{}
Cardiac Anaesthesia Made Easy
Preoperative Management
Patient Examination
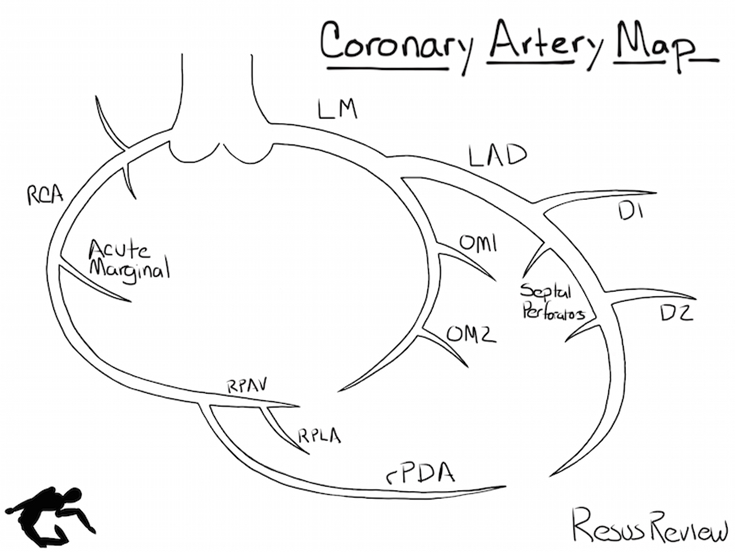
- Cath Report and Echo: Critical information includes:
- Left main disease or equivalent
- Poor distal targets
- Ejection fraction
- Left ventricular end-diastolic pressure (LVEDP)
- Presence of aneurysm
- Pulmonary hypertension
- Valvular lesions
- Congenital lesions
- Laboratory Tests: Minimal tests required:
- Complete blood count (CBC)
- Platelet count (Plt)
- Electrolytes (Lytes)
- Blood urea nitrogen (BUN)
- Creatinine (Cr)
- Glucose (Glu)
- Prothrombin time (PT)
- Partial thromboplastin time (PTT)
- Chest X-ray (CXR): Evaluate for cardiomegaly, tumors, pleural effusions.
- Electrocardiogram (ECG):
- Left bundle branch block (LBBB) is critical if a pulmonary artery catheter is planned, as it can occasionally lead to third-degree block with PA catheter placement.
Consent and Information
- Inform patients about the A-line, PA catheter, and postoperative ventilation.
- Discuss potential complications of cardiac surgery:
- Myocardial infarction (MI) 6%
- Cerebrovascular accident (CVA) 5%
- Neuropsychiatric effects 90%
- Death 1-3-10% (depending on risk)
- Transfusion (40-90%)
- Pneumonia 10%
Premedication
- 40% of patients experience preoperative ischemia with good premedication. Most will without.
- Consider anxiolytic medication.
Planning for Early Extubation
- Treat all patients as candidates for early extubation and evaluate qualification.
- Strategies include limiting fluid administration, reducing total narcotic and benzodiazepine doses, relying on volatile agents or propofol during the case, providing easily titratable postoperative sedation (e.g., propofol), and carefully controlling blood pressure during emergence.
Intraoperative Management
Preparation
Equipment
- Standard room setup: Suction, machine checkout, airway equipment.
- Brain function monitoring (BIS), regional cerebral oximetry (INVOS).
- Transesophageal echocardiography (TOE) probe setup and patient details entry.
- Coordinate with the blood bank to arrange blood units for the theatre.
Drugs
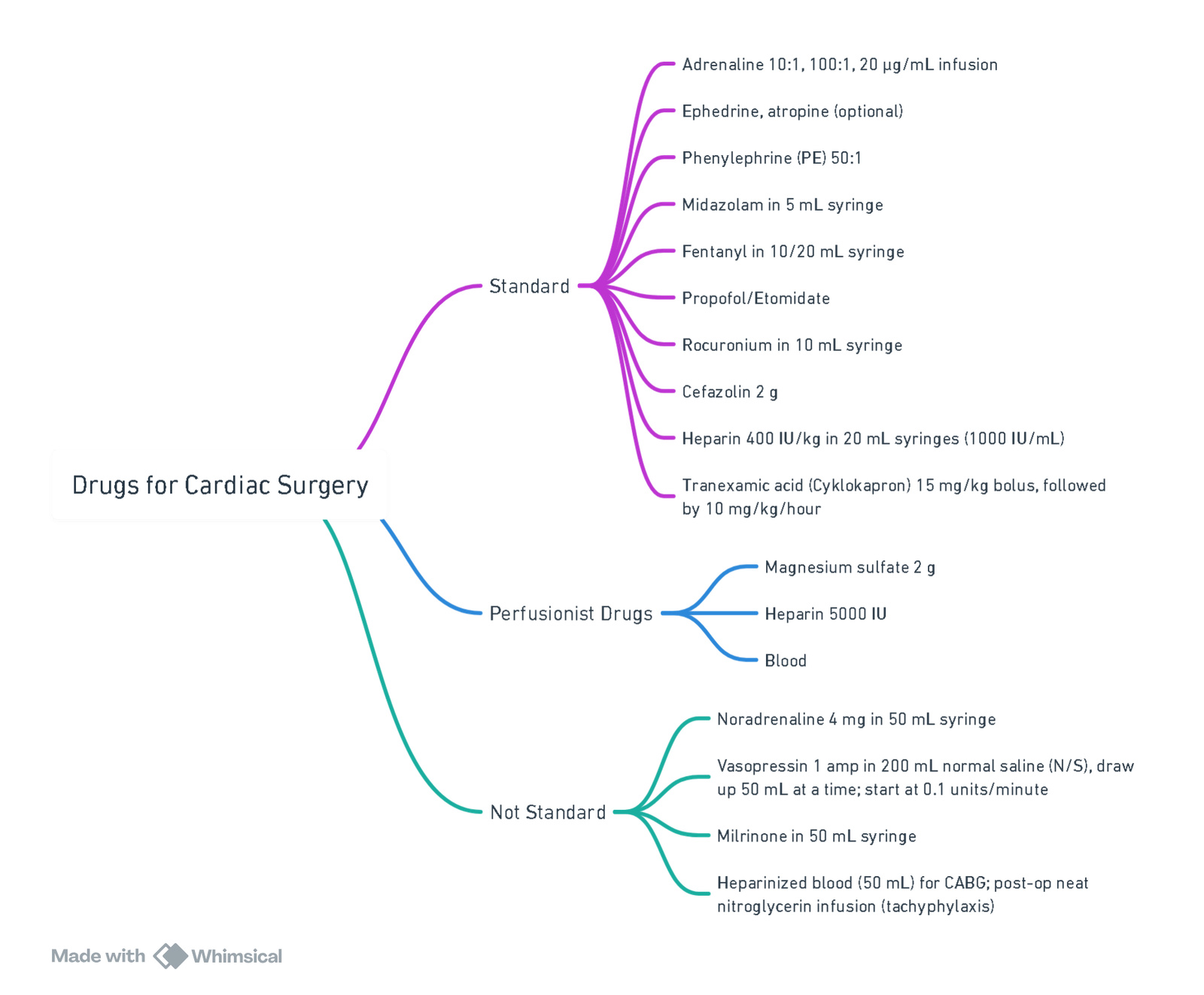
View or edit this diagram in Whimsical.
