{}
Introduction
How is Spirometry Performed
Spirometry involves the patient inhaling until the lungs are full, then rapidly and forcefully exhaling. This test relies heavily on patient effort and must be performed correctly to obtain valid results. The test is repeated until three acceptable and consistent results are achieved.
Measurements in Spirometry
- FVC (Forced Vital Capacity): Total volume of air exhaled after full inspiration, typically measured in the first 6 seconds.
- FEV1 (Forced Expiratory Volume in 1 second): Volume of air exhaled in the first second.
- FEV1/FVC Ratio: This ratio, expressed as a fraction, should be between 0.7 and 0.8 under normal conditions.
- FEF25–75 (Forced Expiratory Flow at 25–75% of the pulmonary volume): Measures the flow rate during the middle portion of the FEV1.
(Normal values are derived from tables based on data from normal controls and vary by height, gender, and ethnicity.)
These measurements are based on flow over time. Flow volume loops, which plot flow rates against volume, are discussed in a separate chapter.
Indications
-
Diagnosis: Spirometry confirms the presence and severity of obstructive and restrictive lung diseases.
-
Bronchodilator Response: Helps differentiate asthma from COPD, and assesses progression and response to therapy.
-
Preoperative Assessment: Not routinely necessary for non-thoracic surgery but important in patients evaluated for lung resection. Simple spirometry, FVC, and FEV1 should be obtained.
-
Predicted Postoperative FEV1 (ppoFEV1): Calculated using the formula:
ppoFEV1 = {preop FEV1% x (1 – frac% functional lung removed)}/ 100
- A ppoFEV1 < 40% indicates a higher risk of postoperative complications.
- Patients with a ppoFEV1 < 30% may require postoperative ventilation and need additional testing.
Specific Indications for Spirometry
- Active wheezing or impaired exercise tolerance.
- Asthma, COPD, scoliosis (if not assessed in the past 12 months).
- ASA 3/4 patients with respiratory disease undergoing intermediate or high-risk surgery.
- Evaluation for lung resection.
How is FRC Measured
Body Plethysmography
- Measures total residual gas in the lungs, including air trapped in bullae and behind closed airways.
- Conducted in an airtight box with a mouthpiece. The patient breathes against a closed mouthpiece.
- Uses Boyle’s law: (P1V1 = P2V2 ).
Helium Dilution
- Measures only ventilated lung volume.
- Involves a spirometer containing helium (initial concentration (C1 ) and volume (V1 )).
- The patient breathes into the spirometer until equilibrium is achieved.
- After equilibrium, the new helium concentration (C2) is measured.
- The formula used is: (C1x V1 = C2 x V2).
Note: The difference between measurements from body plethysmography and helium dilution accounts for any bullae or trapped air.
How is Closing Capacity Measured
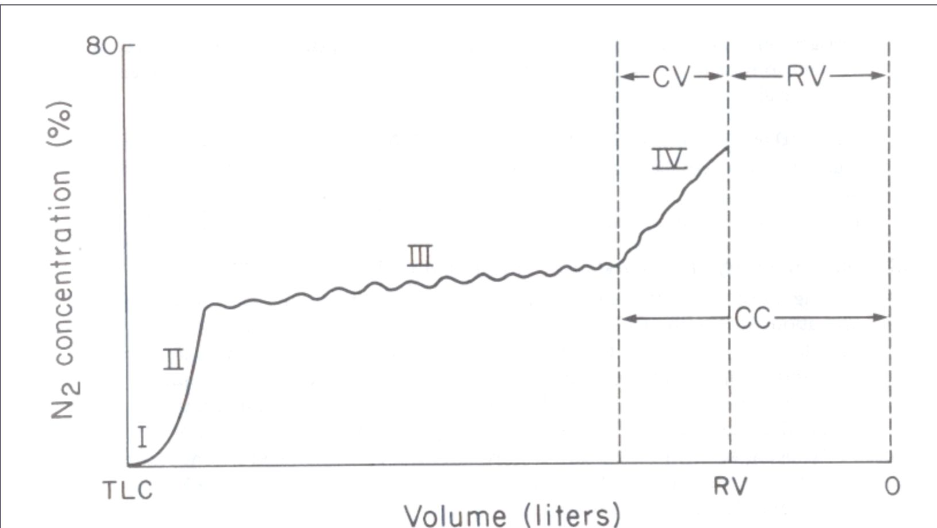
Closing Volume (CV)
Closing Volume (CV) is the volume in the lungs at which the small airways begin to close during expiration. This is an important measurement in assessing small airway function.
Residual Volume (RV)
Residual Volume (RV) is the volume of air remaining in the lungs after a maximal exhalation. This volume cannot be exhaled and ensures that the lungs do not collapse.
Nitrogen Washout Technique
During a nitrogen washout test, an abrupt increase in nitrogen concentration is noted. This occurs due to the closing of the basal airways, leading to the preferential emptying of the poorly ventilated apices, which contain a higher nitrogen concentration. This observation is crucial for evaluating the distribution of ventilation within the lungs.
Normal Vs Obstructive Vs Restrictive
Normal
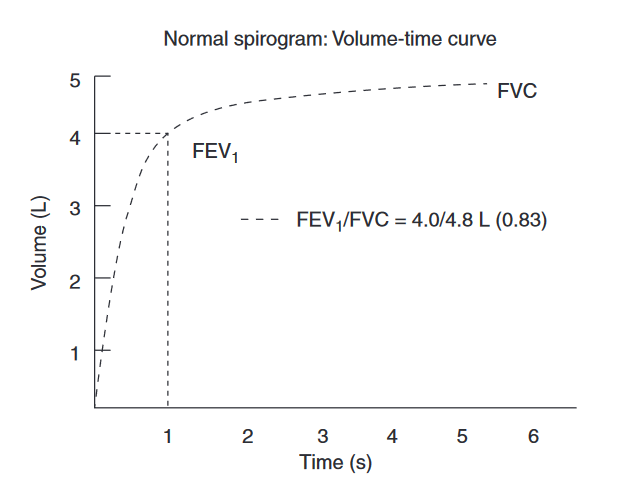
FEV1 and FVC are >80% of predicted. FVC1/FVC is >0.7.
