- Arterial Cannulation
- Indications
- Contraindications
- Site Selection
- Technique
- Maintenance & Infection Prevention
- Complications and Mitigation
- Arterial Pressure Waveform Interpretation
- Special Situations
- Normal ABG on Room Air
- Steps to Interpret Acid-Base Disturbances
- Metabolic Acidosis Considerations
- Respiratory Acidosis Considerations
- Respiratory Alkalosis
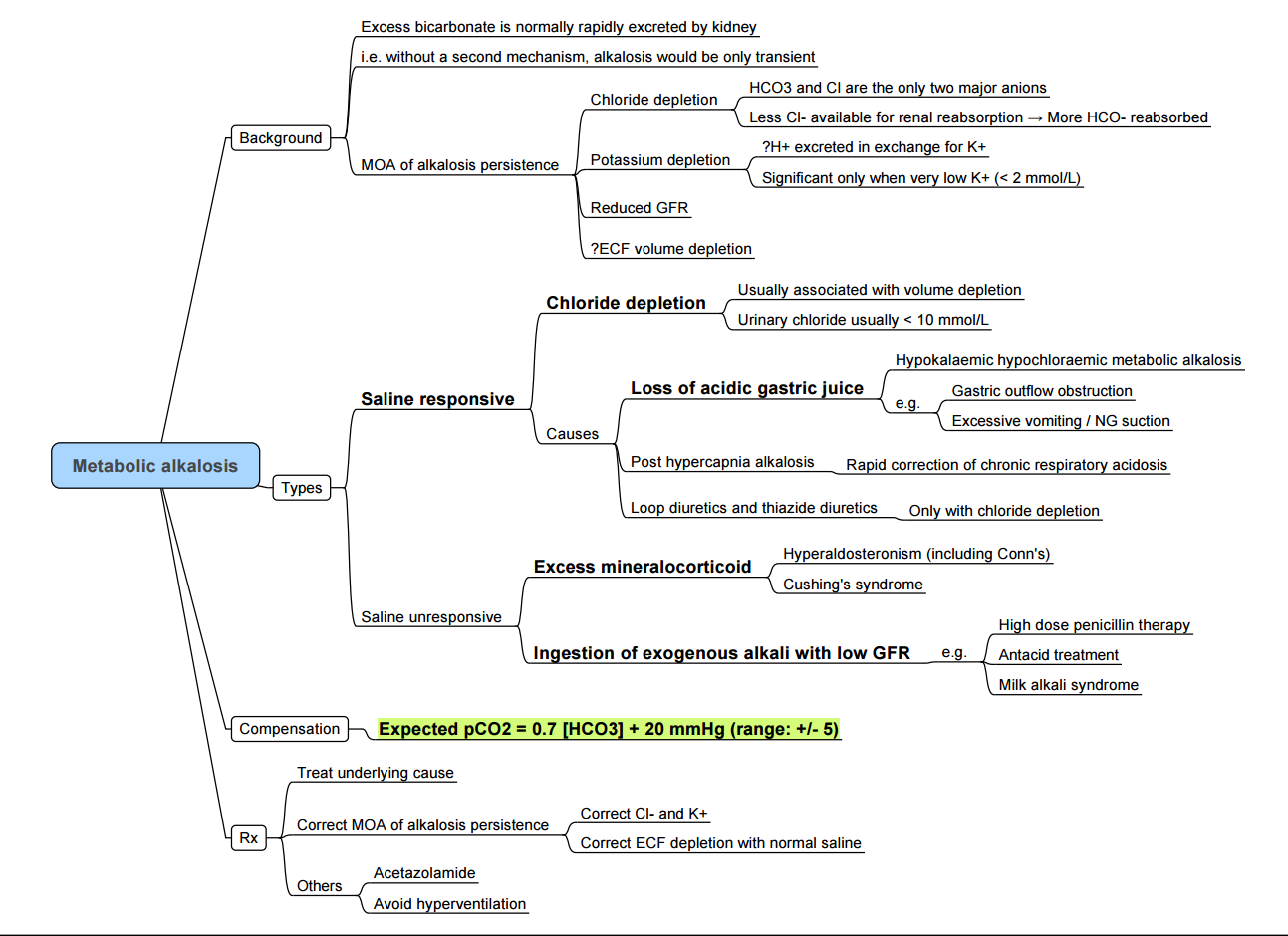
- Metabolic Alkalosis
- Links
{}
Arterial Cannulation
Indications
- Beat-to-beat arterial blood pressure and mean arterial pressure (MAP) monitoring during major surgery, haemodynamic instability, extracorporeal circuits (e.g. ECMO, IABP) and thrombolysis or hypertensive emergencies.