Patient Setup
- IV Line: 16G to clave.
- Fluid administration.
- Phenylephrine later propofol off pump.
- Tranexamic acid later protamine off pump.
- Arterial Line (Right arm for CABG to avoid interference with vein harvesting):
- Baseline activated clotting time (ACT) and arterial blood gas (ABG).
- Central Venous Pressure (CVP):
- Brown: CVP monitoring.
- Blue: Adrenaline.
- White: Fluid.
- Large-bore IV access (<16G), A-line on right, setup in the room with oxygen, 5-lead ECG for baseline comparison.
- Hep lock one IV if two large-bore IVs are placed to prevent inadvertent fluid administration.
Goals for Different Valves
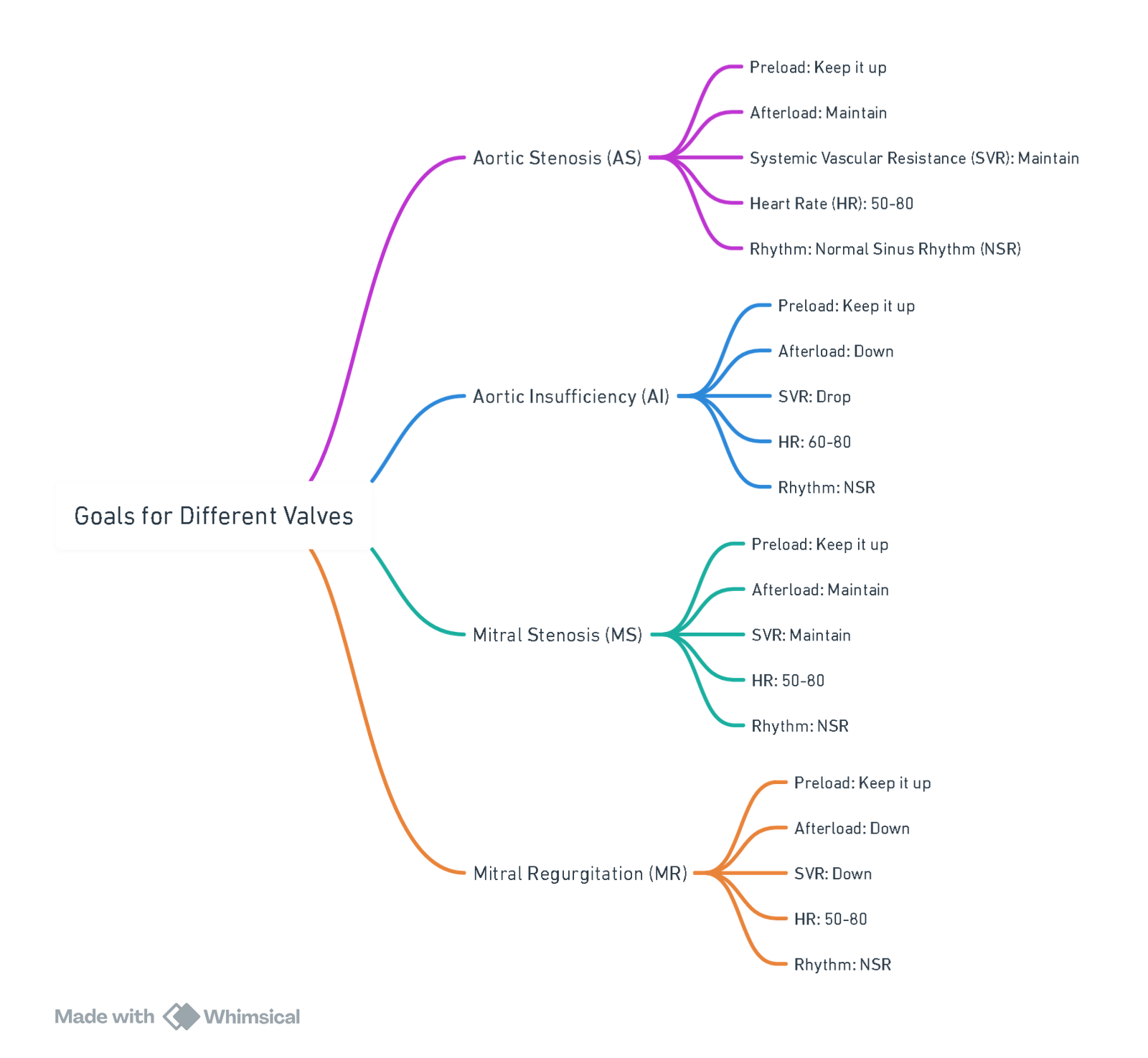
View or edit this diagram in Whimsical.
Pre-bypass
1. Anticoagulation
- Heparin Administration: Administer Heparin at a dose of 400 IU/kg.
- Target Activated Clotting Time (ACT): Ensure ACT exceeds 450 seconds to maintain adequate anticoagulation.
2. Cannulation
- Arterial Cannulation:
- Site: Typically performed in the ascending aorta due to its accessibility, sufficient diameter, and lower risk for aortic dissection.
- Procedure: During the arteriotomy, decrease systemic pressure, targeting a mean arterial pressure (MAP) of less than 70 mmHg (SBP <100 mmHg)
- Complications:
- Inadvertent perforation of aortic arch vessels.
- Aortic dissection.
- Embolization of air or atheromatous material.
