{}
Checklist
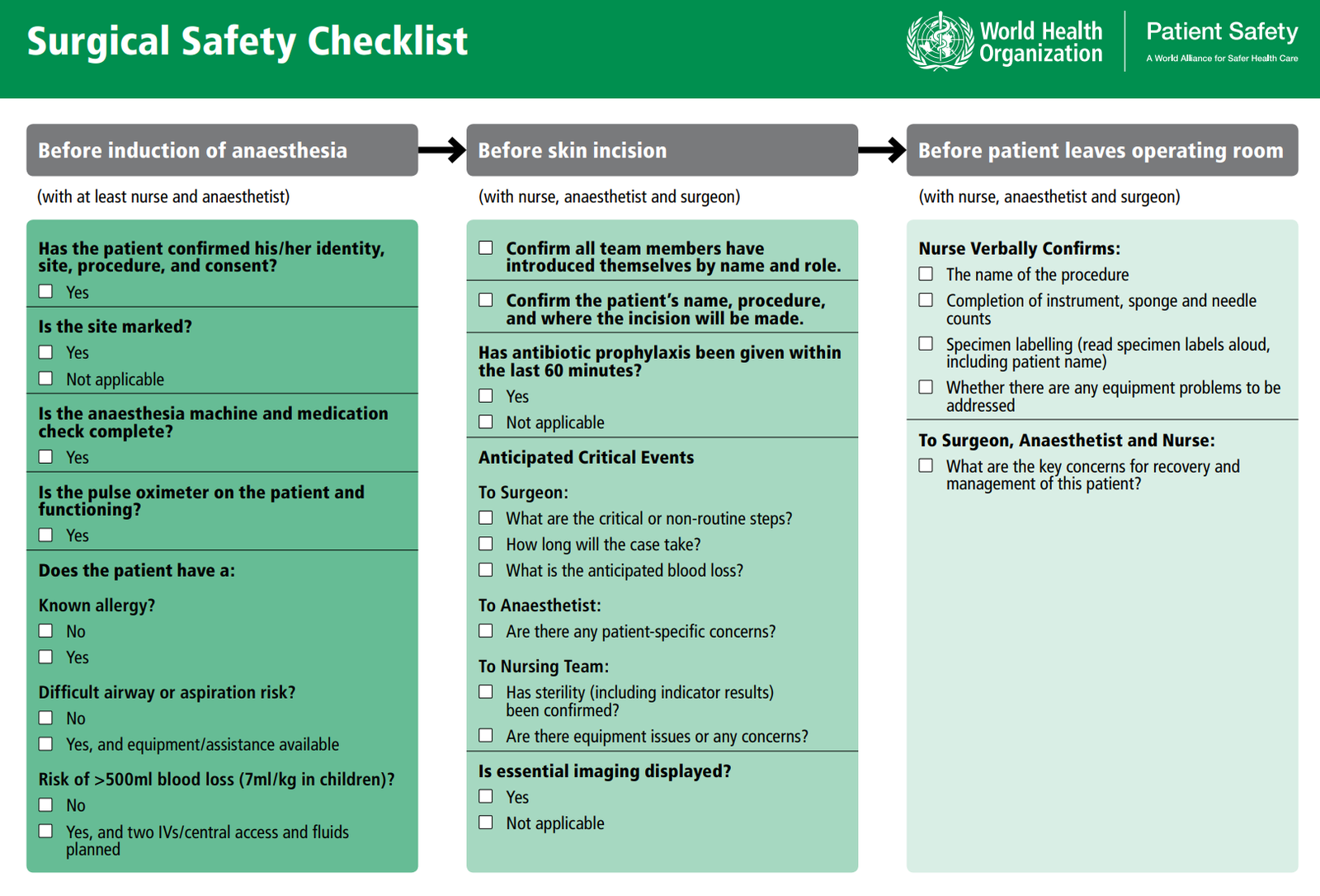
Surgical Safety Checklist Stages
1. Sign-In
Before administration of anaesthesia
- Confirm patient identity, surgical site, procedure, and consent
- Ensure the site is marked
- Complete anaesthesia machine and medication check
- Ensure pulse oximeter is on the patient and functioning
- Check for known allergies, difficult airway or aspiration risk, and risk of significant blood loss
2. Time-Out
Immediately before the surgical incision
- Confirm all team members have introduced themselves by name and role
- Verify the patient’s name, procedure, and incision site
- Ensure antibiotic prophylaxis has been given within the last 60 minutes
- Review anticipated critical events:
- Surgeon: critical/non-routine steps, case duration, anticipated blood loss
- Anaesthetist: patient-specific concerns
- Nursing team: sterility confirmation, equipment issues
- Ensure essential imaging is displayed
3. Sign-Out
At the end of operation before the patient is removed from the operating theatre
- Nurse verbally confirms:
- Procedure name
- Completion of instrument, sponge, and needle counts
- Specimen labelling
- Any equipment problems to address
- Discuss key concerns for recovery and management of the patient
Expanded 5-Step Process
-
Briefing
- Team introductions
- Introduction of each patient on the list
- Discussion of any concerns
-
Sign-In
- Before induction of anaesthesia
- Confirmation of patient identity, procedure, and consent
-
Time-Out
- Pause and final check before surgery starts
-
Sign-Out
- Before all staff leave the theatre
- Verification of swab count and equipment
-
Debriefing
- At the end of the list
- Discussion and reporting of issues
Benefits of the Surgical Safety Checklist (SSC)
- Improves safety and reduces harm from potential errors
- Ensures confirmation of patient identity, surgical site, and important characteristics
- Significant reductions in:
- Complications (from 11% to 7%)
- In-hospital mortality (from 1.5% to 0.8%)
- Rates of unplanned reoperation
- Surgical site infections (SSI)
Implementation
Organizational Factors
Leaders / Local Champions
- Engage administrative staff
- Support juniors
- Provide reasons to engage
Resources
- Conduct audits
- Provide feedback
Data Collection
- Track antibiotics administration before knife-to-skin
- Ensure checklist completion
- Collect audit samples
- Provide regular feedback
Documentation
- Record in patient notes or computer system
Training
- Form an implementation team
- Ensure multidisciplinary involvement
- Provide focused training for new practices
Communication
- Use names
- Ensure everyone is listening
Briefing and Debriefing
Requirements for Successful Implementation
- Training and learning materials
- Organizational priority and leadership
- Checklist as a clinical governance goal
- Local champions and discussion groups/forums