- Frequent arterial blood gas (ABG) analysis or lactate trending.
- Continuous sampling for laboratory investigation when venous access is unreliable.
- Advanced haemodynamic calculations (pulse-contour cardiac output, stroke-volume or pulse-pressure variation).
- Neuro-anaesthesia, trauma or stroke cases in which tight cerebral perfusion pressure control is required.
- Major burns, obstetric crises (e.g. massive haemorrhage) and paediatric cardiac surgery where invasive pressures guide resuscitation.
Contraindications
Absolute
- Absent distal pulse or proven inadequate collateral circulation (Doppler, plethysmography).
- Local infection, burn or traumatic disruption at the proposed site.
- Prior radial artery harvest/prosthetic graft in the limb.
- Critical limb ischaemia or unreconstructable peripheral vascular disease.
Relative
- Coagulopathy (platelets < 50 × 10⁹ L⁻¹ or INR > 2) or therapeutic anticoagulation.
- Raynaud phenomenon, Buerger disease, severe vasospasm.
- ipsilateral arteriovenous fistula/lymphoedema/axillary node dissection.
- High-dose vasopressor infusion (risk of digital ischaemia).
- Sugical field proximity or planned limb positioning incompatible with line security.
Site Selection
| Site | Advantages | Disadvantages | Comment |
|---|---|---|---|
| Radial | Superficial, low infection rate, palmar collateral flow | Small calibre in shock/children | Preferred; ultrasound first-pass success >90 % |
| Ulnar | Preservation of radial grafts | Deeper, smaller, proximity to ulnar nerve | Reserve for failed radial |
| Brachial | Large calibre, easy ultrasound view | End artery, median nerve injury risk | Acceptable for ≤48 h with ≤20 G catheter |
| Axillary | Central pressure, mobile limb | Plexus proximity, technical | Useful when femoral contraindicated |
| Femoral | Rapid access in shock/CPR, reliable waveform | Higher bleed/infection if asepsis poor | Ideal in major vasoconstriction or CPB gradients |
| Dorsalis pedis / Posterior tibial | Accessible prone/upper-limb burns | Amplified systolic BP, distal ischaemia | Continuous foot perfusion checks |
Technique
- Ultrasound guidance (short-axis out-of-plane or long-axis in-plane) is recommended; meta-analysis shows higher first-pass success, fewer attempts and haematomata than palpation.
- Direct over-the-needle, Seldinger or modified Seldinger techniques are acceptable; choose smallest catheter that provides reliable waveform (20–22 G adults, 22–24 G paediatrics).
- Zero transducer at the phlebostatic axis (4th intercostal, mid-axillary); re-zero after patient repositioning >15 °.
- Fast-flush test daily to confirm adequate natural frequency (>10 Hz) and optimal damping (1–2 oscillations).
Maintenance & Infection Prevention
- Pressurised (300 mmHg) 0.9 % saline at 2–3 mL h⁻¹; routine heparinised flush offers no patency benefit and risks thrombocytopenia—avoid unless repeated clotting occurs.
- Chlorhexidine–alcohol skin preparation, maximal sterile-barrier precautions, sterile ultrasound cover and dedicated transducer.
- Transparent dressing with date/time; inspect insertion site at least once per shift.
- Daily line-necessity check—catheter-related bloodstream infection risk rises steeply after day 4–5; remove or resite where feasible.
