- Acute Coronary Syndrome
- Perioperative Myocardial Infarction (MINS)
- Management of Antiplatelet Therapy
- Biomarkers
- Links
{}
Acute Coronary Syndrome
- Major non-cardiac surgery is associated with an incidence of perioperative cardiac death of 0.5–1.5% and major cardiovascular complications (e.g., myocardial infarction, heart failure, and stroke) of 2–3.5%.
Definitions
- Acute Coronary Syndrome (ACS): A spectrum of conditions characterized by varying myocardial ischemic states.
- ACS is broadly categorized based on evidence of myocardial ischemia on an electrocardiogram (ECG) and myocardial necrosis from serum levels of cardiac biochemical markers (e.g., troponin):
- ST-Elevation Myocardial Infarction (STEMI)
- Non-ST-Elevation ACS (NSTE-ACS):
- Non-ST-Elevation Myocardial Infarction (NSTEMI) (associated troponin rise)
- Unstable Angina (no myocardial cell necrosis/troponin increase)
- ACS is broadly categorized based on evidence of myocardial ischemia on an electrocardiogram (ECG) and myocardial necrosis from serum levels of cardiac biochemical markers (e.g., troponin):
- In general, STEMI is associated with more prolonged duration of ischemia and a larger territory of myocardial necrosis (e.g., after a complete coronary artery occlusion) than NSTEMI.
- The short-term mortality from STEMI is marginally higher than that from NSTEMI, but the 4-year mortality rate for patients with NSTEMI is twice that of STEMI patients.
STEMI
- Definition: New ST-elevation at the J-point in two contiguous leads with the cut-points:
- ≥1 mm in all leads other than leads V2-V3.
- Following cut-points apply for leads V2-V3:
- ≥2 mm in men ≥40 years.
- ≥2.5 mm in men <40 years.
- ≥1.5 mm in women regardless of age
- or new onset left bundle branch block (LBBB) is indicative of STEMI
- NSTE-ACS usually presents as ST-segment depression or T-wave inversion. The ECG may be normal, especially if the pain has resolved.
Risk Factors
-
Non-Modifiable:
- Advancing age
- Male gender
- Family history of premature coronary artery disease (males <55 years and females <65 years)
- Premature menopause
- Ethnicity (e.g., higher risk in individuals from the Indian subcontinent)
-
Modifiable:
- Smoking
- Diabetes mellitus
- Hypertension
- Obesity
- Sedentary lifestyle
- High cholesterol, specifically a high ratio of low-density to high-density lipoprotein
Management of ACS
STEMI
Initial Steps
- Offer aspirin (unless already given).
- Assess eligibility for reperfusion therapy:
- Eligible: Proceed to next steps.
- Not eligible: Offer medical therapy.
Eligibility Assessment
- Presentation within 12 hours of symptom onset?
- Yes: Proceed to PPCI assessment.
- No: Check for continuing ischaemia.
- Continuing ischaemia?
- Yes: Consider angiography/PCI.
- No: Offer medical therapy.
- Continuing ischaemia?
Primary Percutaneous Coronary Intervention (PPCI)
- PPCI anticipated within 120 min of potential fibrinolysis?
- Yes: Activate PPCI pathway.
- PPCI Pathway:
- Transfer to PPCI centre immediately.
- Do not offer routine glycoprotein inhibitors/fibrinolysis.
- Offer additional antiplatelet agents (choose one):
- Clopidogrel
- Prasugrel
- Ticagrelor
- Take to catheter laboratory for angiography and coronary angiography.
- Offer bivalirudin or heparin (UFH or LMWH).
- Consider radial over femoral access.
- Consider thrombus aspiration.
- PPCI Pathway:
- No: Offer fibrinolysis with antithrombin.
- Yes: Activate PPCI pathway.
Fibrinolysis
- Offer in compliance with NICE.
- Post-fibrinolysis Electrocardiogram (60–90 min after)
- Residual ST-segment elevation (failed reperfusion):
- Offer immediate angiography (with follow-on PCI if indicated). Do not repeat fibrinolysis.
- No residual ST-segment elevation (successful reperfusion):
- Clinically stable: Consider angiography during the same hospital admission.
- Recurrent myocardial ischaemia: Seek specialist cardiological advice and consider coronary angiography with follow-on PCI if indicated.
