- Anaesthesia for CABG
- Salient Points for Anaesthesia in CABG
- Neuroprotection during CABG
- Coronary Artery Bypass Graft Indications
- Recommendations from the American Heart Association (AHA)
- General Recommendations
- Recommendations for Medication Management in Cardiac and Noncardiac Surgery
- Peri-operative Anti-platelet Management
- Management Options for Patients on Dual Antiplatelet Therapy (DAPT)
- Peri-operative Monitoring
- Peri-operative Optimization
- Preconditioning and Management of Myocardial Ischemia
- Prevent Morbidity and Mortality
- Links
{}
Anaesthesia for CABG
Salient Points for Anaesthesia in CABG
Preoperative Assessment
- Number and Location of Vessels: Determine how many and which vessels will be grafted.
- Grafts: Identify the sources of grafts (e.g., internal mammary artery, saphenous vein) to guide line placement.
- Left Ventricular (LV) Function: Assess LV function to understand the patient’s cardiac performance and tailor anesthesia management.
- Valve Disease: Evaluate for any concomitant valve disease that may affect surgical and anesthetic management.
Risk Assessment
- Mortality, CVA, and MI Risk: Mortality, cerebrovascular accident (CVA), and myocardial infarction (MI) risk around 2-4%.
- Postoperative Cognitive Dysfunction (POCD): Incidence in patients >60 years old is approximately 26%.
Lines and Monitoring
- Arterial Line (A-line) and Drips: Placement depends on the graft harvest site. Ensure appropriate arterial access for continuous blood pressure monitoring and blood sampling.
Critical Events Management
- MAP Management: Maintain mean arterial pressure (MAP) <70 mmHg prior to aortic cannulation to reduce the risk of aortic dissection.
Cardiac Protection
- Use of Volatiles: Volatile anaesthetic agents are recommended for their cardioprotective effects during cardiac surgery.
Neuroprotection during CABG
Non-Pharmacological Strategies
Reduce Embolic Load
- Epiaortic Ultrasound (US): Visualization of atheromatous plaques on the aorta helps guide surgical manipulation to reduce the risk of embolization.
- Pericardial Suction Aspirate: Contains a high fat load, necessitating the use of inline arterial filtering to remove potential emboli.
- CO₂ Insufflation of Mediastinum: CO₂ is 50 times heavier and 25 times more soluble than air. CO₂ emboli have a shorter lifespan, reducing the risk of embolic complications.
Optimizing Brain Tissue Oxygen Tension
- Pulsatile Flow in CPB: Utilizing pulsatile flow during cardiopulmonary bypass (CPB) can enhance cerebral perfusion and oxygenation.
Avoidance of CPB During Cardiac Surgery
- Off-Pump CABG: Performing coronary artery bypass grafting (CABG) without CPB may reduce the incidence of stroke in high-risk populations, although the difference was not statistically significant.
Maintenance of Cerebral Perfusion Pressure (CPP)
- Mean Arterial Pressure (MAP): Traditionally, a minimum MAP of 50 mmHg is recommended. However, studies indicate that maintaining a higher MAP (>70 mmHg) is associated with lower stroke and myocardial infarction outcomes, particularly in high-risk individuals.
Hemoglobin Management
- Transfusion Trigger: A hemoglobin level of 7 g/dL is recommended as the trigger for blood transfusion to maintain adequate oxygen delivery.
Hypothermia
- Evidence: There is little evidence supporting the routine use of hypothermia for neuroprotection during CABG. This may be due to the absence of hypothermia during critical periods of risk or inadvertent hyperthermia during rewarming.
Glycemic Control
- Management: Maintaining optimal blood glucose levels is crucial to reduce the risk of perioperative complications, including neurological events.
Acid-Base Management
- Alpha Stat Method: The alpha stat method of acid-base management has been shown to reduce the embolic load compared to other methods, providing potential neuroprotective benefits.