- Other vascular wall injuries.
- Venous Cannulation:
- Standard Technique:
- Insert an atrial cannula through the right atrium, directing it inferiorly toward the inferior vena cava (IVC).
- Position drainage holes in the IVC and right atrium to drain blood from the lower extremities, superior vena cava (SVC), and coronary sinus.
- Bicaval Technique (Used when right atrial access is required during surgery):
- Cannulate both the SVC and IVC.
- This technique may not adequately drain the coronary sinus, requiring an additional vent or atriotomy.
- Considerations: Ensure venous flow from the SVC is not impaired to prevent SVC syndrome.
- Standard Technique:
- Left Ventricular Management during CPB:
- Objective: Avoid left ventricular (LV) filling and distention to:
- Minimize LV wall tension.
- Prevent myocardial rewarming.
- Reduce myocardial oxygen demand.
- Sources of Blood Return to LV: Blood may return to the LV from:
- Bronchial and thebesian veins.
- Blood navigating through the pulmonary circulation.
- Interventions:
- To avoid LV distention, place a vent in the LV through the left superior pulmonary vein.
- If retrograde cardioplegia is used, an aortic root vent may be necessary during the aortic cross-clamp period.
- Objective: Avoid left ventricular (LV) filling and distention to:
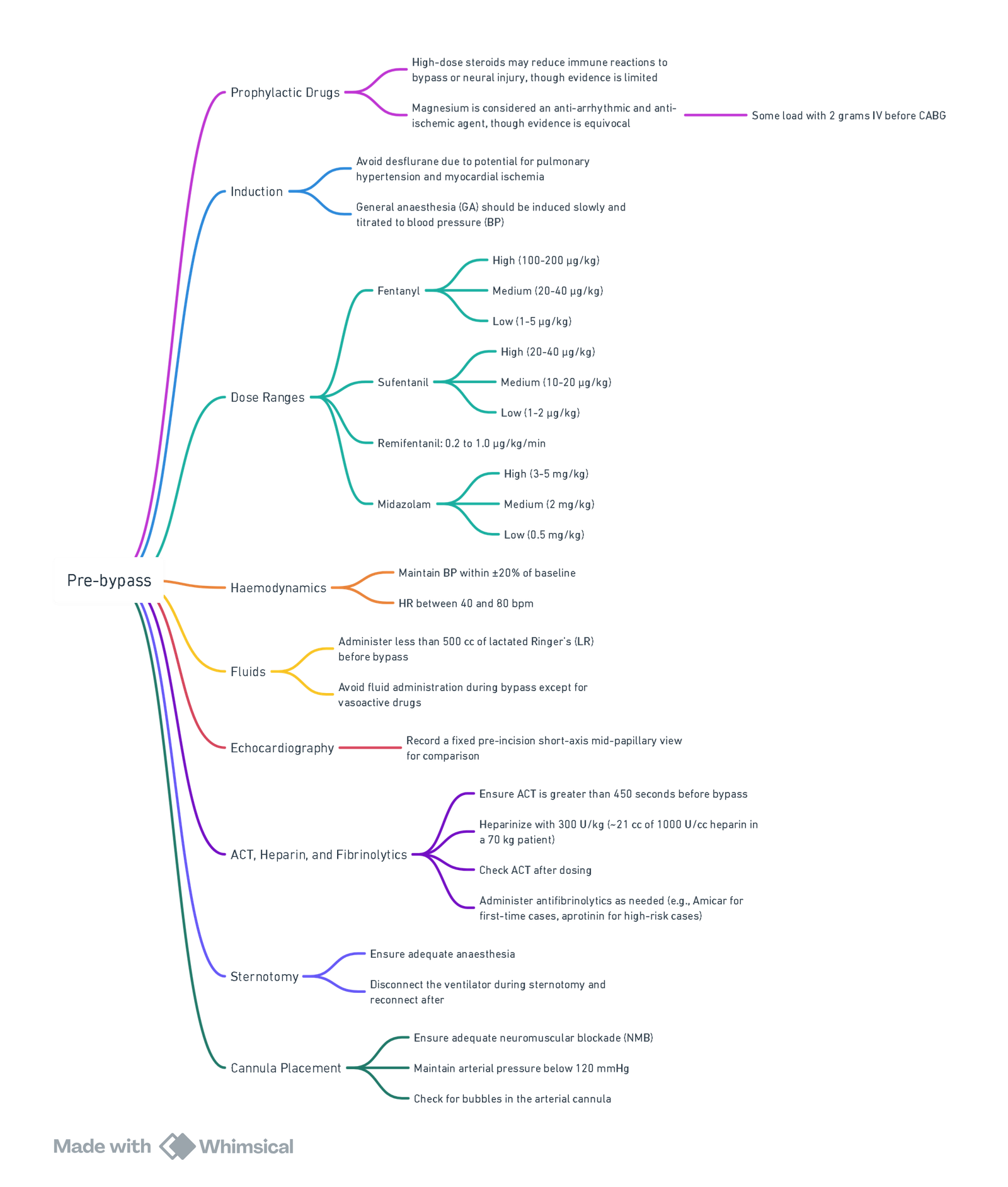
View or edit this diagram in Whimsical.
Bypass
- Hemodilution: Upon initiation of CPB, systemic arterial hypotension commonly occurs due to the acute reduction in blood viscosity caused by hemodilution with nonblood priming solutions.
- Transition to Nonpulsatile Flow: The change from normal pulsatile blood flow to the nonpulsatile flow administered by CPB affects vascular resistance and mean arterial pressure (MAP). These changes are usually transient.
- Effects of Hypothermia:
- MAP Increase: Hypothermia during CPB induces vasoconstriction, leading to an increase in systemic vascular resistance and subsequently raising MAP.
Pump Flow and Pressure Management during CPB
- Balancing Surgical Visualization and Oxygen Delivery:
- Pump flow and pressure are carefully titrated to balance the need for clear surgical visualization with the requirement for adequate oxygen delivery to tissues.
- Determinants of Pump Flow and Pressure:
- Overall arterial impedance, which depends on temperature, hemodilution, and arterial cross-sectional area.
- Pump Flow Guidelines:
- Microcirculation Perfusion: At hematocrit levels of 22% and with induced hypothermia, pump flows of 1.2 L/min/m² can adequately perfuse most of the microcirculation.