- Residual ST-segment elevation (failed reperfusion):
Secondary Prevention and Support
- Offer written and oral information, advice, support, and treatment on related conditions and secondary prevention (including lifestyle advice) as per NICE guidelines.
NSTEMI and UA
NICE Guidelines 2010: Early Management for Unstable Angina and NSTEMI
Initial Treatment Steps
- Aspirin:
- Offer a single loading dose of 300 mg and continue indefinitely.
- Antithrombin Therapy:
- Fondaparinux if no high bleeding risk and angiography planned within 24 h.
- Unfractionated heparin if angiography likely within 24 h or if creatinine > 265 µmol/L.
- Adjust dose to clotting function.
- Risk Assessment:
- Use scoring systems such as GRACE to predict 6-month mortality.
- Assess future adverse cardiovascular events, bleeding risk, and comorbidities.
Factors for Assessing
- Full clinical history
- Physical examination
- Twelve-lead resting ECG
- Blood tests (troponin I or T, creatinine, glucose, hemoglobin)
Factors Associated with High Bleeding Risk
- Increasing age
- Known bleeding complications
- Renal impairment
- Low body weight
Risk Categories and Management
- Lowest Risk (<1.5%)
- Management:
- Initial conservative management.
- If recurrent spontaneous ischaemia, proceed to coronary angiography.
- Low Risk (1.5–3.0%)
- Management:
- Single 300-mg loading dose of clopidogrel and continue for 12 months.
- Intermediate Risk (3.0–6.0%)
- Management:
- Single 300-mg loading dose of clopidogrel and continue for 12 months.
- Consider additional antiplatelet (GPI or bivalirudin) based on ischemic vs bleeding risk.
- Offer coronary angiography with follow-on PCI if indicated.
- High Risk (6.0–9.0%)
- Management:
- Same as intermediate risk but prioritize angiography if unstable.
- Highest Risk (>9.0%)
- Management:
- Single 300-mg loading dose of clopidogrel and continue for 12 months.
- Consider additional antiplatelet (GPI or bivalirudin) based on ischemic vs bleeding risk.
- Offer coronary angiography with follow-on PCI if indicated.
Post-Angiography
- PCI (Percutaneous Coronary Intervention):
- Consider abciximab if not on GPI.
- Offer unfractionated heparin to patients on fondaparinux.
- Consider bivalirudin as an alternative.
- CABG (Coronary Artery Bypass Grafting):
- Stop clopidogrel 5 days before CABG.
- Offer surgery to patients with adverse cardiovascular events.
Additional Considerations
- Discuss management strategy with an interventional cardiologist and cardiac surgeon.
- Consider comorbidities, risks, and benefits when discussing revascularization strategies.
Drugs Used in the Treatment of ACS
| Drug Class | Mode of Action | Usage | Note |
|---|---|---|---|
| Aspirin | COX-1 inhibition. Irreversibly prevents Thromboxane A2 production in platelets | 300 mg loading dose to all patients with ACS. 75 mg daily dosage as effective in long term with fewer side-effects | Incidence of allergy <0.5%. No use with NSAIDs – can block effects of aspirin and their COX-2 inhibition is pro-thrombotic |
| Nitrates | Vasodilators—reduce cardiac preload, IV end-diastolic volume and thus myocardial oxygen demand. Dilate coronary arteries | For all patients with suspected coronary ischaemia, acute, and chronic use. IV more effective | No high-level evidence to show reduction in infarct size, major cardiac events, or outcome improvement. |
| Beta-blockers | Reduce myocardial oxygen demand by reducing heart rate, blood pressure and contractility | Recommended for all patients with ischaemia without contraindications | GRAZ database suggests chronic use means less likelihood of STEMI vs NST-ACS, and less c/m release 34% reduction in mortality in NSTI-ACS |
| Calcium-channel blockers | Vasodilatation including coronary arteries. Non-dihydropyridine (e.g. diltiazem, verapamil) slow atrioventricular conduction. | Used where beta-blockade contraindicated in myocardial ischaemia, especially where bradycardia | Avoid combination of verapamil and beta-blockers: can precipitate profound AV node blockade |
| ACE inhibitors | Inhibit conversion angiotensin-1 to angiotensin-II, the latter being a potent vasoconstrictor and inducing aldosterone production. Beneficial effect on cardiac remodelling | Given to all patients with ischaemic heart disease. Should be started as an in-patient wherever possible | Reduce mortality in ischaemic heart disease |
