{}
Pulmonary Aspiration in Anaesthesia
Definition
Inhalation of oro-pharyngeal or gastric contents into the larynx or distal airways. Consequences depend on volume and acidity/particulate load:
- Obstruction–solid matter occludes large airways → hypoxaemia.
- Chemical pneumonitis–sterile acidic fluid (pH < 2.5, volume > 0.3 mL kg⁻¹) produces an inflammatory alveolitis (Mendelson).
- Aspiration pneumonia–colonised secretions cause infective consolidation
≈ 50 % of anaesthesia-related airway deaths involve aspiration; one-fifth occur after extubation.
Pathophysiology
| Stage | Event | Clinical evolution |
|---|---|---|
| 0–2 h | Surfactant disruption, bronchial oedema, neutrophil influx | Cough, wheeze, SpO₂↓; CXR often normal |
| 2–24 h | Cytokine-mediated capillary leak | Patchy basal infiltrates, refractory hypoxaemia |
| >24 h | Secondary bacterial overgrowth | Fever, purulent sputum, lobar consolidation |
Anatomy & Physiology of Anti-reflux Barriers
- Lower oesophageal sphincter (LOS)–resting tone 10–26 mm Hg; agents ↓ tone: propofol, opioids, volatile anaesthetics, anticholinergics, pregnancy progesterone.
- Upper oesophageal sphincter (UOS)–cricopharyngeus; ketamine uniquely preserves tone.
- Protective reflexes–cough, swallow, laryngospasm; blunted by sedatives, old age and diabetes.
Risk Factors
| Patient | Surgery | Anaesthetic |
|---|---|---|
| Full stomach, delayed emptying (trauma, opioids, diabetes, CKD, pregnancy), obesity, Gourd/hiatus hernia, neuro-disease, bowel obstruction | Upper GI, laparoscopy, lithotomy/Trendelenburg, emergency | Difficult/ prolonged airway, light anaesthesia, positive-pressure via SGA, first-generation SGA, surgery > 2 h |
Risk-reduction Bundle
| Goal | Measure & timing | Evidence (2020–2025) |
|---|---|---|
| ↓ gastric volume | Standard fasting (6-2-1 h); point-of-care gastric ultrasound if uncertain | ERAS consensus 2022 |
| ↑ emptying & LOS tone | Metoclopramide 10 mg IV 30 min pre-induction | Cochrane 2024: ↑ antral motility, no outcome harm |
| ↑ gastric pH | Ranitidine 150 mg PO night ± 2 h pre-op or PPI 20 mg PO night before | SIGN guideline 2023 |
| Airway protection | RSI with properly applied cricoid (30 N awake, 40 N asleep); 2nd-generation SGA when intubation not indicated | DAS 2022 RSI guideline |
| Extubation | Fully awake, head-up; suction pharynx; lateral or semi-upright positioning | NAP4 recommendations |
Management Algorithm
Suspected aspiration during GA
- Call for help. Stop surgery if possible.
- Airway–suction oropharynx; apply 100 % O₂.
- Intubate and before ventilation pass a large-bore catheter to suction trachea/bronchi; consider bronchoscopic lavage for particulate matter.
- Ventilate with lung-protective strategy (VT 6 mL kg⁻¹ PBW, PEEP 8–10 cm H₂O).
- Assess severity (within 2 h): persistent SpO₂ < 94 % on FiO₂ 0.5, A-a O₂ gradient > 300 mm Hg, bilateral infiltrates → ICU.
- Adjuncts–bronchodilators for wheeze, recruitment manoeuvres; no role for prophylactic steroids or antibiotics unless fever/leucocytosis > 6 h or radiological pneumonia.
- Consider ECMO for refractory hypoxaemia (PaO₂/FiO₂ < 80 mm Hg).
Elective list: postpone if major aspiration suspected.
Post-event Follow-up
| Finding at 2 h | Disposition | Notes |
|---|---|---|
| Normal sats, CXR and exam | Ward with 6 h obs | Provide patient information sheet |
| Any new sign (SpO₂↓, wheeze, infiltrate) | HDU/ICU | Serial gas & imaging 24 h |
Key Points
- Critical pH 2.5 & volume 0.3 mL kg⁻¹ (10 mL adult) derive from cat study; human data limited–still guide practice.
- Regurgitation is 3× more common than active vomiting during GA.
- 2nd-generation SGAs (e.g. i-gel, LMA Supreme) ↓ aspiration reports but do not replace tracheal tube in high-risk cases.
