programmed intermittent bolus + IV PCA improves mobilisation and reduces ileus. |
| Post-operative goals | – Early removal of NGT (in theatre). – Clear fluids day 0, chew gum × 6 daily. – Target urine output > 0.5 mL kg⁻¹ h⁻¹ through conduit/neo-bladder; beware hidden leak (↑ drain creatinine). – Daily serum electrolytes; replace bicarbonate/potassium if hyperchloraemic metabolic acidosis develops. |
Selected Dermatomal Coverage for Regional Techniques
| Incision | Sensory levels required |
|---|---|
| Flank | T9–T11 |
| Thoraco-abdominal | T7–T12 |
| Trans-abdominal | T6–T10 |
Common Complications & Mitigation
| Timing | Complication | Prevention/Management |
|---|---|---|
| Immediate | Vascular or visceral injury, pneumothorax | Experienced surgical exposure; large-bore access & rapid infuser ready |
| Early | AKI, ileus, VTE, bleeding | Goal-directed fluids; early mobilisation; LMWH; check Hb & drain output |
| Late | CKD progression, incisional hernia, chronic pain | Renal follow-up, abdominal wall closure bundles, multimodal analgesia |
Links
- Urology
- Renal protection
- Renal Physiology
- Renal replacement therapy
- Anaesthesia and renal disease
- Robotic surgery
References:
- Allman K, Wilson I, O’Donnell A. Oxford Handbook of Anaesthesia. Vol. 4. Great Clarendon Street, Oxford, OX2 6DP, United Kingdom: Oxford University Press; 2016. Page 590-600.
- Butterworth J, Mackey D, Wasnick J. Morgan and Mikhail’s Clinical Anesthesiology, 7th Edition. 7th edition. New York: McGraw Hill Medical; 2022.elect/library/items/UWTJV8UG)
- Chapman, E. and Pichel, A. (2016). Anaesthesia for nephrectomy. BJA Education, 16(3), 98-101. https://doi.org/10.1093/bjaceaccp/mkv022
- European Association of Urology. EAU Guidelines on Non-muscle-invasive Bladder Cancer. Limited update 2025.
- Karadeniz M, et al. Effect of obturator nerve blockade on outcomes of lateral-wall NMIBC resection. J Urol Surg. 2023. jurolsurgery.org
- Mao W, et al. Regional block plus spinal reduces recurrence after TURBT. Urol Oncol. 2024. [pmc.ncbi.nlm.nih.gov](https://pmc.ncbi.nlm.nih.gov/articles/PMC11917164/?utm_source=chatgpt.com
- ERAS® Society. Guidelines for urological surgery–Radical Cystectomy. 2024 update. pmc.ncbi.nlm.nih.gov
- Deng L, et al. ERAS protocol in laparoscopic radical nephrectomy improves outcomes: systematic review. Front Surg. 2023. pmc.ncbi.nlm.nih.gov
- Wang Y, et al. Enhanced recovery after surgery in partial nephrectomy: meta-analysis. Asian J Urol. 2023.
- Zhang X, et al. Thoracolumbar paravertebral block for renal surgery reduces opioid consumption. Pain Res Manag. 2023. pmc.ncbi.nlm.nih.gov
- National Institute for Health & Care Excellence. Cell Salvage in Major Surgery. NICE IPG 2021 update. bjanaesthesia.org
- Sessler DI, et al. Cumulative hypotension and organ injury: BJA prospective cohort. Br J Anaesth. 2025. bjanaesthesia.org
- European Association of Urology. EAU Guidelines on Urological Infections. 2025. d56bochluxqnz.cloudfront.net
Summaries
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “3f104806-bfc7-4c18-bc31-e8b6a24268a0”