- Normothermic Target Flow Rate: In normothermic adult patients, the target flow rate during CPB is typically 2.2–2.4 L/min/m².
- Nomograms: These are used to determine the ideal pump flow rate based on temperature and oxygen consumption.
- Monitoring and Adjusting Perfusion:
- Mixed Venous Saturation: A target mixed venous oxygen saturation (SvO2) of 70% or greater is often monitored during CPB. However, this does not always ensure adequate perfusion, as certain tissue beds, such as muscle and subcutaneous fat, may be functionally excluded from circulation during CPB.
- Cerebral Oximetry: Monitoring cerebral oximetry or other physiological measurements of brain function can provide additional guidance for optimizing CPB flow rates to ensure adequate cerebral perfusion.
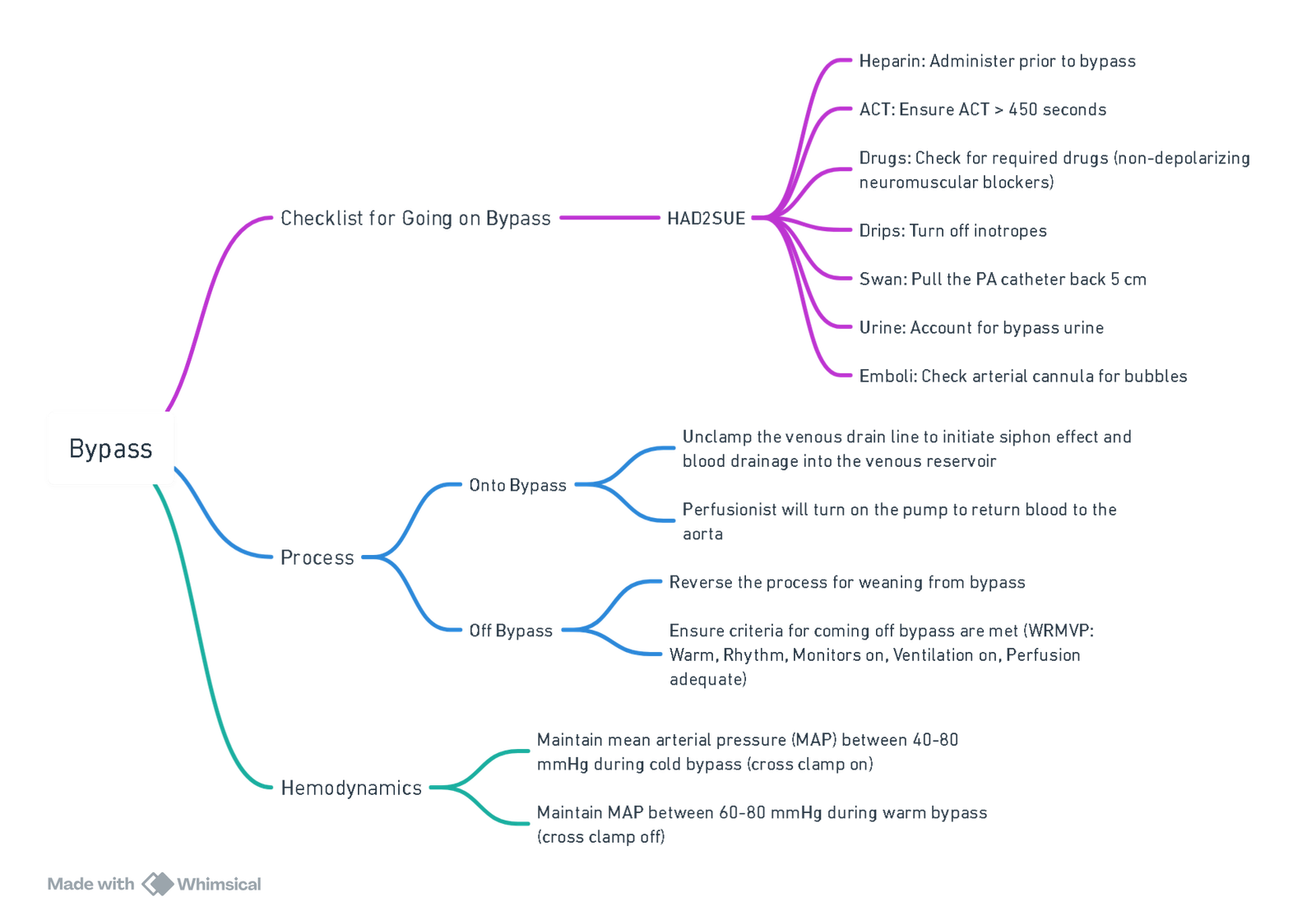
View or edit this diagram in Whimsical.
Hemodynamic Monitoring
- Arterial Pressure Tracing: Upon initiation of CPB and full support, the arterial pressure tracing will lose its characteristic pulsatile waveform. Once the heart is arrested, the tracing will be completely devoid of pulsatile activity, though a mean arterial pressure (MAP) will still be visible.
- MAP Monitoring:
- The primary concern during CPB is cerebral perfusion, which also indicates systemic perfusion adequacy.
- MAP Target:
- Maintain a MAP between 50–100 mm Hg to ensure cerebral blood flow in patients without preexisting conditions.
- In patients with preexisting hypertension, adjust the MAP target to 60 mm Hg.
Metabolic and Systemic Responses
- Systemic Inflammatory Response: CPB induces a complex physiologic response similar to systemic inflammatory response syndrome (SIRS), which includes:
- Decreased insulin release.
- Increased insulin resistance.
- Hyperglycemia.
- Hyperglycemia Management:
- Hyperglycemia during CPB (blood glucose levels >180 mg/dL) is detrimental to neurologic recovery, especially in ischemic brain areas.
- Insulin Administration: Administer insulin during CPB, commonly at a rate of 10 units/h, and adjust based on blood glucose levels, with close monitoring.
Anesthetic Management
- Inhaled Anesthetics:
- Since the lungs are bypassed, the delivery of inhaled anesthetics falls under the perfusionist’s responsibility.
- A vaporizer with a volatile agent, typically isoflurane, is part of every CPB machine. Upon CPB initiation, ensure that the isoflurane vaporizer is set to 1% and titrate as needed.
- Total IV Anesthesia: If issues arise with the vaporizer, anesthetic agents can be administered intravenously.
