{}
Pulmonary Edema
Basic Mechanism and Classification
- Definition: Pulmonary edema is the accumulation of fluid in the lung interstitium and alveoli, caused by leakage of intravascular fluid.
- Types:
- Hydrostatic (Cardiogenic) Pulmonary Edema:
- Cause: Increased capillary pressure due to elevated hydrostatic forces.
- Mechanism: Commonly occurs due to left ventricular failure, leading to increased pulmonary venous pressure and fluid translocation into the alveoli.
- Increased Capillary Permeability (Non-Cardiogenic) Pulmonary Edema:
- Cause: Increased permeability of the pulmonary capillaries.
- Mechanism: Often a result of direct injury to the alveolar-capillary membrane from factors such as infections, inhaled toxins, or systemic inflammatory responses.
- Pulmonary Vasoconstriction:
- Mechanism: Increases capillary pressure, leading to fluid translocation into the alveoli.
- Examples:
- Neurogenic: Can occur following acute brain injuries.
- Drugs: Certain substances like cocaine can induce vasoconstriction and subsequent pulmonary oedema.
- Hydrostatic (Cardiogenic) Pulmonary Edema:
How to Get Pulmonary Oedema
| Increased Capillary Permeability | Increased Hydrostatic Pressure | Decreased Plasma Protein | Decreased Interstitial Pressure | Lymphatic Obstructions |
|---|---|---|---|---|
| Oxygen toxicity | Increased LA pressure (mitral stenosis, or myocardial infarction) | Protein starvation | Unknown origin | Tumors |
| Inhaled toxins | Excess IV fluids | Excess IV fluids | Too rapid evacuation of pneumothorax or hemothorax | Interstitial fibrotic diseases |
| Circulating toxins | Renal injury | High altitude | ||
| ARDS | Neurogenic (head injury) | |||
| Drug overdose |
Anaesthesia Considerations for Pulmonary Oedema
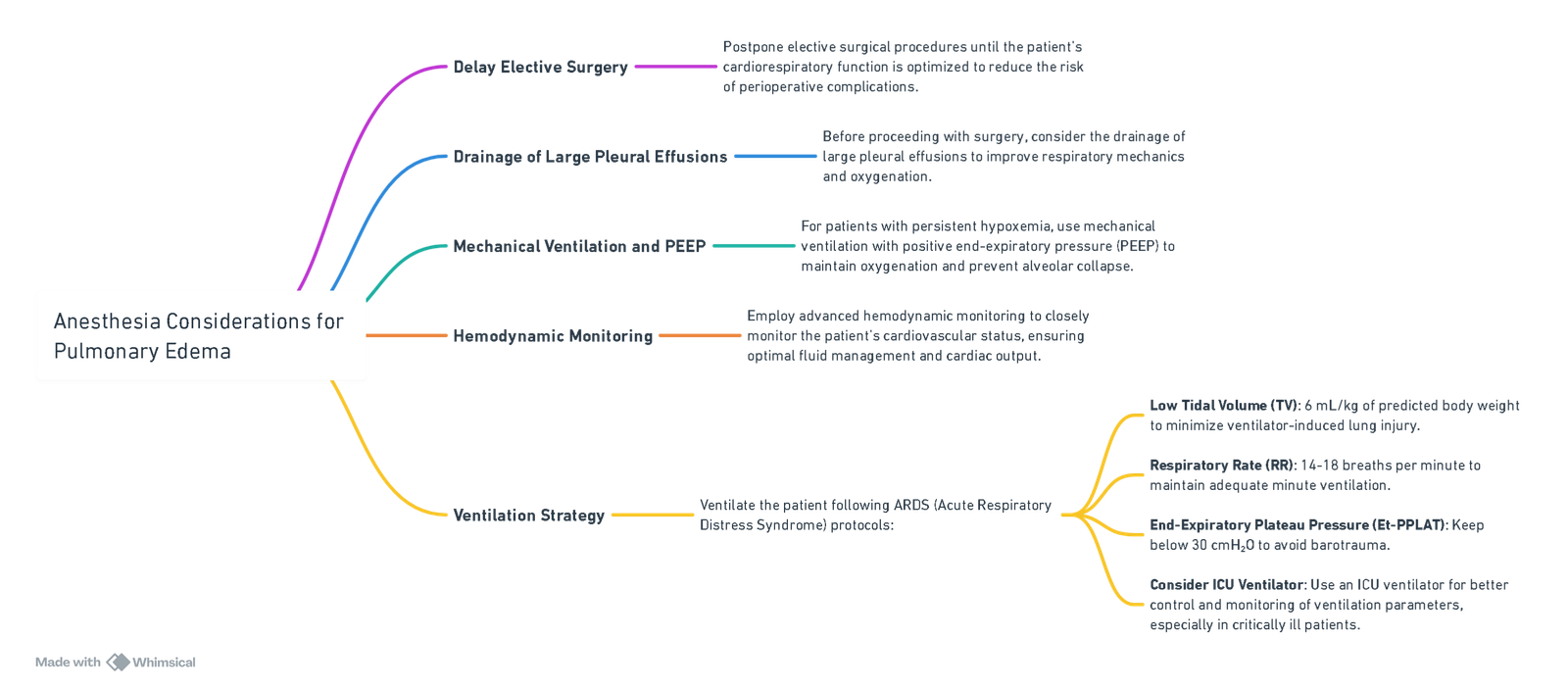
View or edit this diagram in Whimsical.