Complications and Mitigation
| Category | Incidence | Prevention/Management |
|---|---|---|
| Mechanical failure / haematoma | 6–28 % | Ultrasound, <3 attempts, compression 5 min |
| Thrombosis / digital ischaemia | 0.1–0.5 % | Small catheter, limb perfusion checks, remove if blanching |
| Catheter-related infection | 0.15 per 1000 catheter-days | Strict asepsis, minimise dwell time |
| Haemorrhage / line disconnection | <1 % | Locking connectors, alarms, securement device |
| Nerve injury (median, radial) | Rare | Use ultrasound to visualise nerve, avoid multiple passes |
Arterial Pressure Waveform Interpretation
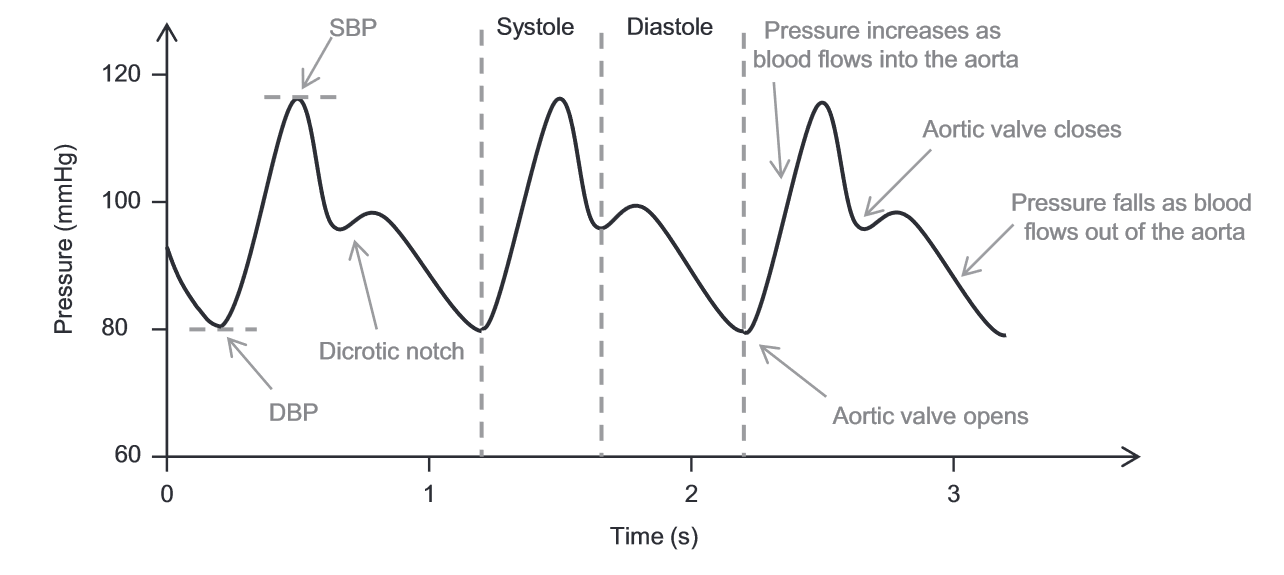
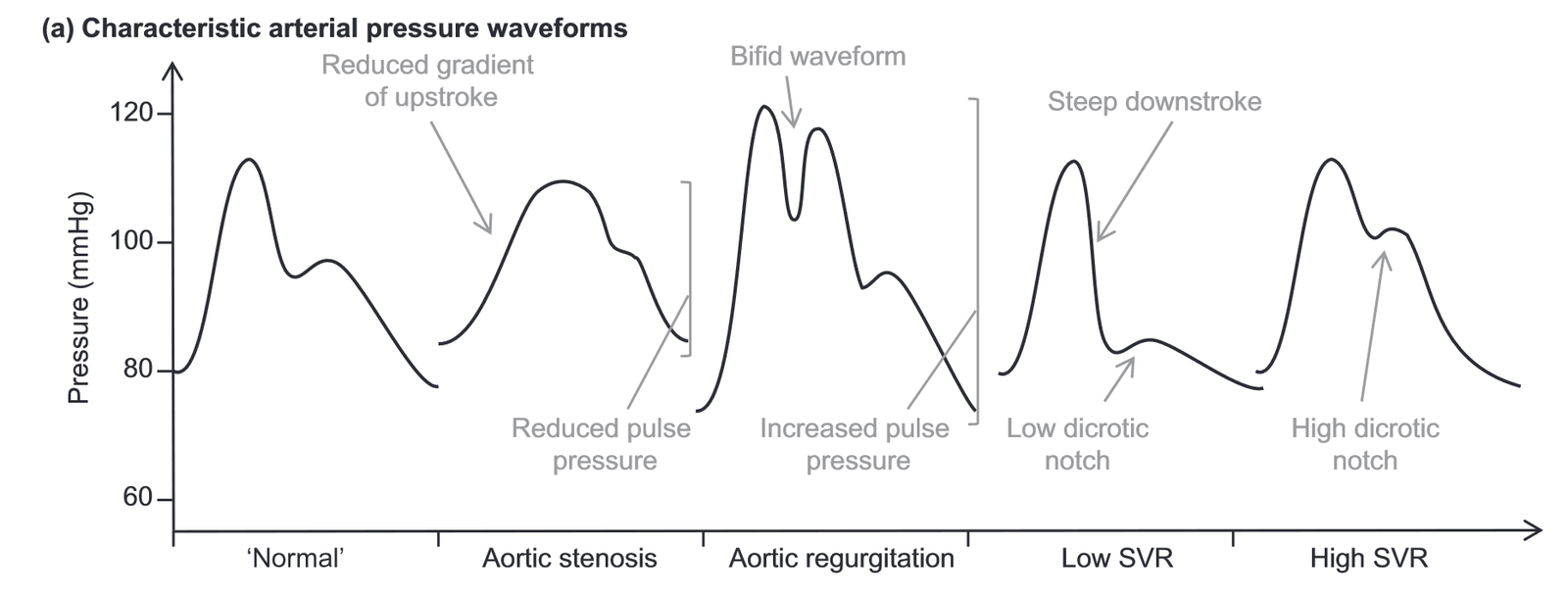
- Components: rapid systolic upstroke → peak systolic → dicrotic notch (aortic valve closure) → diastolic runoff → end-diastolic pressure.
- Peripheral amplification: from aorta to radial the systolic rises (~5–20 mm Hg), diastolic falls; MAP remains constant.
- Dynamic response errors:
- Underdamped–tall, narrow peaks, overshoot SBP, wide pulse pressure.
- Overdamped–blunted upstroke, loss of dicrotic notch, underestimated SBP.
- Troubleshooting: remove air/clots, shorten tubing (<120 cm), ensure 300 mm Hg flush pressure, replace kinked catheter/tubing.
Special Situations
- Paediatrics/neonates: ultrasound guidance markedly improves success; 24 G radial or posterior tibial preferred.
- Cardiac bypass/vasopressor use: dual radial + femoral lines detect radial–central gradient.
- Prone ventilation/major burns: secure limb padding, consider dorsalis pedis.
- South African context: higher prevalence of HIV, diabetes and peripheral vascular disease—ultrasound enhances safety, and resource-adjusted protocols should balance cost with reduction in complications and cannulation time.