- Neuromuscular Blockers:
- Can be administered by the anesthesiologist after ensuring that the patient has received an adequate dose of anesthetic and analgesic agents.
- Anesthetic Requirements:
- Dosage requirements decrease during hypothermia but increase during rewarming. Consider administering intravenous agents like midazolam during rewarming.
Temperature Monitoring and Management
- Core and Cerebral Temperature:
- While temperature control is primarily managed by the perfusionist using the CPB machine’s heat exchanger, the anesthesiologist should monitor temperature to approximate core and cerebral temperatures.
- Core Temperature: Measured via bladder, rectal, or esophageal thermometers.
- Cerebral Temperature: Best approximated by nasopharyngeal or tympanic membrane measurements.
- Cerebral Metabolic Rate of Oxygen (CMRO2): CMRO2 decreases by 7% for each 1°C drop in temperature.
Blood Gas Management
- Alpha-Stat Management:
- The most common method used in cardiac surgery.
- Blood gases are analyzed at 37°C to maintain electrical neutrality between hydrogen (H+) and hydroxyl (OH−) ions, which decrease in concentration with decreasing temperature.
- The resulting alkalosis at lower temperatures is corrected when the blood sample is warmed during analysis.
- pH-Stat Management:
- Primarily used in pediatric patients, particularly during circulatory arrest.
- This method involves temperature-corrected blood gas analysis to report pH at the actual hypothermic temperature and maintaining a pH of 7.4 and CO2 tension of 40 mm Hg by adding CO2 to the oxygenator gas inflow.
- Physiologic Effects:
- Cerebral vasodilation, resulting in increased cerebral blood flow and better brain cooling prior to deep hypothermic circulatory arrest.
- This method carries a higher risk of emboli in patients with atheromatous disease, which is why it is more popular in children than adults.
- Clinical Outcomes: There is little evidence to suggest that one method is superior to the other in terms of overall outcomes, except for the specific benefit of pH-stat management in children undergoing circulatory arrest.
Post-bypass
Before discontinuing CPB, several steps must be taken to restore and optimize cardiac and pulmonary function. The transition from CPB to the patient’s own circulation is a critical phase in cardiac surgery.
Key Preparations Prior to Weaning from CPB
-
Rewarming:
- Ensure that the nasopharyngeal temperature is between 36°C and 37°C.
- Rectal or bladder temperature should be greater than 35°C but less than 37°C.
-
Cardiac Rate and Rhythm:
- Achieve a stable cardiac rate and rhythm. Pacing may be required to maintain this stability.
-
Monitoring:
- Confirm that all monitors and the arterial line are in place and functioning correctly.
-
Ventilation:
- Reinstitute mechanical ventilation.
-
Intravenous Fluids:
- Restart intravenous fluid administration.
-
Pharmacologic Support:
- Ensure that inotropes, vasodilators, and vasopressors are prepared and readily available.
-
Metabolic Parameters:
- Normalize arterial pH, pa02 and paC02
- Target hematocrit (Hct) levels between 20% and 25%.
- Maintain potassium levels between 4.0 and 5.0 mEq/L.
- Ensure ionized calcium levels are within normal limits.
-
Acid–Base, Electrolyte, and Hemoglobin Optimization:
- Correct any acid–base imbalances, calcium, and potassium abnormalities.
- Maintain adequate hemoglobin levels, with a nadir hemoglobin level recommended at 6–7 g/dL by the Society for Thoracic Surgeons, potentially higher in select cases.
-
Anesthesia Management:
- Additional doses of anesthetic agents may be required during the rewarming phase due to the risk of intraoperative awareness as brain normothermia is restored.
Ventilation Considerations After CPB
- Lung Reinflation:
- The lungs must be reinflated with positive pressure, applied repeatedly until atelectasis is resolved.
- Increased Ventilatory Rate:
- To compensate for increased dead space (which can lead to increased PaC02 and modest increases in pulmonary shunt fraction), potentially leading to suboptimal oxygenation and decreased Pa02, increase the ventilatory rate by 10%–20% above pre-CPB values.
- FiO2 Adjustment:
- Set FiO2 between 80% and 100%, with further adjustments based on arterial blood gas analysis.
Separation from CPB
-
Process:
- Once cardiopulmonary function has been optimized, the venous outflow line is slowly clamped.
- The patient’s intravascular volume and ventricular loading conditions are restored by transfusion of perfusate through the aortic inflow line.
- When conditions are optimal, the aortic inflow line is clamped, and CPB is discontinued.
-
Monitoring and Potential Restart of CPB:
- After separation from CPB, carefully monitor the patient’s oxygenation, ventilation, and perfusion status.
- If these parameters are compromised, CPB can be reinitiated by unclamping the venous and arterial lines and restoring pump flow to provide systemic support.
-
Post-CPB Support:
- If necessary, utilize pharmacologic agents (vasopressors, inotropes, inodilators) and mechanical myocardial assistance (e.g., temporary cardiac pacing, intra-aortic balloon pump counterpulsation) to stabilize the patient.
Final Steps
- Removal of Cannulae:
- Once cardiac parameters are optimized, remove the vascular access cannulae.
- Reversal of Anticoagulation:
- Reverse anticoagulation using protamine sulfate.
- Closing:
- Complete the procedure by closing the thoracic incisions.