CXR Features
- Cardiomegaly
- Cardiothoracic Ratio (CTR) = 18/30 (>50%)
- Upper Zone Vessel Enlargement
- Sign of pulmonary venous hypertension
- Septal (Kerley B) Lines
- Sign of interstitial oedema
- Airspace Shadowing
- Due to alveolar oedema, acutely in a peri-hilar (bat’s wing) distribution
- Blunt Costophrenic Angles
- Due to pleural effusions
Cardiogenic Pulmonary Edema
Pathophysiology
- Acutely reduced forward flow and subsequent neurohumoral activation augment LAP; pulmonary capillary engorgement promotes alveolar haemorrhage and oedema
Understanding the Ventricular Pressure-Volume Loops in Normal and Pathological Conditions
Key Points
-
End-Systolic Elastance (Ees):
- Steeper slope indicates higher contractility.
- Depressed ventricular contractility leads to a reduced Ees, and thus, a reduced stroke volume.
-
Effective Arterial Elastance (Ea):
- Represents the arterial load the ventricle must overcome to eject blood.
- Increased Ea indicates increased arterial impedance, resulting in higher ventricular pressure to eject the same volume of blood.
- Therapies that reduce arterial impedance can decrease Ea and restore SV.
Pathological Implications
-
Reduced Ventricular Compliance:
- Reduces EDV and SV while EDV is maintained at the expense of elevated end-diastolic pressure (frequently seen in heart failure).
- Nitrates and diuretics lower EDV and hence end-diastolic pressure (EDP); this has the desired effect of lowering left atrial pressure (LAP) and limiting pulmonary congestion but may reduce preload and SV.
-
Increased Arterial Impedance:
- Increases the ventricular pressure required to eject blood and decreases SV.
- Therapies that reduce arterial impedance (e.g., nitrates, restoration of coronary perfusion) can reduce Ea and restore SV.
-
Depressed Ventricular Contractility:
- Leads to reduced Ees and thus a reduced SV.
- Therapies that improve contractility (e.g., inotropes) can restore Ees and ventricular ejection pressure, decreasing ESV and boosting SV.
-
Elevated Left Atrial Pressure (LAP):
- Seen in the right shift of the EDV due to elevated LAP, indicative of heart failure and fluid overload.
Summary
- Normal Conditions: Balance between ventricular contractility (Ees) and arterial impedance (Ea) ensures effective stroke volume and pressure.
- Pathological Conditions: Disruptions in Ees or Ea lead to reduced SV and elevated ventricular pressures.
- Therapeutic Interventions: Aim to restore the balance by reducing arterial impedance, improving ventricular contractility, and managing preload and afterload to optimize cardiac output and reduce congestion.
Negative Pressure Pulmonary Oedema (NPPE)
Pathogenesis
- Cause: Generation of high negative intrathoracic pressures in an attempt to overcome airway obstruction.
- Hydrostatic Mechanism:
- Increased Preload and LV Afterload: Augmented venous return due to high negative pressures.
- Hypoxia: Causes hypoxic pulmonary vasoconstriction (HPV) and decreased myocardial contractility, increasing pulmonary pressure.
- Sympathetic Tone: Increased systemic vascular resistance (SVR) due to sympathetic stimulation.
- Mechanical Stress Mechanism:
- Reduced microvascular integrity leads to increased permeability.
Pathophysiology
- Hypoxia:
- Detected by peripheral chemoreceptors, triggering sympathetic stimulation.
- Airway Obstruction:
- Commonly due to involuntary biting of the endotracheal (ET) tube or laryngospasm.
- Patient attempts to inspire forcefully against the obstruction, causing highly negative intrathoracic pressure.
- Acute Increase in Systemic Venous Return to Right Heart:
- Increases pulmonary blood volume, raising pulmonary arterial and capillary pressure.
- Leads to increased pulmonary interstitial pressure and trans-capillary pressure gradient.