Normal ABG on Room Air
- pH: 7.40
- pCO2: 40 mmHg
- HCO3: 24 mEq/L
- Normal O2: > 80 mmHg
- Normal Anion Gap (AG): 12 ± 2
Steps to Interpret Acid-Base Disturbances
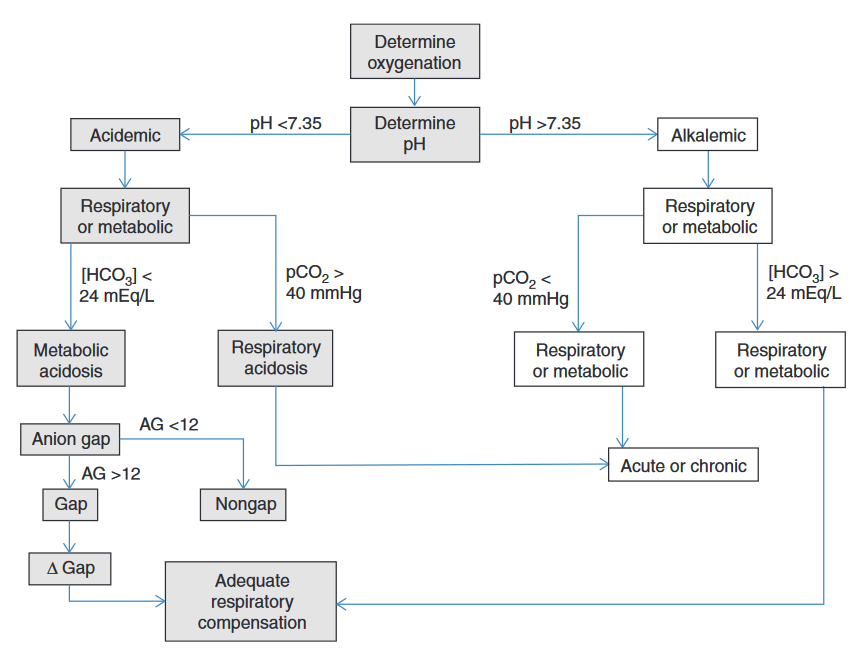
1. Adequate Oxygenation?
- Normal O2: > 80 mmHg
- Possible Hypoxemia: Consider if pO2 is less than expected.
2. Define the Acid-Base Disturbance
- pH < 7.35: Acidemia
- Metabolic Acidosis: Gain of acid or loss of HCO3⁻
- Respiratory Acidosis: Hypoventilation, increased pCO2
- pH > 7.45: Alkalemia
- Metabolic Alkalosis: Gain of HCO3⁻ or loss of acid
- Respiratory Alkalosis: Hyperventilation, decreased pCO2
3. Identify the Primary Process
-
Metabolic Acidosis:
- Acute: HCO3⁻ < 24 mEq/L with corresponding pCO2 compensation
- Chronic: Same pattern but over longer duration
-
Respiratory Acidosis:
- Acute: Elevated pCO2 with minimal change in HCO3⁻
- Chronic: Elevated pCO2 with compensatory increase in HCO3⁻
-
Metabolic Alkalosis:
- Acute: HCO3⁻ > 24 mEq/L with compensatory increase in pCO2
- Chronic: Same pattern but over longer duration
-
Respiratory Alkalosis:
- Acute: Decreased pCO2 with minimal change in HCO3⁻
- Chronic: Decreased pCO2 with compensatory decrease in HCO3⁻
4. Compensatory Mechanisms
A. Metabolic Disorders
- Metabolic Acidosis (Winter’s formula)
- pCO2 expected=(1.5×[HCO3−])+8 ± 2(mmHg)
- Metabolic Alkalosis
- pCO2 expected=(0.7×[HCO3−])+20(mmHg)
B. Respiratory Disorders
ΔPCO₂ = (measured PCO₂ – 40 mmHg).