Obstructive
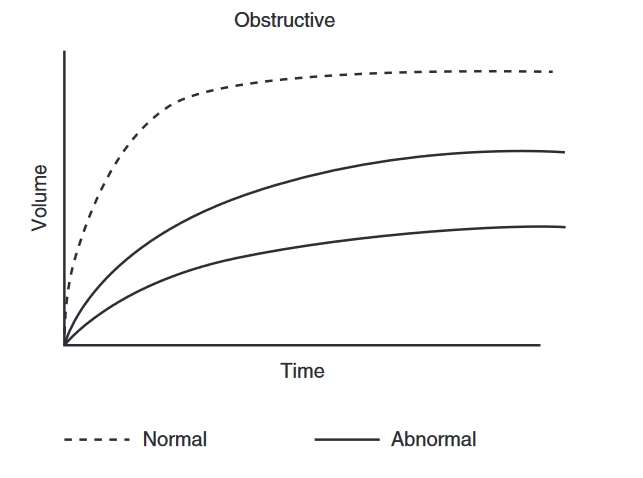
Obstructive Lung Disease Criteria
- FEV1 < 80% of Predicted: Indicates an obstructive pattern when FEV1 is less than 80% of the predicted value.
- FVC: May be normal or reduced, but typically decreased to a lesser degree than FEV1.
- FEV1/FVC Ratio < 0.7: Confirms the presence of obstructive lung disease.
GOLD Spirometric Criteria for COPD Severity
The Global Initiative for Chronic Obstructive Lung Disease (GOLD) criteria categorize COPD severity based on post-bronchodilator FEV1:
-
Mild (Stage I):
- FEV1/FVC < 0.7
- FEV1 ≥ 80% of predicted
- May be asymptomatic
-
Moderate (Stage II):
- FEV1/FVC < 0.7
- 50% ≤ FEV1 < 80% of predicted
- Dyspnea on exertion
-
Severe (Stage III):
- FEV1/FVC < 0.7
- 30% ≤ FEV1 < 50% of predicted
- Activity limited by SOB. Exacerbations may be severe
-
Very Severe (Stage IV):
- FEV1/FVC < 0.7
- FEV1 < 30% of predicted or FEV1 < 50% of predicted with chronic respiratory failure
- Impaired quality of life
Bronchodilator Testing
Bronchodilator testing assesses the reversibility of airflow obstruction, which indicates the potential benefit from bronchodilator therapy. This test involves measuring FVC and FEV1 at baseline and after administering an inhaled bronchodilator.
- Significant Response: An increase in FEV1 of at least 12% or 200 ml from baseline is considered significant, supporting the diagnosis of asthma.
Restrictive
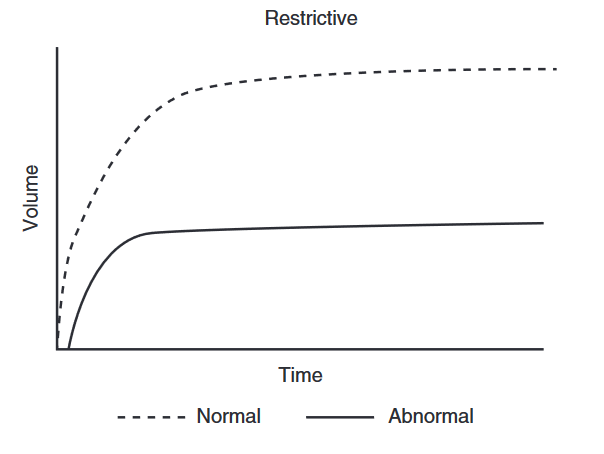
Restrictive Lung Disease Criteria
- FEV1: Normal or slightly reduced.
- FVC: Less than 80% of predicted.
- FEV1/FVC Ratio: Greater than 0.7.
Mixed Restrictive and Obstructive Disorders
- When both FEV1 and FVC are reduced, the patient may have a mixed restrictive and obstructive disorder.
- Severe obstruction can lead to air trapping, which affects these measurements.
Air Trapping Assessment
To differentiate between mixed disorders and air trapping due to severe obstruction, additional lung volume measurements are necessary:
- Total Lung Capacity (TLC): Should be measured to evaluate overall lung volume.
- Residual Volume (RV): Increased residual volume indicates air trapping.
Summary
- FEV1 < 80% of predicted with normal or reduced FVC and FEV1/FVC < 0.7 suggests obstructive lung disease.
- FEV1 normal or slightly reduced, FVC < 80% of predicted, and FEV1/FVC > 0.7 indicates restrictive lung disease.
- Both FEV1 and FVC reduced may indicate mixed restrictive and obstructive disorders, or severe obstruction with air trapping.
- Increased RV confirms air trapping.
Links
References:
- Raj, T. D. (2017). Data interpretation in anesthesia.. https://doi.org/10.1007/978-3-319-55862-2
- Ntima, N. and Lumb, A. B. (2019). Physiology and conduct of pulmonary function tests. BJA Education, 19(6), 198-204. https://doi.org/10.1016/j.bjae.2019.02.002
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “2c5a6709-6c05-485b-99f3-cb219be6fd9d”