- Fluid Movement:
- Fluid is pushed out of pulmonary capillaries into the interstitium, causing NPPE.
Mechanisms and Effects
- Fluid Surrounds Alveoli:
- Decreases diffusion of alveolar O2 into pulmonary capillaries.
- Severe Cases:
- Pressure and fluid build-up damage capillaries and alveolar walls.
- Fluid and red blood cells enter alveoli, potentially being coughed up as frothy pink sputum.
Signs, Symptoms, and Lab Findings
- Chest X-Ray (CXR):
- Shows diffuse bilateral infiltrates.
- Blood Gases:
- Decreased PaO2 and oxygen saturation (Sats).
Management of NPPE
- Maintain a Patent Airway:
- Oxygen supplementation.
- PEEP (Positive End-Expiratory Pressure) / NIV (Noninvasive Ventilation) guided by physical examination and ABG (Arterial Blood Gas) results.
- Mechanical Ventilation:
- Reserved for severe cases that do not respond to NIV.
- Preload Reduction:
- Use GTN (Glyceryl Trinitrate) if adequate blood pressure (e.g., SBP >100 mmHg).
- May also provide beneficial afterload reduction effects.
- Diuretics:
- Often used, but there is no evidence of their utility and may exacerbate hypovolemia and hypoperfusion.
- Clinical Course:
- NPPE usually resolves rapidly within 12-48 hours when recognized early and treated immediately.
Neurogenic Pulmonary Edema
Pathophysiology of Pulmonary Edema in Acute CNS Injury
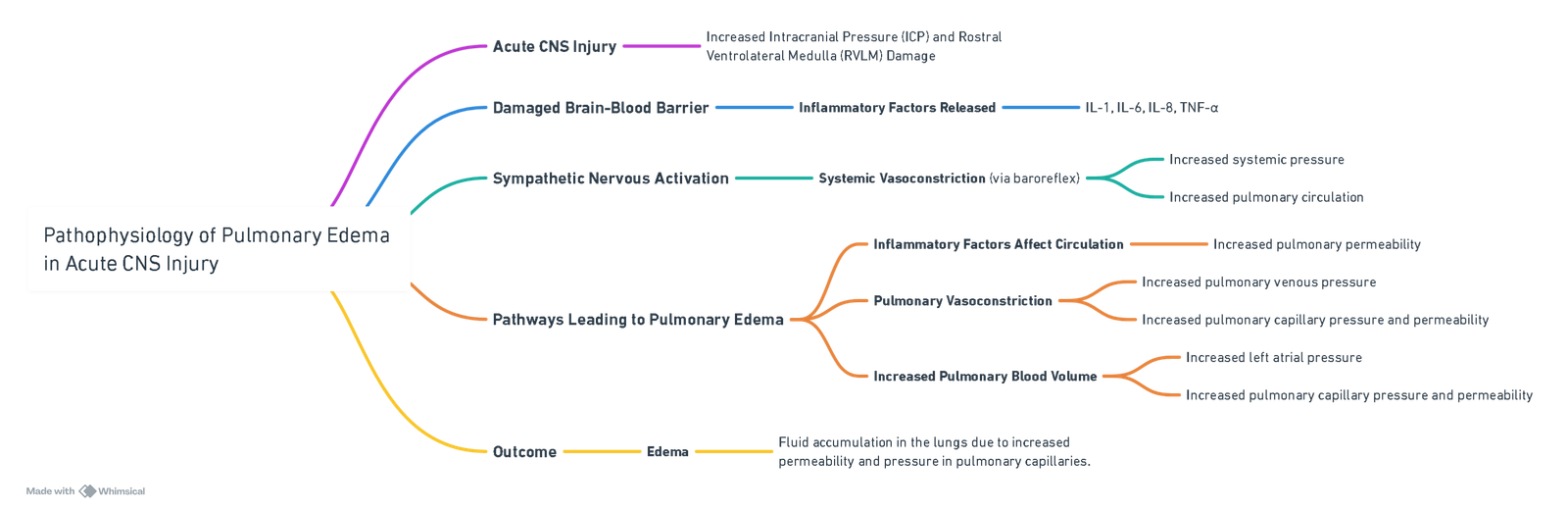
View or edit this diagram in Whimsical.
Links
- Heart failure
- Ventilation and Weaning
- Pulmonary Hypertension
- Acute Respiratory Distress Syndrome (ARDS)
References:
- The Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- Reddi, B. A. J., Shanmugam, N., & Fletcher, N. (2017). Heart failure—pathophysiology and inpatient management. BJA Education, 17(5), 151-160. https://doi.org/10.1093/bjaed/mkw067
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “2b779e61-533c-4b6b-bd9e-7f6c67a48205”