Coronary Artery Bypass Graft Indications
- Assess Surgical Risk and Comorbidities
- Individual management plan for patients with comorbidities that increase mortality.
- Assess risk with heart team including a cardiac surgeon and interventional cardiologist (SYNTAX Trial).
- Use Society of Thoracic Surgeons Score, EuroSCORE, or SYNTAX II Score to predict patient outcome with anatomy, disease severity, and preoperative characteristics.
-
Symptomatic Multivessel (≥ 3 Vessels) or Complex VCAD
- Complex CAD includes stenosed vein grafts, bifurcation lesions, calcified lesions, total occlusions, ostial lesions.
-
Acute Coronary Syndrome (ACS)
- STEMI Initial Treatment: PCI/Thrombolysis
- Rapid reperfusion to myocardium most important in STEMI to decrease myocardial damage.
- NSTEMI or Unstable Angina (UA) with MVCAD involving at least three vessels including the proximal left anterior descending (LAD):
- CABG can be considered for residual stenoses 6-8 weeks later.
- ↑ Survival
- STEMI Initial Treatment: PCI/Thrombolysis
-
Left Main Coronary Artery Disease
- Left Main Coronary Artery divides into Left Anterior Descending (LAD) and Left Circumflex (LCx) which supplies 2/3 of myocardium.
- Myocardial infarction from left main artery occlusion: Death
- Left main stenosis: Ventricular Dysrhythmias, Ongoing Ischemia, LV Dysfunction, Hemodynamic Instability.
- Left Main Coronary Artery divides into Left Anterior Descending (LAD) and Left Circumflex (LCx) which supplies 2/3 of myocardium.
-
Multivessel (≥ 3 Vessels) CAD and Diabetes
- ↑ Risk of cardiovascular disease in diabetes
- ↑ Risk of atherosclerosis, hyperglycemia, and dyslipidemia.
- CABG bypasses several atherosclerotic plaques in coronary arteries.
- ↑ Durability
- Complete perfusion
- CABG has mortality benefit
-
Cardiac Surgery Required for Other Pathology
- Revascularization indicated along with other cardiac surgery:
- Valve Stenosis or Regurgitation
- Septal Defect
- Aortic Root or Arch Pathology
- Combination Procedure: ↑ Number of Operations
- Revascularization indicated along with other cardiac surgery:
-
Multivessel CAD, LV Dysfunction, and Congestive Heart Failure (CHF)
- Multivessel CAD with >90% Stenosis and CHF
- Evidence of Ischemia at Rest
- LV Ejection Fraction < 35%
- Evidence of Impaired LV Function at Rest
- ↑ All-cause Mortality in CABG vs Medical Management
- Multivessel CAD with >90% Stenosis and CHF
-
Coronary Artery Bypass Graft Recommended
- Consider revascularization (restore blood flow to blocked or narrowed blood vessels) of coronary arteries to increase perfusion to myocardium (heart muscle).
Additional Factors Influencing CABG Indications
Chronic Obstructive Pulmonary Disease (COPD)
- ↑ Inflammation and deregulated angiogenesis affects all organ systems.
- ↑ Pneumonia
- ↑ Respiratory and Renal Failure
- ↑ Stroke
Frailty
- ↓ Physiologic reserve and ability to recover from acute stress.
- ↑ In-hospital Mortality
- ↓ Survival Two Years After Surgery
Chronic Renal Failure
- Cardiopulmonary bypass, fluid overload, ↑ renal vasoconstriction, and renal oxygenation from rewarming.
- Kidney Injury
- End-stage Kidney Disease
Outcomes of CABG
- Blood flow restored to ischemic myocardium:
- ↓ Angina
- ↑ Quality of Life
- ↑ LV Function
- ↑ Survival
Recommendations from the American Heart Association (AHA)
General Recommendations
Class I
- Early extubation and accelerated recovery for low to medium risk patients.
