{}
Off-Pump Coronary Artery Bypass (OPCAB) Surgery
Introduction
- Advantages: OPCAB surgery reduces postoperative complications such as systemic inflammation, myocardial injury, and cerebral injury.
- Potential Benefits: Avoiding cardiopulmonary bypass (CPB) reduces postoperative complications like systemic inflammation, atrial fibrillation, bleeding, kidney dysfunction, and cerebral injury.
- Controversies: Long-term graft patency rates are better with on-pump coronary artery bypass grafting.
- Outcomes in High-Risk Patients: OPCAB shows better outcomes in high-risk patients.
Indications to Convert to Bypass
- Cardiac index < 1.5 L/min/m²
- SvO₂ < 60%
- MAP < 50 mmHg
- ST segment elevation > 2 mV
- Larger new wall motion abnormalities or collapse of LV function on TOE
- Sustained malignant arrhythmias
Conduct of Anaesthesia
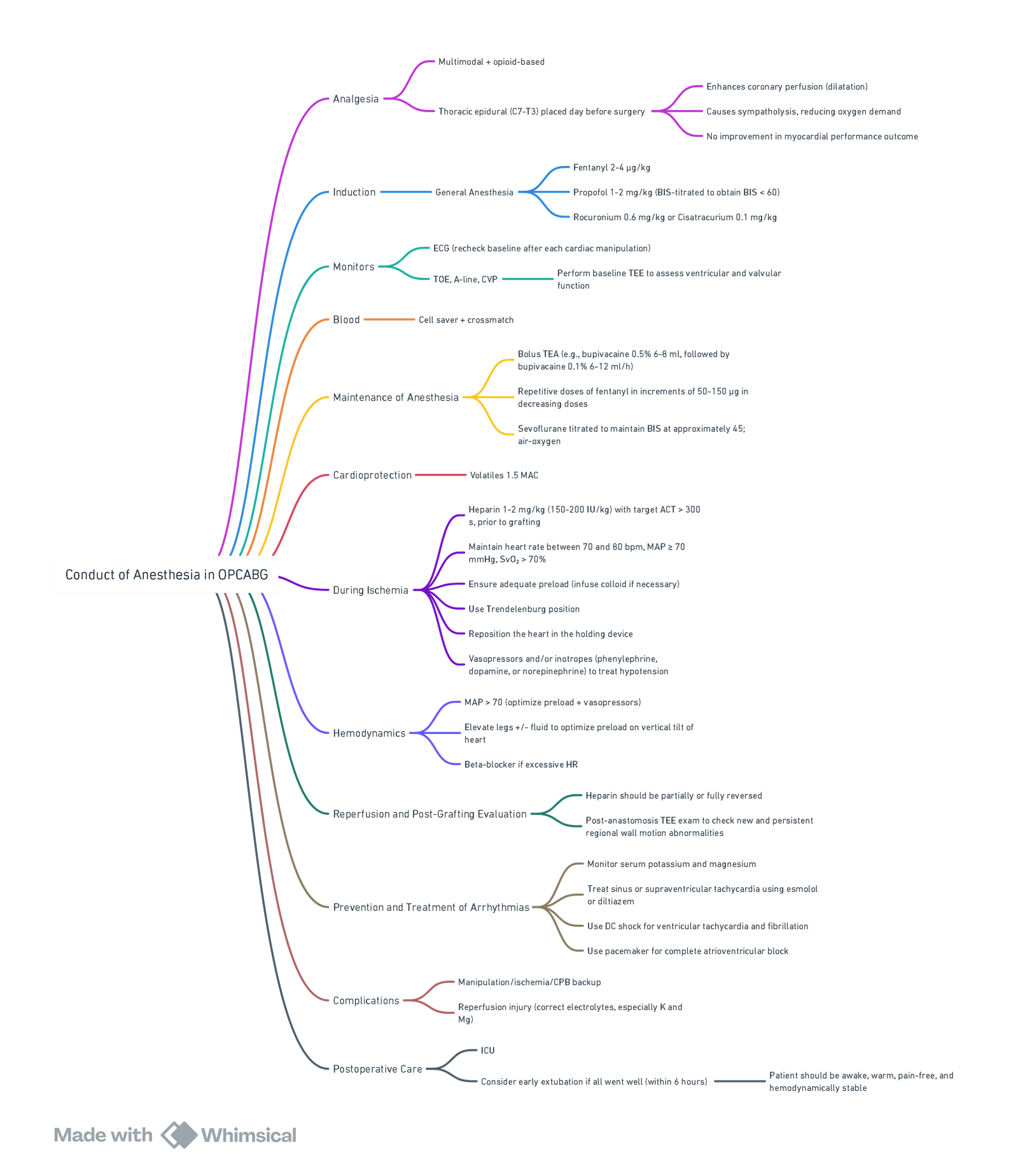
View or edit this diagram in Whimsical.