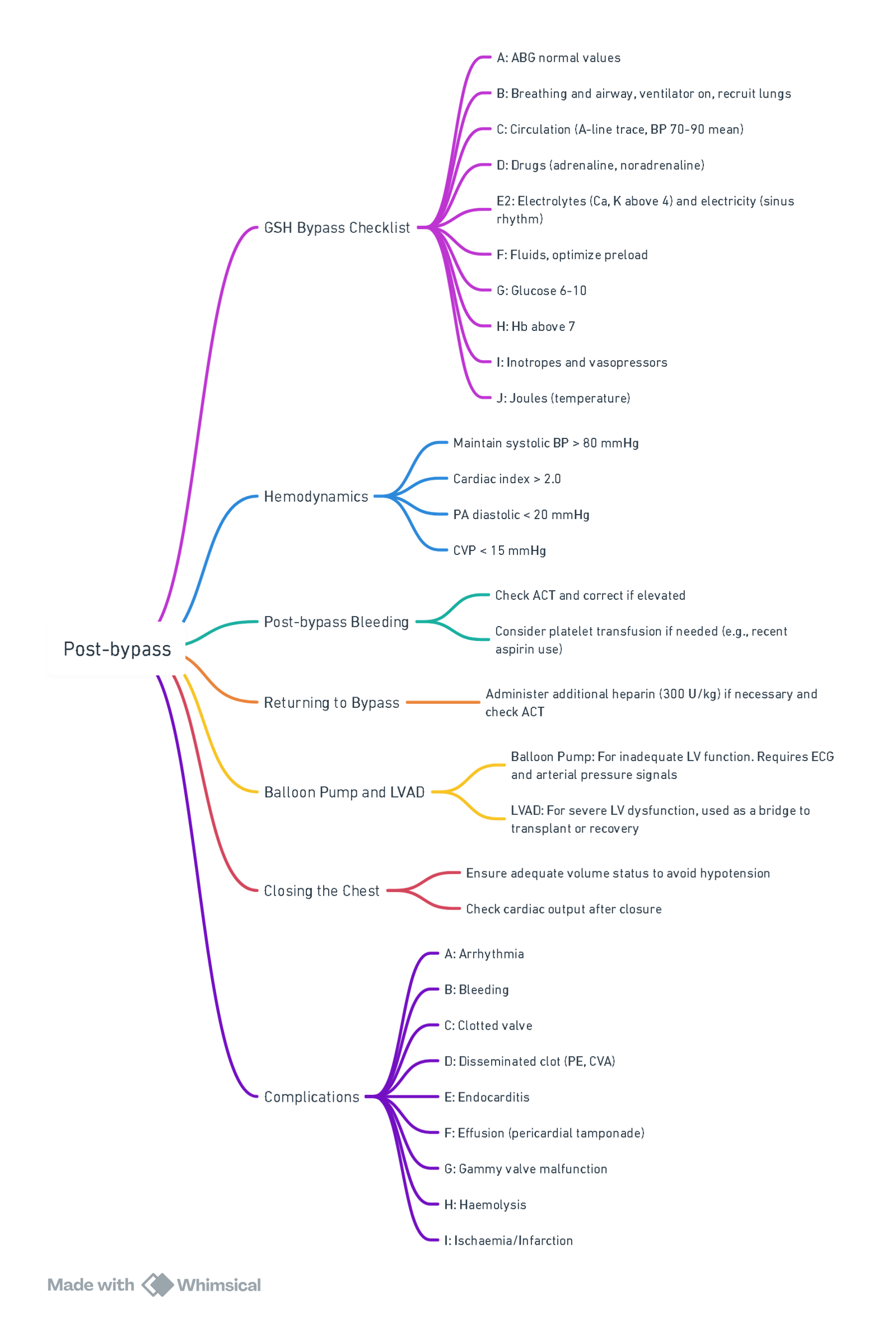
View or edit this diagram in Whimsical.
“THIEVES” Mnemonic
- Temperature
- Normothermia: Ensure the patient is normothermic to maximize cardiac contractility and reduce the risk of arrhythmias.
- Hemoglobin
- Target Hemoglobin: Confirm that hemoglobin levels are at least 7 g/dL.
- Infusions
- Inotropic Support: Initiate inotropic support if necessary, especially after the removal of the aortic cross-clamp.
- Electrolytes
- Potassium Levels: Ensure potassium is within the normal range, ideally between 4–5 mEq/L.
- Ventilation
- Lung Management: The lungs should be fully expanded and ventilated. If the patient can tolerate it, ensure the delivery of a volatile anesthetic agent.
- ECG
- Cardiac Pacing: Pace the heart at a rate of 90 beats per minute (bpm). This rate is optimal for balancing oxygen demand with heart rate, filling, and cardiac output, particularly in a heart with decreased compliance post-CPB.
- Special Considerations
- Mechanical Support: Evaluate the need for mechanical support, such as an intra-aortic balloon pump or a ventricular assist device, and determine if these need to be reactivated.
- Transesophageal Echocardiography (TEE):
- Use TEE to assess the adequacy of deairing maneuvers.
- Evaluate the effectiveness of valve repair or replacement if such procedures were performed.
Hypotension Management
| CVP | PAP | PADP or PAWP* | Cardiac Output | Blood Pressure | LV Function by TEE | RV Function by TEE | Diagnosis | Response |
|---|---|---|---|---|---|---|---|---|
| Low | Low | Low | Low | Low | Normal or hyperdynamic | Normal or hyperdynamic | Hypovolemia | Administer volume |
| Low or normal | Low or normal | Low or normal¶ | High | Low | Normal or hyperdynamic | Normal or hyperdynamic | Vasoplegia | Administer vasopressor |
| High or normal | High | Low or normal¶ | High | Low | Normal | Normal or hypocontractile | Pulmonary hypertension | Administer pulmonary vasodilator |
| High | Normal or low | Normal or high¶ | Low | Low | Normal | Hypocontractile, often dilated | Right ventricular dysfunction | Administer inotropic agent Administer pulmonary vasodilator |
| Normal or high | Normal or high | High | Low | Low | Hypocontractile, often dilated | Normal | Left ventricular dysfunction | Administer inotropic agent |
Off-Pump CABG
- Choose an anesthetic that lowers the heart rate (fentanyl, sufentanil, alfentanil, remifentanil).
- Use a median sternotomy approach with the perfusionist on standby.
- Anticoagulate similarly to on-pump CABG (Heparin 300 U/kg).
- Prophylaxis for arrhythmias (Magnesium 2 g IV, Lidocaine 100 mg followed by 2 mg/min infusion, Amiodarone if necessary).
- Load with volume after heart retraction and maintain pressure with vasoconstrictors.
- Adjust ventilator settings to reduce motion (small tidal volumes, increased rate).
- Plan for further heart rate reduction if necessary (esmolol, adenosine).
- Avoid glycopyrrolate or atropine for HR increase.
- Reverse heparin gently with protamine. Check ACT during protamine administration to avoid overdosing.
- Consider postoperative anticoagulation after protamine reversal.