- Optimal analgesia and patient comfort through multidisciplinary efforts.
- Improved communication between disciplines using checklists.
- Fellowship-trained cardiac anaesthetist credentialed in the use of transesophageal echocardiography (TOE) for high-risk patients.
Class IIa
- Use of volatile-based regimen to facilitate early extubation and decrease recall.
Recommendations for Medication Management in Cardiac and Noncardiac Surgery
| Medication | Surgery Type | Drug-naïve Patients | Chronically Treated Patients |
|---|---|---|---|
| Renin-Angiotensin-Aldosterone System Blockers (RAASB) | Cardiac | No definite recommendations | Discontinue before surgery (COR, I; LOE, C) |
| Noncardiac | Start therapy at least 1 week before surgery for cardiac-stable patients with heart failure and left ventricular systolic dysfunction (COR, IIa; LOE, B) | Continuation of ACE inhibitors or ARBs perioperatively is reasonable (COR, IIa; LOE, B) | |
| Statins | Cardiac | Do not initiate before surgery (COR, III; LOE, A) | Continue statin therapy (COR, IIa; LOE, C) |
| Noncardiac | Start therapy at least 2 weeks before vascular surgery (COR, IIa; LOE, B) | Continue perioperative therapy (COR, I; LOE, C) | |
| Beta-blockers | Cardiac | Low-dose therapy 2-3 days before surgery for atrial fibrillation prophylaxis (COR, IIa; LOE, B) | Continue therapy before surgery (COR, IIa; LOE, B) |