Preoperative Considerations
Preoperative Anaesthetic Assessment
- Evaluate the patient, risks, and comorbidities.
- Discuss the surgical plan and anesthesia management with the surgeon.
Premedication
- Temazepam (0.5-1 mg/kg per os).
- Atenolol (50 mg per os).
Operating Room Readiness
- CPB machine ready with a perfusionist in attendance.
- Set temperature to 24°C, place a warming pad or mattress on the operating table, use an air warming device.
- External pads connected to a defibrillator (internal pads and a pacemaker should also be available).
Monitoring
- 5-lead surface ECG with automated ST segment analysis.
- Pulse oximetry; unconsciousness monitoring system.
- Radial arterial cannula.
- 4-lumen central line via right internal jugular vein.
- 8.5 F catheter via right internal jugular vein for inserting pulmonary artery catheter (if necessary).
- Stroke volume and pulse pressure variation monitoring.
- Foley catheter.
- Transesophageal echocardiography (TEE), pulmonary artery catheter, esophageal and rectal temperature monitoring.
Coagulation Monitoring
- Activated clotting time (ACT) is commonly monitored. No standardized ACT target value for OPCAB, but ~300 s is accepted by approximately 80% of US/Canadian surgeons and 60% of European surgeons.
Intraoperative Considerations
Anaesthesia Objectives
- Ensure maximum cardiac protection, maintain hemodynamic and cardiac rhythm stability, and promote early ambulation with excellent postoperative analgesia.
Anaesthetic Approaches in OPCAB
-
GA with Opioids and Inhalation Anaesthesia or TIVA
- Volatile anesthetics offer advantages of pharmacological ischemic preconditioning.
- Minimally invasive direct coronary artery bypass (MIDCAB) surgery requires a double-lumen endobronchial tube or a bronchial blocker.
- Cisatracurium/Rocuronium.
- Avoid long-acting opioids; use remifentanil/sufentanil.
- Dexmedetomidine may reduce intraand postoperative opioid consumption.
-
Combined GA with Controlled Ventilation and Neuraxial Blockade (TEA or ITM)
- High TEA attenuates neuro-hormonal response, provides thoracic sympatholysis, ensures hemodynamic stability, decreases myocardial oxygen demand, improves myocardial blood flow, reduces the risk of perioperative arrhythmia and myocardial ischemia, improves renal function, and significantly decreases heart rate.
-
Awake Regional Anaesthesia with Spontaneous Ventilation (TEA Alone)
- Awake OPCAB is a promising modality using combined femoral block/TEA or spinal anaesthesia/TEA.
Hemodynamic Goals
- Adequate Monitoring
- 5-lead ECG, IBP, TOE
- Management of Intraoperative Ischemia
- MAP > 70 mmHg with increased preload and vasopressors.
- Elevate legs and give fluid to treat hypotension from tilting the heart.
- Treat excessive tachycardia with β-blocker.
- Control myocardial O₂ supply/demand.
- Indications to Convert to CPB
- Reperfusion and Post-Graft Evaluation
- Monitor ECG for ischemic changes.
- Check for RWMA on TEE.
- Correct electrolyte abnormalities.
- Use Doppler evaluation of graft patency.
Hemodynamic Challenges
Cardiac Displacement
- Left anterior descending coronary artery (LAD) is usually approached without displacing the heart.
- Multiple coronary revascularizations involving the circumflex or posterior descending artery require significant mobilization and stabilization of the heart.
- Positioning can lead to reduced stroke volume (SV) and arterial blood pressure (ABP), increased central venous pressure (CVP), and right ventricular (RV) end-diastolic pressure.