| P2Y12 inhibitors (Clopidogrel) | Pro-drug, metabolized via two cytochrome P450 (CYP450) enzymes in liver to its active metabolite, thus genetic variability and affected by drugs interacting with CYP450 metabolism | Offered to all patients with a GRACE mortality >1.5%, or those likely to have PCI within 24 h. 300 mg loading dose, 75 mg maintenance for 1 yr | Currently recommended by the NICE guidelines for the treatment of STEMI and NSTEMI; however, the European Society of Cardiology guidelines only recommend clopidogrel if prasugrel or ticagrelor are not available or contraindicated |
| Prasugrel | Similar with two step metabolism however first step is plasma esterase, second CYP450. So faster onset and more consistent than clopidogrel | Used in addition to aspirin for patients with STEMI undergoing primary PCI, or in patients with previous stent thrombosis on clopidogrel | Longer duration of action than clopidogrel |
| Ticagrelor | Not a pro-drug, faster onset and more consistent than clopidogrel. Quicker offset than prasugrel | Used in patients with STEMI before angioplasty. May be continued up to 12 months | Higher efficacy with aspirin than clopidogrel with no increase in bleeding risk. Because of this it is the preferred agent in many centres in NSTE-ACS before PCI |
| Glycoprotein IIb/IIIa receptor inhibitors (GIIb/IIIa) | Inhibition of platelet aggregation by antagonizing their cross-linking | Eptifibatide or tirofiban: considered for all intermediate or high-risk patients if angiography scheduled within 96 h. Abciximab: for all intermediate/high-risk patients as adjunct for PCI who are not already taking GIIb/IIIa inhibitors | Increased risk of bleeding especially in the elderly |
| Anti-thrombin therapy | Thrombin inhibition either indirectly (heparin) or directly (bivalirudin) | Fondaparinux: offered to all NSTE-ACS patients without high bleeding risk. If PCI anticipated within 24 h or renal impairment then unfractionated heparin should be used instead. Bivalirudin is alternative for patients not on GIIb/IIIa having PCI within 24 h | For all patients with ACS, a combination of anti-thrombin with anti-platelet therapy is superior to either therapy alone |
Perioperative Myocardial Infarction (MINS)
Overview
- Timing and Symptoms: Most PMIs occur early after surgery and are often asymptomatic.
- ECG Findings: Commonly preceded by ST-segment depression. ST-elevation is rare (<2% of cases).
- Histological Findings: Both circumferential infarction (due to myocardial oxygen supply mismatch) and transmural infarctions are commonly found.
Mechanisms
- Acute Coronary Syndrome (ACS) due to a Primary Coronary Event:
- Pathophysiology:
- Occurs when coronary plaques rupture or fissure, leading to coronary thrombosis.
- Postoperative increases in catecholamines and cortisol, especially with anaemia, hypothermia, or pain.
- Tachycardia and hypertension post-surgery cause shear stresses, leading to plaque rupture.
- Pro-coagulant and pro-thrombotic state with elevated fibrinogen, factor VIII, von Willebrand factor, increased platelet activation, and decreased protein C and antithrombin levels.
- Classification:
- According to the universal classification of myocardial infarction, this is defined as a type 1 myocardial infarction.
- Pathophysiology:
- Reduced Myocardial Oxygen Supply to Demand Ratio:
- Pathophysiology:
- Associated with intraoperative and postoperative hypotension, hypertension, tachycardia, anaemia, hypoxaemia, hypercarbia, and hypothermia.
- Represents a spectrum from minor myocardial ischaemia with low-level troponin increase to prolonged overt ischaemia in multiple ECG leads, resulting in significant myocardial necrosis and high troponin elevation.
- Classification:
- Defined as a type 2 myocardial infarction.
- Pathophysiology:
Key Points
- PMIs typically occur early post-surgery and are often asymptomatic.
- ECG findings are usually ST-segment depression, with ST-elevation being rare.
- Mechanisms include ACS due to plaque rupture (type 1 MI) and reduced myocardial oxygen supply to demand ratio (type 2 MI).
