Summary
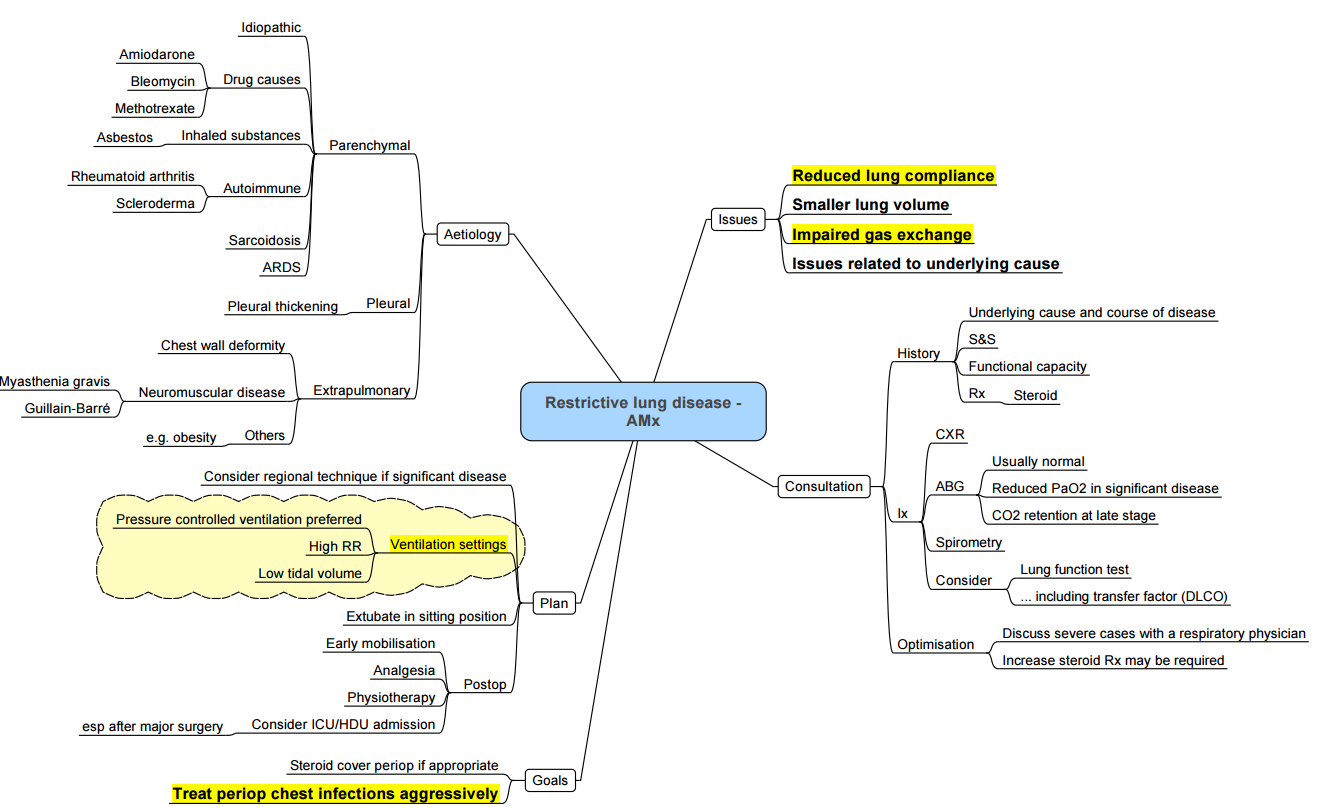
Restrictive Lung Disease
Key Anaesthetic Considerations
- Anticipate potential difficulty with bag-mask ventilation and rapid desaturation due to reduced functional residual capacity (FRC).
- Respiratory physiology is often altered:
- Hypoxemia primarily due to ventilation-perfusion mismatch.
- Decreased lung compliance, with increased susceptibility to barotrauma and pneumothorax.
- Presence of pulmonary hypertension and potential for cor pulmonale.
- Elevated risk of perioperative respiratory complications, including
- Pneumonia
- Pneumothorax
- Respiratory depression (especially in response to opioids)
- Respiratory failure
Indicators of Elevated Risk
- Vital capacity (VC) < 15 mL/kg
- Forced vital capacity (FVC) < 50% predicted or < 500 mL
- Arterial carbon dioxide tension (pCO₂) > 45 mmHg
- Elective surgeries should be postponed in the presence of acute and reversible respiratory conditions.
Intraoperative and Perioperative Management
- Use of advanced ventilatory support may be required:
- High-performance ventilators
- Low tidal volumes with increased respiratory rates
- Postoperative mechanical ventilation and ICU monitoring may be necessary
Underlying Conditions and Associated Comorbidities
- Common etiologies include:
- Autoimmune and connective tissue disorders
- Idiopathic pulmonary fibrosis (IPF)
- Acute respiratory distress syndrome (ARDS)
- Malignancy
- Obesity hypoventilation syndrome
- Neuromuscular disorders
- Drug-induced lung injury
Medications of Concern
-
Chronic use of:
- Corticosteroids
- Immunosuppressive agents
- Supplemental oxygen therapy
- Agents for pulmonary hypertension
Note prior exposure to agents associated with pulmonary toxicity such as bleomycin and amiodarone.
Anaesthetic Goals
Preoperative Phase
- Optimization is limited, especially in chronic or irreversible cases.
- Aim for minimally invasive approaches when possible
- Prefer local or regional anaesthesia
- If general anaesthesia is required, ensure maximal supportive care and plan for slow postoperative weaning
Intraoperative Ventilatory Strategy
- Employ lung-protective ventilation technique
- Low tidal volume
- Higher respiratory rate
- Consider inverse ratio ventilation
- Pressure control ventilation modes
- Application of positive end-expiratory pressure (PEEP)
- If prior bleomycin exposure, limit oxygen concentration to reduce risk of oxygen toxicity.
- Avoid triggers of pulmonary hypertension:
- Prevent hypoxia, hypercapnia, acidosis, and uncontrolled pain.
Postoperative Care
- Effective analgesia is critical to prevent hypoventilation and respiratory failure
- Consider multimodal pain management techniques, including regional blocks or epidural analgesia, when not contraindicated.
Links
References:
1. Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
2. Groeben H. Strategies in the patient with compromised respiratory function. Best Pract Res Clin Anaesthesiol. 2004 Dec;18(4):579-94. doi: 10.1016/j.bpa.2004.05.013. PMID: 15460547.
Copyright
© 2025 Francois Uys. All Rights Reserved.
Summary or mindmap:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “6f42bfbb-2180-48fa-856f-5851d0124485”