- Cricoid controversy: maintain unless airway soiled, then release to improve laryngoscopy/suction.
Rapid-Sequence Induction & Intubation (RSII)
- Key aim: secure the trachea quickly while minimising the risk of pulmonary aspiration and hypoxia.
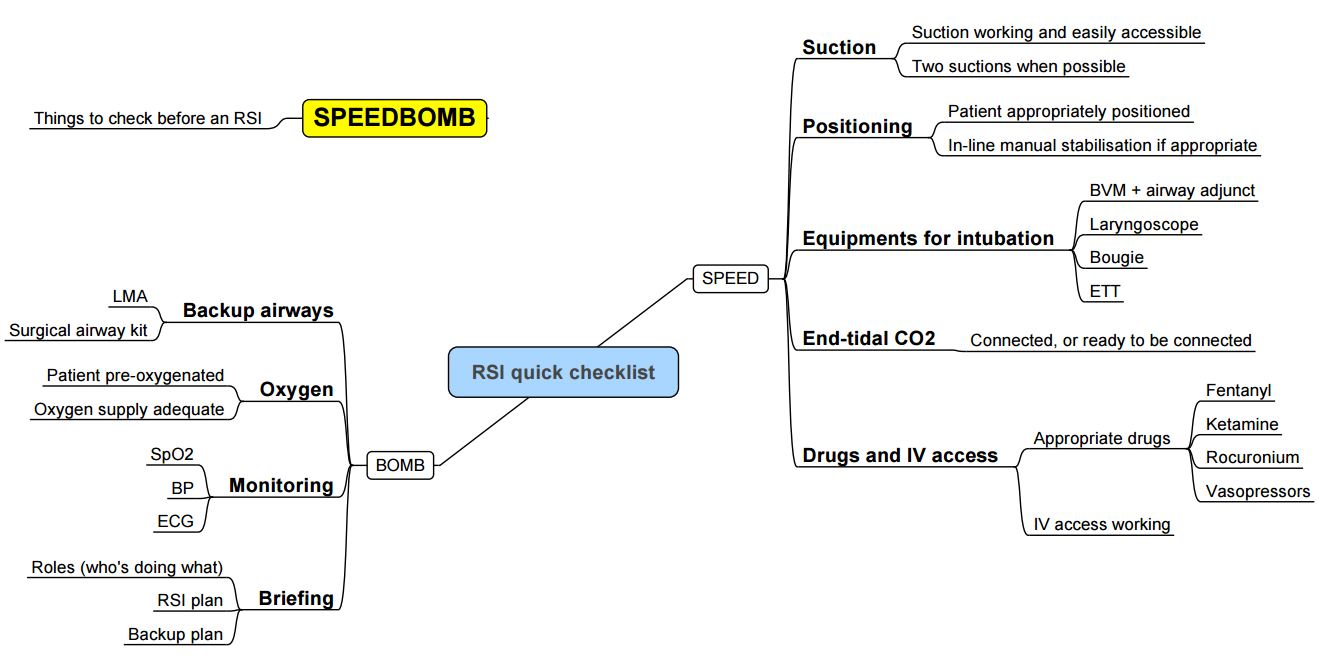
Contemporary RSII Workflow (“9 Ps”)
| Step | Actions & checkpoints |
|---|---|
| Plan | Define primary and rescue airway strategy; allocate roles; decide on use of cricoid pressure. |
| Prepare | Patient–optimise position (“head-up‐30°” if tolerated), ramp obese/gravida. Place–lights, suction each side, bed height at xiphisternum. People–brief assistant on cricoid, drug draw-up, checklist. |
| Protect C-spine | If trauma suspected; manual inline stabilisation until airway secured. |
| Position | Sniffing or ramp; pre-oxygenation FiO₂ 1.0 with tight mask or HFNO 50 L min⁻¹. |
| Pre-oxygenate | ≥ 3 min tidal breathing or 8 vital-capacity breaths; confirm EtO₂ > 0.9. |
| Pretreat (optional) | Fentanyl 1–2 µg kg⁻¹ to blunt sympathetic surge; lidocaine 1.5 mg kg⁻¹ for airway reactivity; atropine 20 µg kg⁻¹ IV in infants. |
| Paralyse & induce | Co-administer hypnotic (propofol 2 mg kg⁻¹ or ketamine 1–2 mg kg⁻¹) + neuromuscular blocker (succinylcholine 1–1.5 mg kg⁻¹ or rocuronium 1.0–1.2 mg kg⁻¹). Start apnoeic oxygenation via HFNO 15 L min⁻¹. |
| Place tube & prove | Videolaryngoscopy first-line; limit to ≤ 2 attempts. Verify with waveform capnography × 5 breaths, bilateral chest rise. |
| Post-intubation care | Secure tube, release cricoid, commence ventilation, check cuff pressure < 30 cm H₂O, set lung-protective parameters, redose analgesia and sedation. |
Drug Choices
| Class | Dose (adult) | Advantages | Caveats |
|---|---|---|---|
| Induction | Propofol 1.5–2 mg kg⁻¹ | Rapid, bronchodilator | Hypotension reduce 30 % in shock |
| Ketamine 1–2 mg kg⁻¹ | Maintains MAP/bronchodilates | ↑ secretion; give glycopyrrolate 0.2 mg | |
| Etomidate 0.3 mg kg⁻¹ | Cardiostable | Adrenocortical suppression–avoid septic shock | |
| NMB | Succinylcholine 1–1.5 mg kg⁻¹ | 45 s onset; 6 min offset | K⁺ rise, MH, bradycardia contraCK>1000, HD trauma > 48 h |
| Rocuronium 1 mg kg⁻¹ | 60 s onset; reversible with sugammadex 16 mg kg⁻¹ | Longer block if sugammadex unavailable |
Cricoid Pressure: 2022 DAS Consensus
- Application: 10 N awake → 30 N after LOC.