| Noncardiac | Do not administer on the day of surgery or to patients undergoing low-risk surgery (COR, III; LOE, B) | Continue therapy before surgery (COR, I; LOE, B) | |
| Aspirin | Cardiac | Do not start before surgery (ATACAS trial) (COR, I; LOE, B) | Continue throughout the preoperative period for CABG surgery (COR, IIa; LOE, C). Stop at least 5 days before non-CABG surgery or for cases of high bleeding risks (COR, IIa; LOE, C) |
| Noncardiac | Do not administer before surgery (COR, III; LOE, B) | Continue aspirin when the risk of potential increased cardiac events outweighs the risk of increased bleeding (COR, IIb; LOE, B) | |
| Alpha-2 Agonists | Cardiac | No definite recommendations | Not used long term |
| Noncardiac | Do not administer before surgery (COR, III; LOE, B) | Not used long term |
Peri-operative Anti-platelet Management
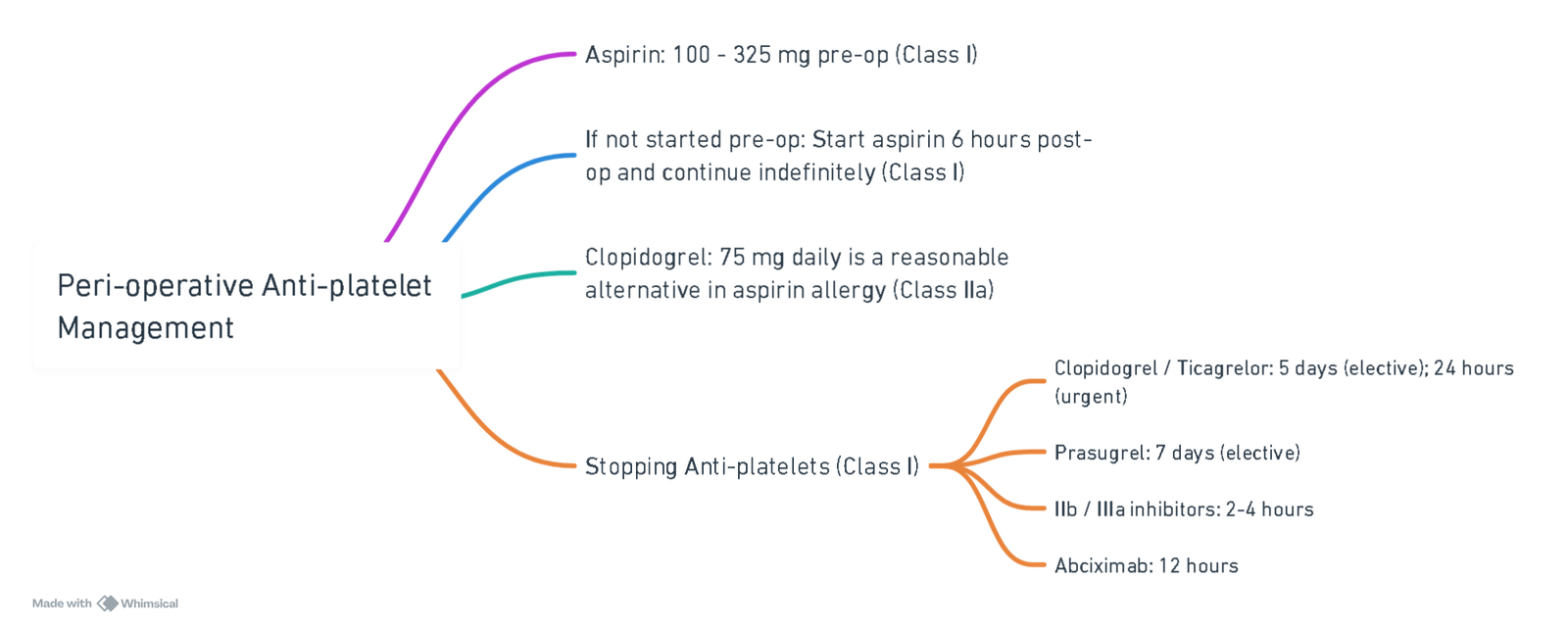
View or edit this diagram in Whimsical.
Management Options for Patients on Dual Antiplatelet Therapy (DAPT)
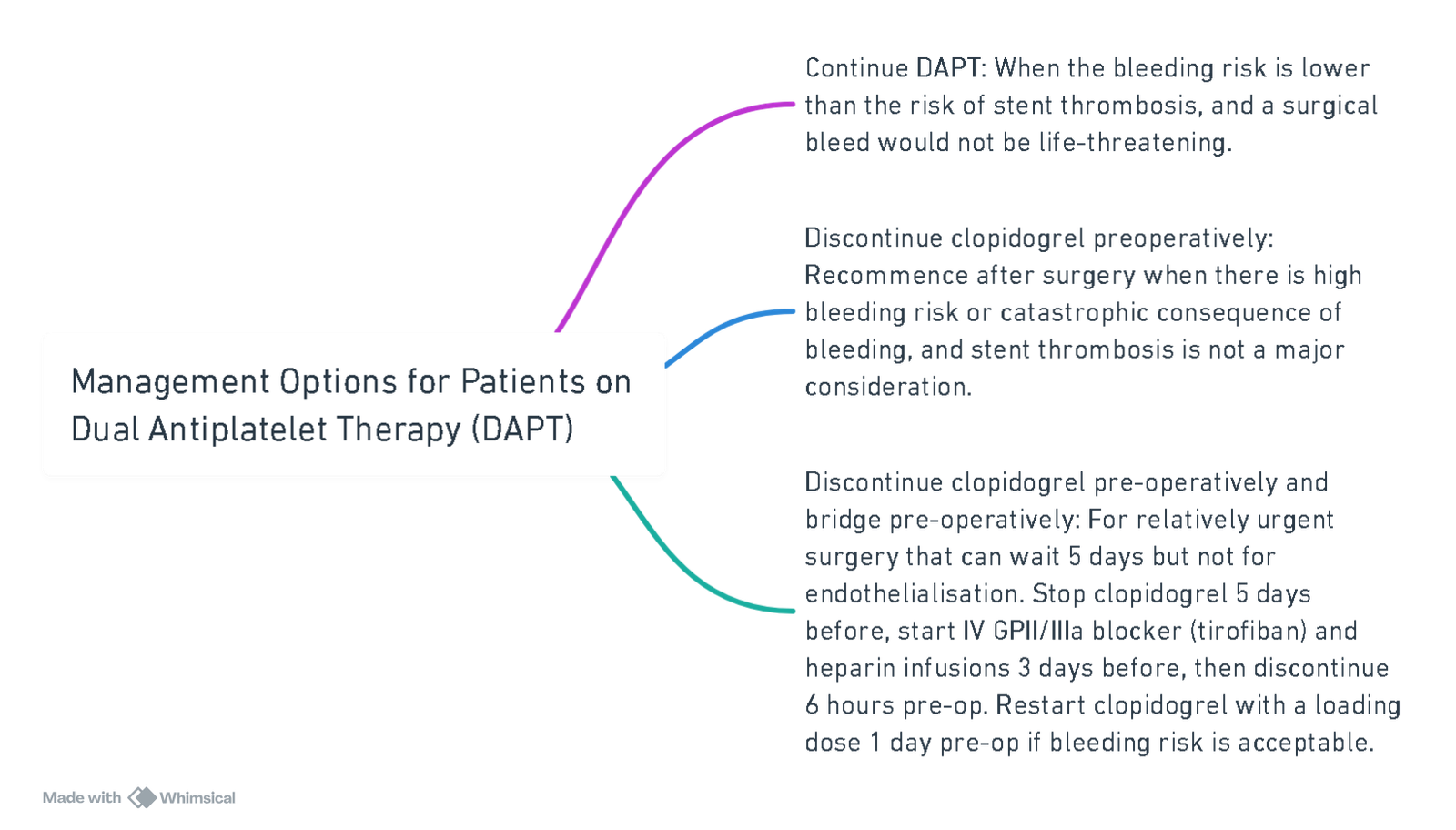
View or edit this diagram in Whimsical.
Summary of Drug Management in Cardiac Surgery
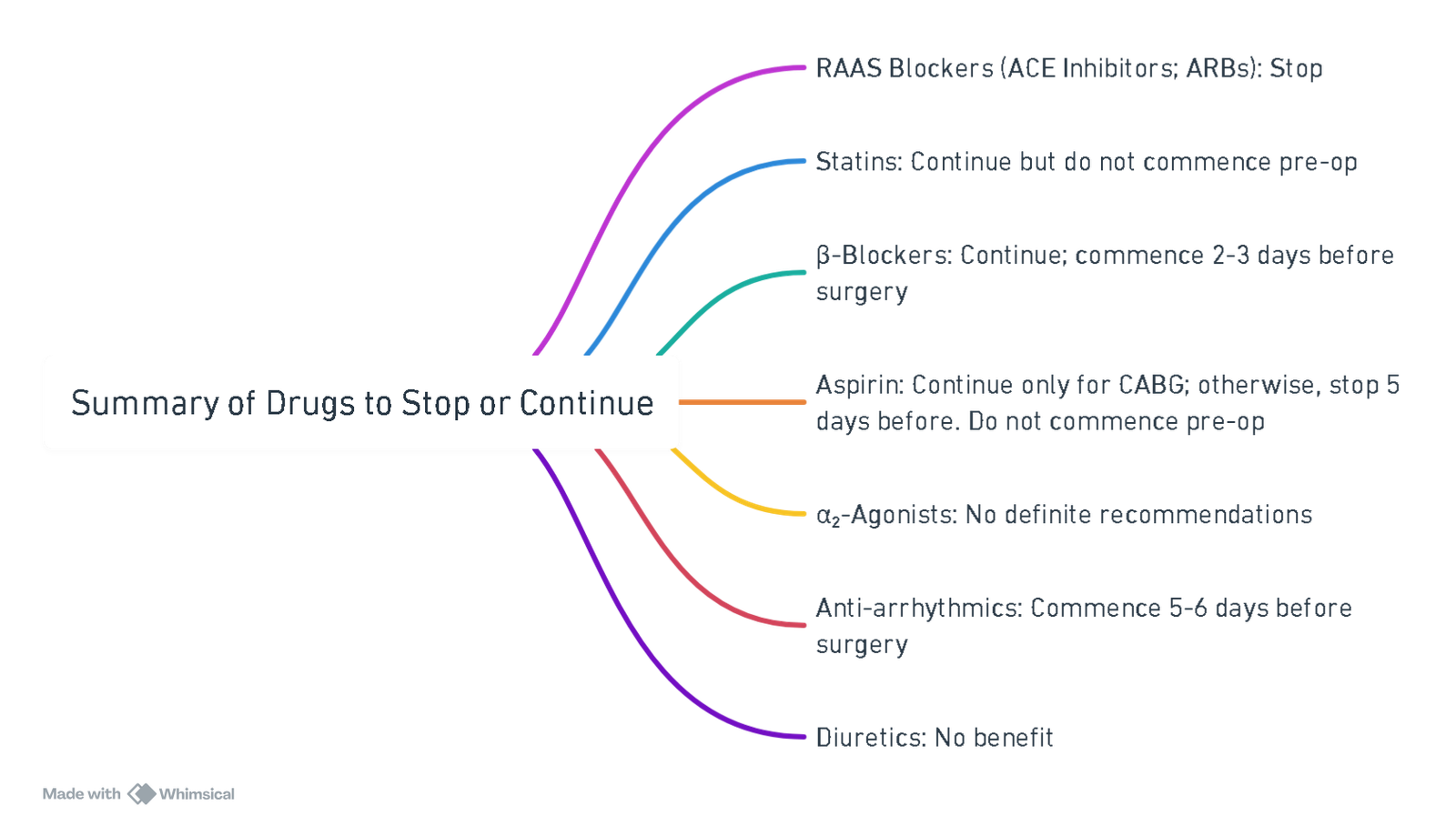
View or edit this diagram in Whimsical.
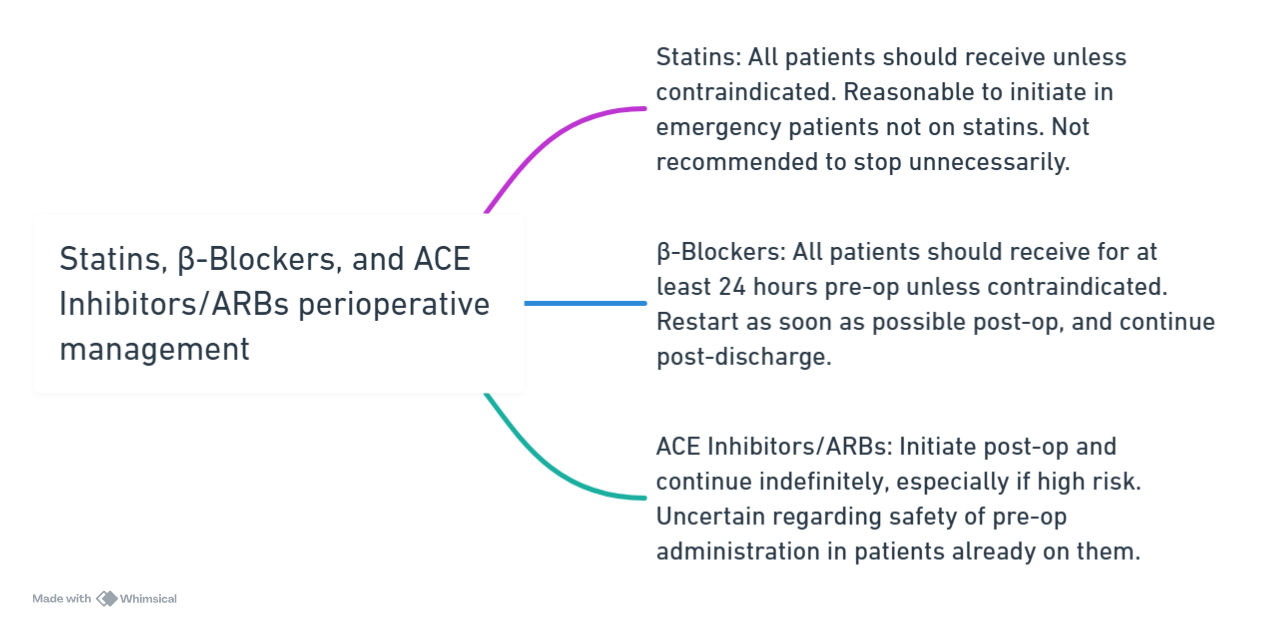
View or edit this diagram in Whimsical.