Hemodynamic Effects
- Vertical Tilt: Atria below ventricles impair diastolic filling and enlarge atria with higher atrial pressures, leading to moderate diastolic dysfunction.
- Compression of Ventricular Wall with Stabilizer Device: Local restriction of movement and reduced lumen size.
- Vertical Positioning: Folding of intracardiac structures at the AV groove distorts the mitral and tricuspid annulus, causing regurgitation.
Pathophysiology
- Compression of the RV free wall against the interventricular septum leads to impaired diastolic filling and obstruction of the RV outflow tract.
- Tilting the heart impairs normal blood flow from the atria to the ventricles, increasing atrial size and filling pressure, reducing cardiac output.
- Distortion of mitral and tricuspid annuli causes regurgitation and enlargement of atria and pulmonary veins.
- Mitral regurgitation is associated with falling peripheral oxygen saturation and myocardial ischemia.
- Trendelenburg positioning to 20° head down improves preload and cardiac output.
- Inotropes and vasopressors (dopamine, epinephrine, norepinephrine) and cautious fluid management are helpful.
- Phenylephrine is indicated when MAP remains low due to reduced peripheral resistance.
- Investigate persistent hypotension with ST segment changes on ECG or TEE for new wall motion abnormalities.
- Surgical procedures like pleuropericardial incision or heart repositioning may stabilize hemodynamics.
- In high-risk patients, consider intra-aortic balloon pump (IABP).
- Conversion to CPB increases morbidity and mortality (8.5-18%).
- Predictors of emergency conversion to CPB include congestive heart failure, redo surgery, low ejection fraction, recent myocardial infarction, mitral regurgitation, and chronic obstructive pulmonary disease.
Management of Ischemia
- Temporary occlusion of the target coronary artery may be used for precise anastomosis.
- Maintain hemodynamic stability, reduce myocardial oxygen consumption, and provide myocardial protection during distal anastomosis.
- Maintain MAP > 70 mmHg with fluid loading, Trendelenburg position, vasopressors, and inotropes.
- The severity of coronary artery stenosis influences hemodynamic response; modest stenosis produces significant changes when occluded, while severe stenosis produces little change.
- Changes in SvO₂ and PaCO₂ are associated with changes in SjO₂.
- Maintain SvO₂ > 70% to prevent cerebral blood flow reduction.
- Maintain heart rate between 70-80 bpm; treat tachycardia with esmolol or diltiazem.
Prophylactic anti-arrhythmic agents (lidocaine, magnesium) may be used.
- Prophylactic β-blockers reduce the incidence of postoperative atrial fibrillation (POAF).
- The use of magnesium for POAF prevention is controversial.
Summary
- Improvement of Myocardial O₂ Balance
- Decrease HR/contractility with β-blockers or CCBs.
- Maintain CPP with MAP.
- Ischemic Preconditioning: Intermittent release of coronary artery clamp.
- Pharmacological Preconditioning: Volatiles at 2 MAC 30 minutes before ischemia.
- Pharmacological Prophylaxis
- Continue β-blockers perioperatively, possibly with esmolol.
- CCBs (e.g., diltiazem).
- Magnesium to reduce atrial tachycardia.
- Surgical Shunting
Postoperative Considerations
- Post-revascularization, surface ECG shows significant T-wave inversion; TEE shows new RWMA which may be associated with reperfusion injury and myocardial stunning.
- Persistent and severe new RWMA are prognostic for postoperative cardiac complications and adverse outcomes.
- Ultra-fast-track anesthesia with immediate patient extubation in OPCAB is feasible and likely safe.
- Immediate extubation requires a stable, warm, normovolemic, pain-free, and alert patient at the end of surgery; neuromuscular blockade should be reversed.
Links
References:
- Hemmerling, Thomas M.; Romano, Gianmarco; Terrasini, Nora; Noiseux, Nicolas.Anesthesia for off-pump coronary artery bypass surgery. Annals of Cardiac Anaesthesia 16(1):p 28-39, January–March 2013. | DOI: 10.4103/0971-9784.105367
Summary or mindmap:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “7d6a4755-6a51-47c9-b5ab-6261777f01ca”