Pulmonary Hypertension
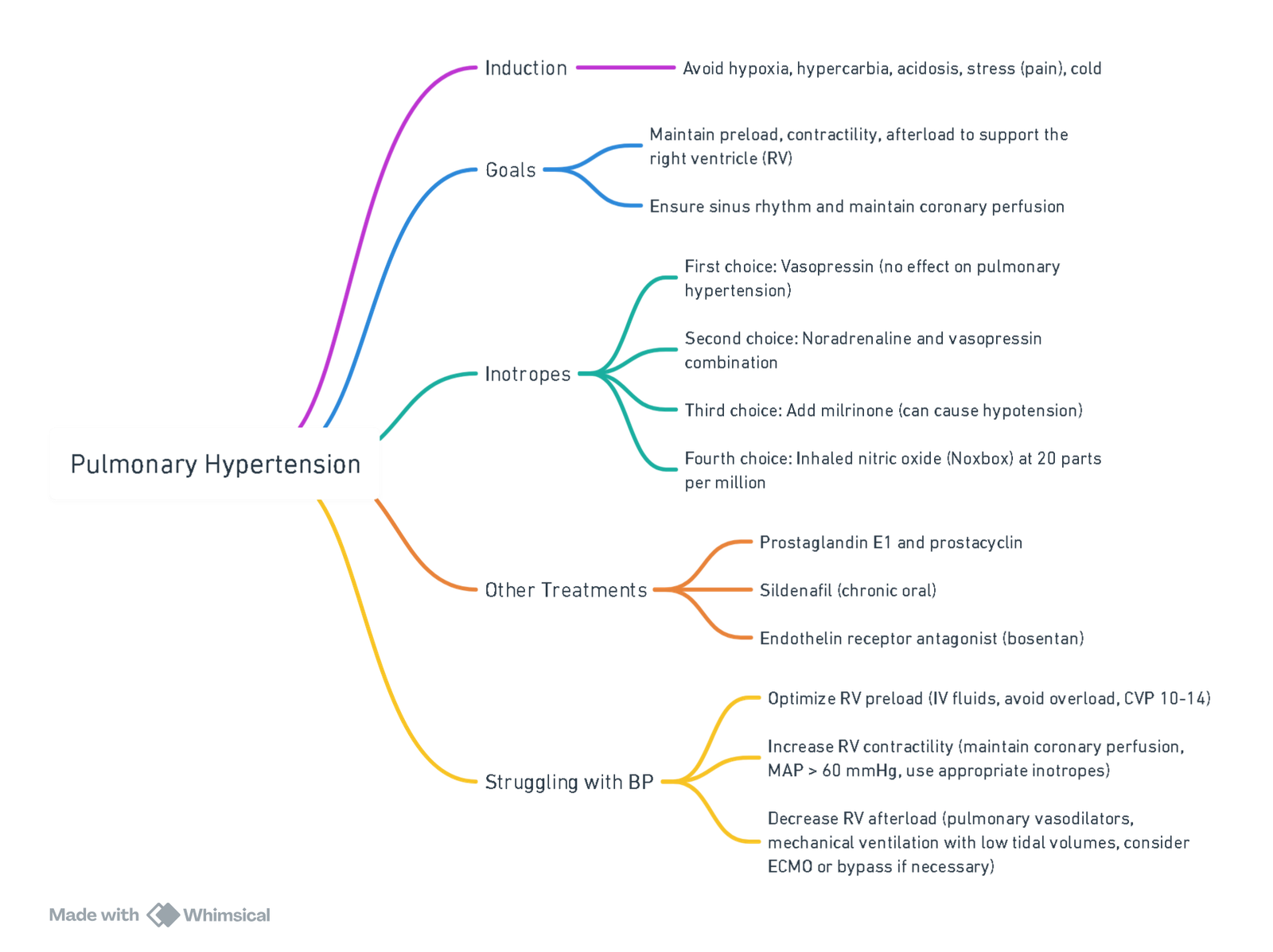
View or edit this diagram in Whimsical.
CABG
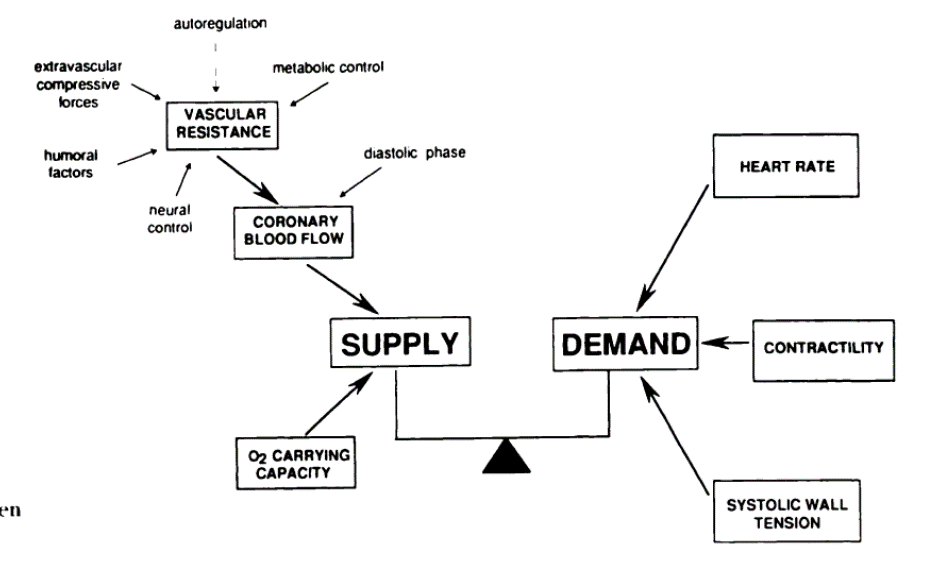
- Optimise Supply demand ratio above
- Coronary perfusion pressure = Aortic diastolic BP–LVEDP
- Slow heart rate (Pain)
- High perfusion pressure
- Don’t raise LVEDP, don’t overload, but avoid hypovolaemia
- Optimize Carrying capacity (HB, Sats, CO)
- Cannot change arteries
Important TOE Views
Mid-Esophageal (ME) Views
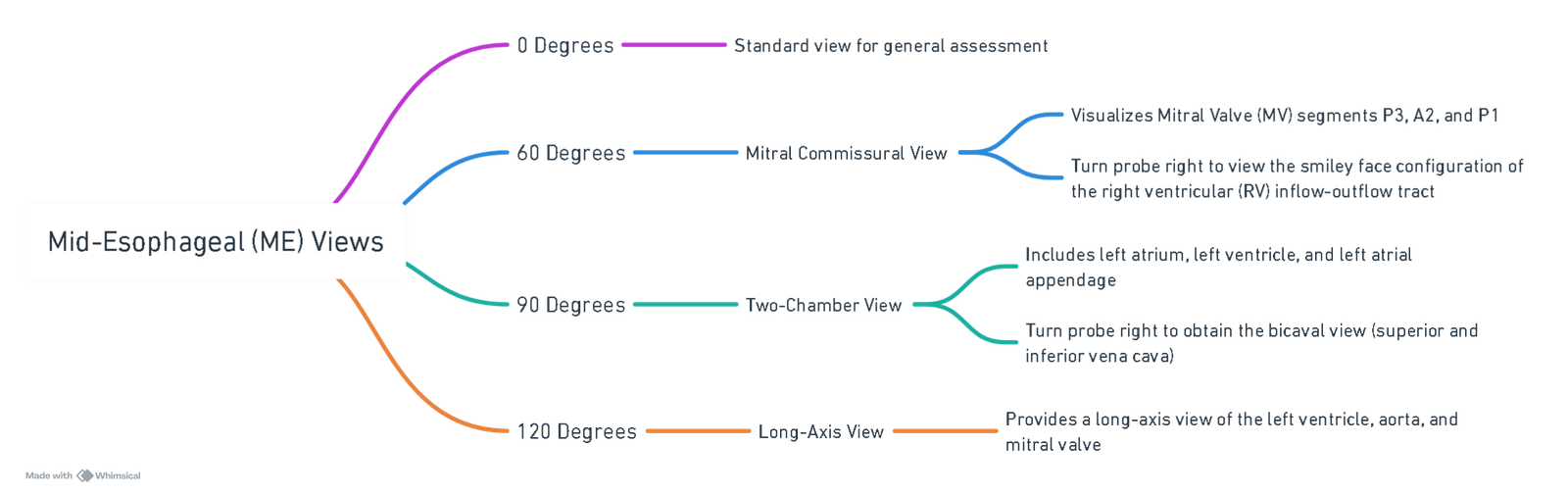
View or edit this diagram in Whimsical.