Management of Antiplatelet Therapy
Surgical Haemorrhagic Risk, Blood Transfusion Requirement, and Type of Surgery
- Low Risk
- Blood Transfusion Requirement: Usually not required
- Type of Surgery:
- Peripheral, plastic, and general surgery biopsies
- Minor orthopaedic, otolaryngology, and general surgery
- Endoscopy
- Eye anterior chamber
- Dental extraction and surgery
- Intermediate Risk
- Blood Transfusion Requirement: Frequently required
- Type of Surgery:
- Visceral surgery
- Cardiovascular surgery
- Major orthopaedic surgery
- Otolaryngology
- Urological surgery
- High Risk
- Blood Transfusion Requirement: Possible bleeding in a closed space
- Type of Surgery:
- Reconstructive surgery
- Intracranial neurosurgery
- Spinal surgery
- Eye posterior chamber surgery
Management Algorithm
ASA (Aspirin)
- Primary Prevention
- Stop ASA for 7-10 days
- Secondary Prevention
- All Other Surgeries
- Continue treatment
- High Risk of Bleeding
- Stop ASA for 7-10 days
- All Other Surgeries
ASA + ADP Inhibitors
- High-Risk Situations:
- <2 weeks PTCA
- <6 weeks MI
- <6 weeks BMS
- <6 months DES
- <12 months DES with increased risk of ST
- Emergency Surgery
- Continue with treatment
- Urgent Surgery
- High risk for bleeding
- Stop ADP inhibitors and ASA
- Bridging therapy
- Intermediate Risk of Bleeding
- Stop ADP inhibitors, continue ASA
- Low risk of bleeding
- Continue with treatment
- High risk for bleeding
- Elective Surgery
- Delay surgery
- Low-Risk Situations
- Stop ADP inhibitors, continue ASA
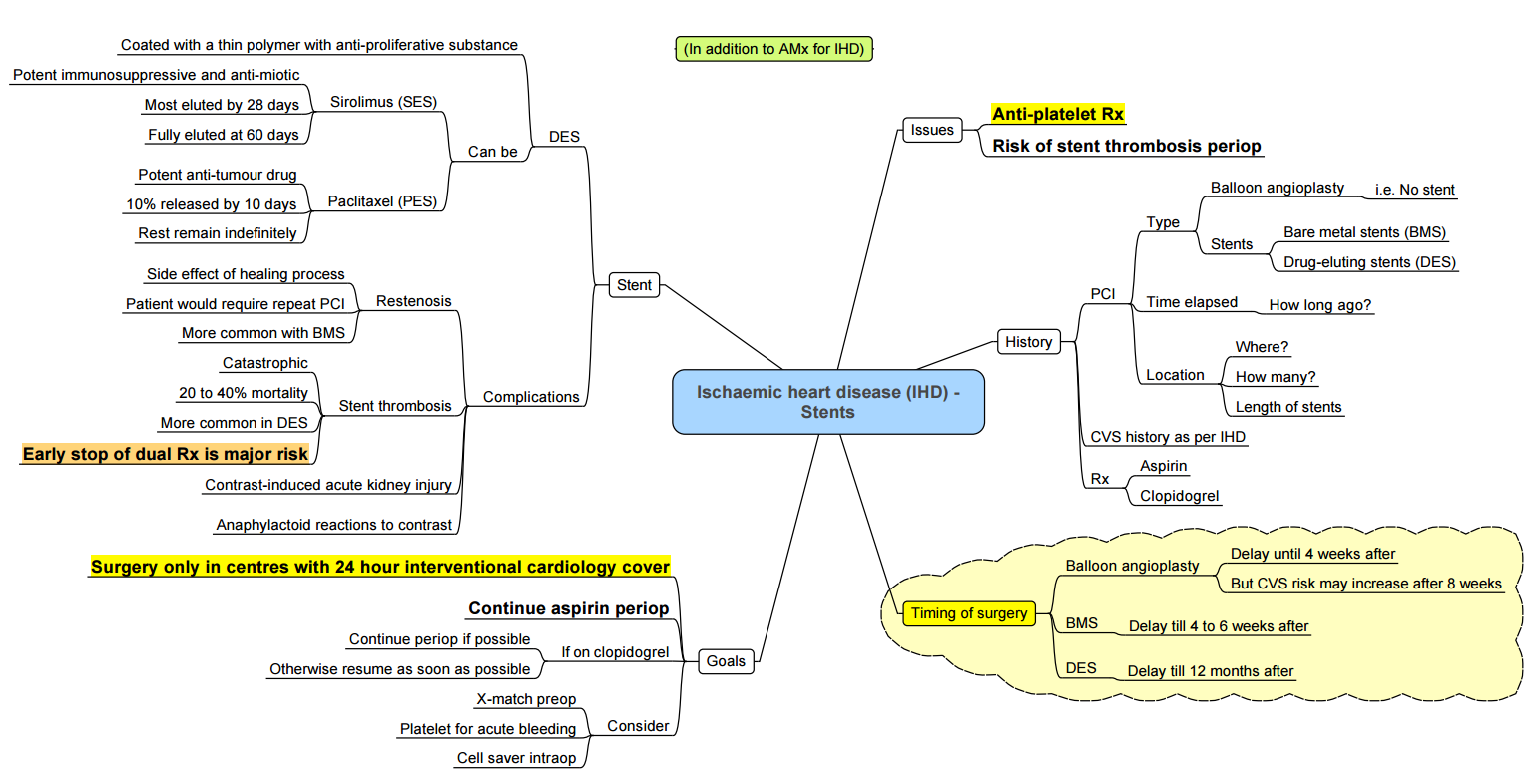
Management of Perioperative Stents
Biomarkers
Significant Studies
VISION Study
- Key Finding: High sensitivity troponin level post non-cardiac surgery is an independent predictor of 30-day mortality.
- Diagnostic Threshold: Peak levels of 0.03 ng/ml are judged to be diagnostic of myocardial injury after non-cardiac surgery (MINS).
2014 Systematic Review by Biccard Et Al
- Key Finding: Post-operative NT-proBNP levels in patients undergoing non-cardiac surgery are the strongest independent predictor of outcomes at 30 days and ≥180 days post-operation.
Canadian Cardiovascular Society Guidelines