- Continue unless it impedes laryngoscopy, mask/SAD ventilation or suctioning.
- Abort if vomiting–risk of oesophageal rupture.
- Evidence: reduces gastric insufflation; clinical efficacy against aspiration unproven, but low harm if performed correctly.
Apnoeic Oxygenation & Gentle Ventilation
- Apnoeic oxygenation via nasal cannula (≥ 15 L min⁻¹) prolongs SpO₂ > 95 % by ~60 s in adults; HFNO 40–70 L min⁻¹ superior in obesity/paediatrics.
- “Modified RSII” permits gentle pressure-controlled ventilation (≤ 12 cm H₂O) after loss of reflexes to prevent desaturation in high-risk patients (obese, paediatric, pregnancy, critical hypoxaemia).
Paediatric RSII Highlights
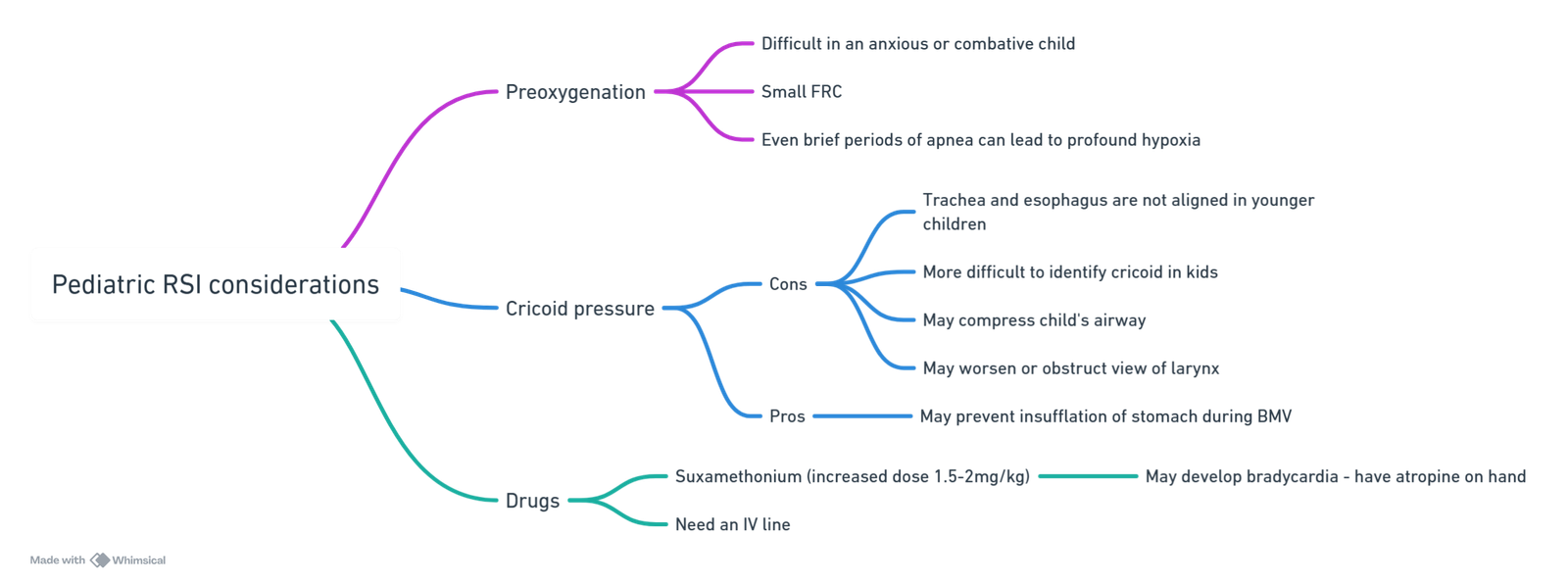
| Challenge | Adaptations |
|---|---|
| Short safe apnoea time | 3 min CPAP 5 cm H₂O + HFNO 2 L kg⁻¹ min⁻¹; allow gentle PSV. |
| Bradycardia with succinylcholine | Atropine 20 µg kg⁻¹ IV/IM pre-dose in < 1 yr. |
| Cricoid debate | Use < 10 N; abandon if worsens view/ventilation. |
| Drug doses | Propofol 3 mg kg⁻¹; ketamine 2 mg kg⁻¹; sux 2 mg kg⁻¹ IV (4 mg kg⁻¹ IM) or rocuronium 1.2 mg kg⁻¹. |
Difficult & Emergency Airway Considerations
- Employ Vortex or Also airway algorithm: 3 attempts rule (face-mask, SGA, ETT) before CICO pathway.
- Have front-of-neck access kit (scalpel-bougie-tube) immediately available.
- Pre-brief: lowest SpO₂ target (usually 90 %), maximum laryngoscopy attempts, cricoid release criteria.
Complications & Mitigation
| Complication | Prevention | Management |
|---|---|---|
| Hypoxaemia | Head-up, CPAP, HFNO, modified RSII | Stop attempt < 60 s; mask ventilate with PEEP |
| Hypotension | Fluid loading; ketamine/etomidate; vasopressor drawn up | Phenylephrine 100 µg bolus or Norad 5–10 µg |
| Aspiration | 6-2-1 fasting, antacid, cricoid | Suction, intubate, bronchial lavage, ICU |
| Failed intubation | Videolaryngoscope first; bougie ready | Follow DAS failed airway algorithm |
Links
- Aspiration