- Clarify roles of each professional group
- Conduct regular audits and feedback sessions
- Support local measurement of effectiveness
- Encourage local adaptations
- Create evidence of success in improving patient safety
Barriers to Checklist Implementation
Pragmatic Challenges
- Duplication with existing checklists causing irritation and ‘checklist fatigue’
- Time-consuming and inconvenient processes
- Inappropriate timing
- Poor communication
- Unfamiliarity and confusion about who should prompt items
- Absence of key team members
- Perception of checklist as a ‘tick box exercise’
Resources
- Lack of resources such as marker pens, antibiotics, and pulse oximeters
Attitudes
- Denial that routine tasks can be forgotten
- Dismissive attitudes and lack of engagement
- Hierarchical structures discouraging open communication
- Embarrassment about introductions
- Lack of support from leaders or managers
Underlying Processes of Care
- Lack of antibiotic policies and protocols
- No routine swab, needle, or instrument counts
WHO 10 Essential Steps
- Operate on the correct patient at the correct site
- Use methods to prevent harm from anaesthetics and protect from pain
- Recognize and prepare for life-threatening loss of airway or respiratory function
- Prepare for risk of high blood loss
- Avoid inducing allergic or adverse drug reactions
- Minimize risk of surgical site infection
- Prevent inadvertent retention of instruments and sponges
- Secure and accurately identify all surgical specimens
- Communicate and exchange critical information for safe operation conduct
- Establish routine surveillance of surgical capacity, volume, and results
Links
- Morbidity and mortality in Anaesthesia
- Infection control
- Practice guideline
- Practice management
- Risk
Past Exam Questions
Practical Challenges in Implementing the WHO Checklist
A single scrub sister was assigned to scrub for an orthopaedic list with 8 patients booked on the slate. The last patient of the day presented for an ankle procedure. The patient received a general anaesthetic followed by a left popliteal block. A tourniquet was applied to the left leg. During the operation, the surgeon failed to find the bony deformity on the left-hand side and re-checked his notes in the bed letter. He then announced that it was not the left but actually the right ankle which required the operation.
What are the practical challenges in implementing the WHO checklist that could have prevented the above complication? (10)
References:
- Mahajan, R. (2011). The who surgical checklist. Best Practice &Amp; Research Clinical Anaesthesiology, 25(2), 161-168. https://doi.org/10.1016/j.bpa.2011.02.002
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
Summaries:
WHO checklist
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “e6333703-5d46-4fd1-bba2-3db0ba9a1660”