- Application: Use NT-proBNP levels for risk stratification in pre-operative cardiac assessment for non-cardiac surgery.
ProBNP
Introduction
- The most commonly used clinical risk stratification tool, the Revised Cardiac Risk Index (RCRI), is recommended by both the American College of Cardiology/American Heart Association (ACC/AHA) and the European Society of Cardiology/European Society of Anaesthesiology (ESC/ESA) guidelines for pre-operative cardiac risk assessment. However, the RCRI misclassifies a substantial number of patients in mixed cohorts of non-cardiac surgical patients.
- The association between pre-operative natriuretic peptides (NPs) and major postoperative cardiovascular complications has been extensively validated in prospective studies.
Pre-operative Natriuretic Peptide Thresholds for Predicting 30-day Mortality and Non-fatal Myocardial Infarction
| Type of Surgery | Type of NP | NP Level (pg/ml) | MACE (%) |
|---|---|---|---|
| Vascular | BNP | 0-29 | 1.2 (0.3-2) |
| 30-115 | 6.5 (4.6-8.4) | ||
| 116-371 | 20.9 (17.7-24.1) | ||
| ≥ 372 | 36.7 (32.9-40.5) | ||
| Mixed Non-cardiac Surgery | BNP | 0-99 | 5.3 (3.2-7.2) |
| 100-250 | 11.6 (4.3-18.8) | ||
| > 250 | 26.9 (17.1-35.5) | ||
| NT-proBNP | 0-300 | 5.2 (4-6.8) | |
| 301-900 | 16.1 (12-20.2) | ||
| 901-3000 | 26 (18.3-33.7) | ||
| > 3000 | 39.5 (26.3-52.6) |
Postoperative Natriuretic Peptide Thresholds for Predicting 30-day Mortality and Non-fatal Myocardial Infarction
- Patients with a postoperative BNP ≥ 245 pg.ml or NT-proBNP ≥ 718 pg.ml had significantly elevated risk for 30-day mortality or non-fatal MI, mortality and cardiac failure
| Type of Surgery | Type of NP | NP Level (pg/ml) | MACE (%) |
|---|---|---|---|
| Mixed Non-cardiac Surgery | BNP | 0-250 | 6.6 (4.7-9.2) |
| 251-400 | 15.7 (6.4-26.1) | ||
| > 400 | 29.5 (20.7-37.8) | ||
| NT-proBNP | 0-300 | 1.8 (0.8-2.9) | |
| 301-900 | 8.7 (5.8-11.7) | ||
| 901-3000 | 20.9 (16.3-22.5) | ||
| > 3000 | 38.4 (30.7-46) |
Trop T
Introduction
- Pre-operative troponin elevation may be useful to risk stratify vascular surgery patients pre-operatively, demonstrating prospective validation.