- Paediatric Induction and Rapid Sequence Induction (RSI)
- Airway guidelines
- Airway anatomy and assessment
References:
- Robinson, M. J. and Davidson, A. H. (2014). Aspiration under anaesthesia: risk assessment and decision-making. Continuing Education in Anaesthesia Critical Care &Amp; Pain, 14(4), 171-175. https://doi.org/10.1093/bjaceaccp/mkt053
- Nason KS. Acute Intraoperative Pulmonary Aspiration. Thorac Surg Clin. 2015 Aug;25(3):301-7. doi: 10.1016/j.thorsurg.2015.04.011. PMID: 26210926; PMCID: PMC4517287.
- Cook TM, et al. Airway complications and deaths due to aspiration: lessons from NAP4. Br J Anaesth. 2023;130:570-580.
- American Society of Anesthesiologists Task Force. Practice Guidelines for Preoperative Fasting & Pharmacologic Risk Reduction of Pulmonary Aspiration. 2022 update.
- Difficult Airway Society. Guidelines for Rapid Sequence Induction and Intubation. Anaesthesia 2022;77:915-932.
- Wong DT, et al. Apnoeic oxygenation during RSII: meta-analysis. Anesth Analg 2024;138:112-123.
- Litman RS. Paediatric rapid sequence induction: update 2023. Paediatr Anaesth 2023;33:1001-1012.
- Riva T, et al. Optimising cricoid pressure: ultrasound and manometry data. Anaesthesia 2024;79:150-159.
- Driver BE, et al. Gastric ultrasound for aspiration risk assessment: systematic review. Anesth Analg. 2024;138:112-123.
- Halliday S, et al. DAS guidelines for rapid sequence induction and intubation. Anaesthesia. 2022;77:915-922.
- Schmidt U, et al. Prokinetics in trauma patients: randomised trial. Crit Care. 2025;29:46.
- Steinmann D, et al. Antibiotics after aspiration pneumonitis? Pragmatic RCT. Lancet Respir Med. 2023;11:678-687.
- The Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- Image: Novice Anaesthesia. (2021). Infographics. Retrieved April 24, 2025, from https://www.gasnovice.com/infographics
Summaries:
RSI
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “7071f52f-23f2-4e89-b37f-0137117fc635”