Cardioplegia
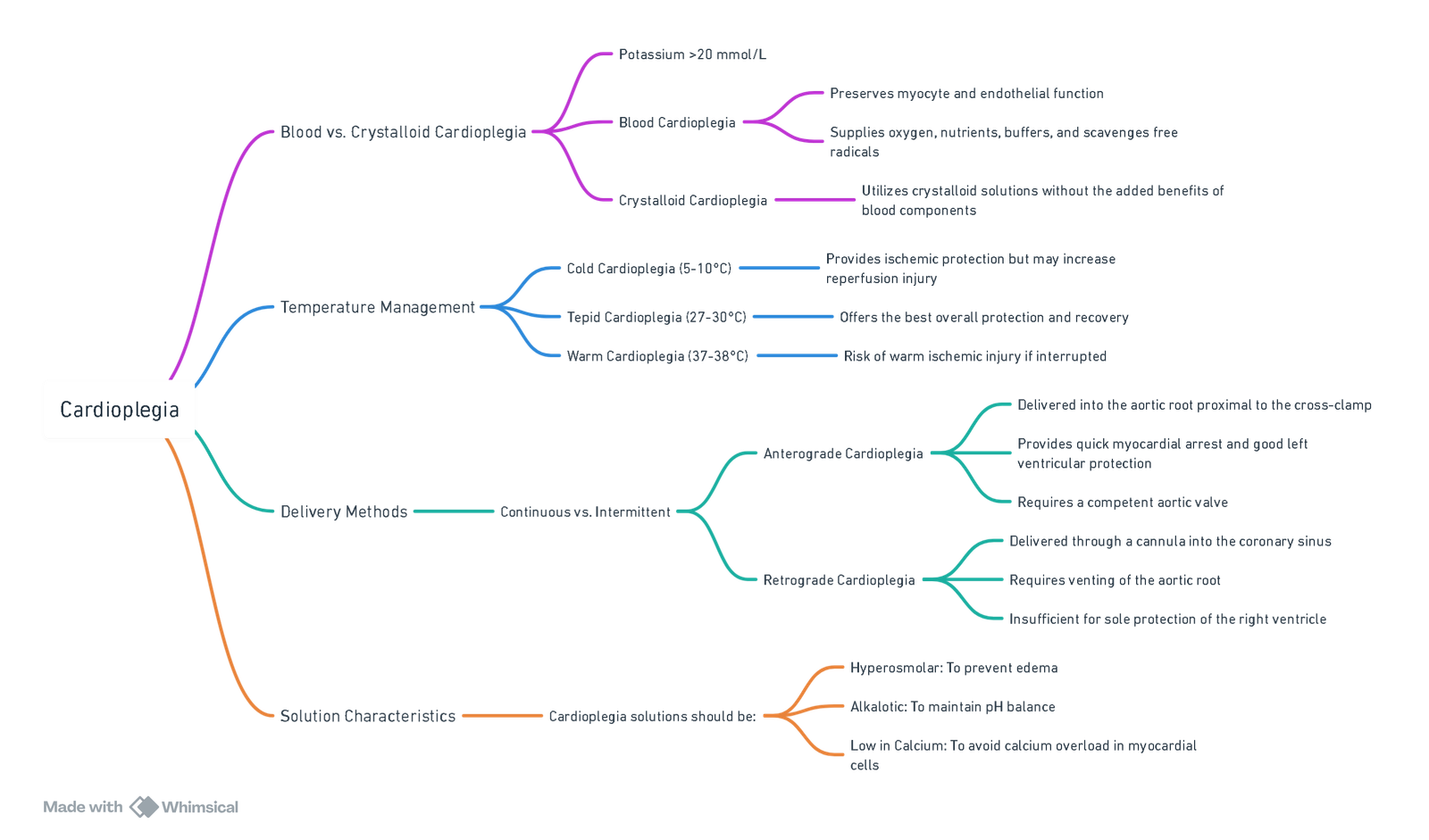
View or edit this diagram in Whimsical.
Links
- Cardiac physiology
- Paediatric congenital heart disease
- Bypass
- Off Pump CABG
- Coronary artery bypass surgery (CABG)
References:
- Cardiac Anesthesiology Made Ridiculously Simple. Dr. Wallace, A
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries:
Anticoag during bypass
Cardiac
Cardiothoracic
Coagulopathy in cardiac surgery
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “e50a302a-74db-4d62-a4ba-b0e4f44c31cd”