- A prospective observational study of patients with a history of coronary artery disease or at risk of coronary artery disease undergoing major non-cardiac surgery has shown that a pre-operative high-sensitivity troponin T above the upper reference limit (>14 ng/L) is independently associated with early postoperative and 3-year mortality.
- In all non-cardiac surgical patients with known cardiovascular risk or undergoing major surgery, we recommend postoperative troponin monitoring.
Postoperative Troponin Monitoring
- An analysis of the first 15,133 patients in the study found that patients with a peak postoperative troponin T elevation ≤10 ng/L had a mortality rate of 1%. In contrast, patients with a peak troponin T value of 20 ng/L, 30–290 ng/L, and ≥300 ng/L had mortality rates of 4%, 9.3%, and 16.9%, respectively.
- In summary, postoperative troponin elevation, with or without myocardial infarction-defining features, is associated with a significant increase in mortality risk.
Interpretation of Postoperative Troponin Thresholds for Predicting 30-day Mortality After Non-Cardiac Surgery
| Troponin T (ng/L) | 30-day Mortality | Likelihood Ratio |
|---|---|---|
| ≤10 | 1% (Low) | 0.53 (Low) |
| 20 | 4% (Moderate) | 2.22 (Moderate) |
| 30–290 | 9.3% (High) | 5.39 (High) |
| ≥300 | 16.9% (Very High) | 10.71 (Very High) |
- The cardiac troponins (cTn) T and I are the most commonly used biomarkers of myocardial damage. They become elevated around 3–6 hours, peak at around 12–24 hours, and can remain elevated for up to 2 weeks, depending on renal function.
- Abnormal levels of cTn are defined as those above the 99th percentile of the normal population or upper reference limit for that laboratory assay, and most local cardiology services will issue a ‘positive’ result range.
- Elevated levels of cTn must be interpreted in the clinical context. Serial cTn levels may aid diagnosis (e.g., a rapid increase within 24 hours, peak levels >50× upper reference limit, and rapid decrease of >50% within 72 hours are indicative of acute myocardial infarction).
- In ACS, higher troponin levels (peak values and area under the cTn–time curve) correlate with infarct size and consequent risk of mortality and morbidity. In the postoperative population, an elevated troponin, peaking in the first 3 days after operation, is strongly associated with increased 30-day mortality.
Causes for Raise Trop T Levels
Demand Ischemia (In the Absence of ACS)
- Supraventricular tachycardia/atrial fibrillation
- Left ventricular hypertrophy
- Anemia
- Hypotension
- Hypovolemia
Direct Myocardial Damage
- Cardiac contusion
- Direct current cardioversion
- Cardiac infiltrative disorders
- Chemotherapy
- Myocarditis
- Cardiac transplantation(immune-mediated reactions)
Myocardial Strain
- Congestive heart failure
- Pulmonary embolism
- Pulmonary hypertension or COPD
Chronic Renal Insufficiency
Sepsis/Systemic Inflammatory Processes
Intracranial Pathology
- Intracerebral hemorrhage or stroke
Links
References:
- Reed-Poysden, C. and Gupta, K. (2015). Acute coronary syndromes. BJA Education, 15(6), 286-293. https://doi.org/10.1093/bjaceaccp/mkv010
- Rodseth RN, Biccard BM, Le Manach Y, Sessler DI et al. The prognostic value of pre-operative and post-operative B-type natriuretic peptides in patients undergoing noncardiac surgery: B-type natriuretic peptide and N-terminal fragment of pro-B-type natriuretic peptide: a systematic review and individual patient data meta-analysis. J Am Coll Cardiol. 2014 Jan 21;63(2):170-80. doi: 10.1016/j.jacc.2013.08.1630. Epub 2013 Sep 26. PMID: 24076282.
Summaries:
Antiplatelet and stents
Copyright**
© 2025 Francois Uys. All Rights Reserved.
id: “691180d1-66ec-4efa-817b-7a0ef0b8bfc3”