Peri-operative Monitoring
- ECG: Intra-op ST-segment monitoring, post-op for 48 hours continuously.
- PAC: Indicated pre-induction for cardiogenic shock. Useful intra-op and early post-op in hemodynamically unstable patients. Reasonable for stable patients.
- CNS Monitoring: Uncertain effectiveness of processed EEG or NIRS.
Peri-operative Optimization
- Antiplatelet management.
- Hyperlipidemia management.
- β-Blocker management.
- ACE / ARB management.
- Smoking cessation.
- Emotional: Depression management.
- Cardiac rehabilitation.
- Monitoring.
- Hormonal: Insulin infusion to maintain glucose ≤ 180 mg/dL without causing hypoglycemia.
Preconditioning and Management of Myocardial Ischemia
- Optimize determinants of coronary perfusion (HR, DAP, MAP, RVEDP, LVEDP) (Class I).
- Use volatile-based anesthesia to reduce risk of peri-op MI (Class IIa).
- Consider mechanical preconditioning in OPCAB (Class IIb).
- Consider remote preconditioning to attenuate reperfusion injury (Class IIb).
- Uncertain effectiveness of pharmacological therapies, controlled reperfusion, or post-conditioning (Class IIb).
Prevent Morbidity and Mortality
- Infection: Pre-op antibiotics, aggressive debridement of sternal wound infection, insulin infusion targeting ≤ 180 mg/dL glucose.
- Renal Dysfunction: OPCAB may be reasonable in renal dysfunction. Maintain MAP > 60 and Hct > 19% during on-pump procedures.
- Myocardial Dysfunction: IABP in high-risk patients if not contraindicated; measure biomarkers for 24 hours post-op.
- Dysrhythmias: β-Blockers as primary treatment; amiodarone if contraindicated.
- Bleeding: Lysine analogues; multimodal approach with transfusion algorithms, point-of-care (POC) testing, and focused blood conservation strategies.
- Non-invasive carotid artery screening.
- Epiaortic ultrasound.
- Public reporting of outcomes.
Links
References:
- Anaesthesia refresher University of Cape Town 2008. Nieuwveld
- Basagan-Mogol E, Goren S, Korfali G, Turker G, Kaya FN. Induction of anesthesia in coronary artery bypass graft surgery: the hemodynamic and analgesic effects of ketamine. Clinics (Sao Paulo). 2010 Feb;65(2):133-8. doi: 10.1590/S1807-59322010000200003. PMID: 20186295; PMCID: PMC2827698.
- Luxford, J., Bassin, L. (2017). Anesthesia for Coronary Artery Bypass Graft (CABG). In: Aglio, L., Urman, R. (eds) Anesthesiology. Springer, Cham. https://doi.org/10.1007/978-3-319-50141-3_13
Summaries:
Calgary CABG indications
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “82502709-b742-4416-9a82-c3f27ff068dd”