- Respiratory Acidosis
- Acute:
Δ[HCO3−]=0.1×ΔpCO2⟹
(HCO3−)exp=24+0.1×(pCO2−40) - Chronic:
Δ[HCO3−]=0.35×ΔpCO2⟹
(HCO3−)exp=24+0.35×(pCO2−40)
- Acute:
- Respiratory Alkalosis
- Acute
Δ[HCO3−]=0.2×(40−pCO2)⟹
(HCO3−)exp=24−0.2×(40−pCO2) - Chronic:
Δ[HCO3−]=0.35×(40−pCO2)⟹
(HCO3−)exp=24−0.35×(40−pCO2)
- Acute
5. Calculate Anion Gap (AG)
- AG: Na⁺ – (Cl⁻ + HCO3⁻)
- Normal AG: 12 ± 2
- High AG: Presence of unmeasured anions
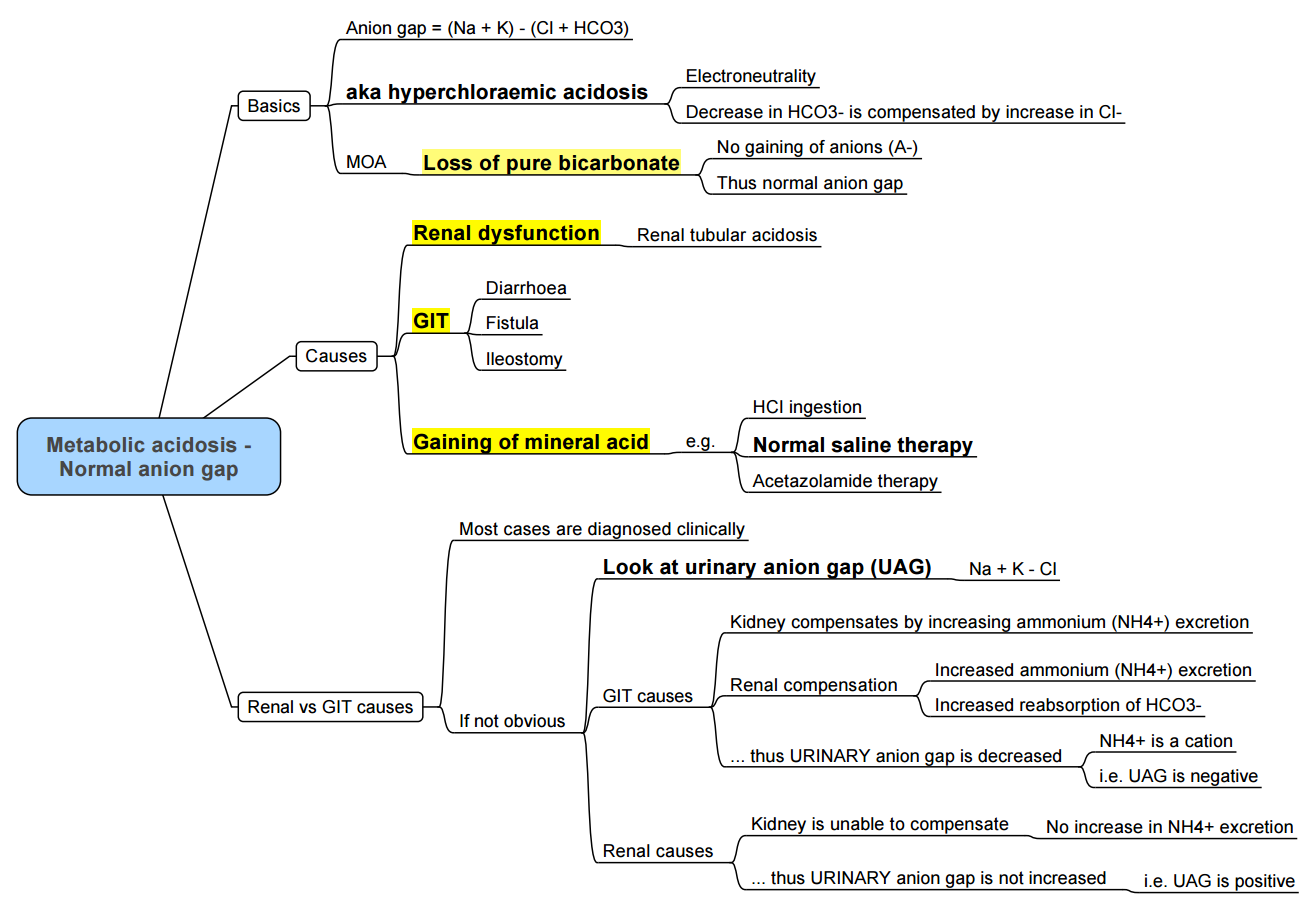
6. Normal AG Metabolic Acidosis (NAGMA)
- Causes:
- GI Losses of HCO3⁻ (Diarrhea)
- Renal Tubular Acidosis (RTA)
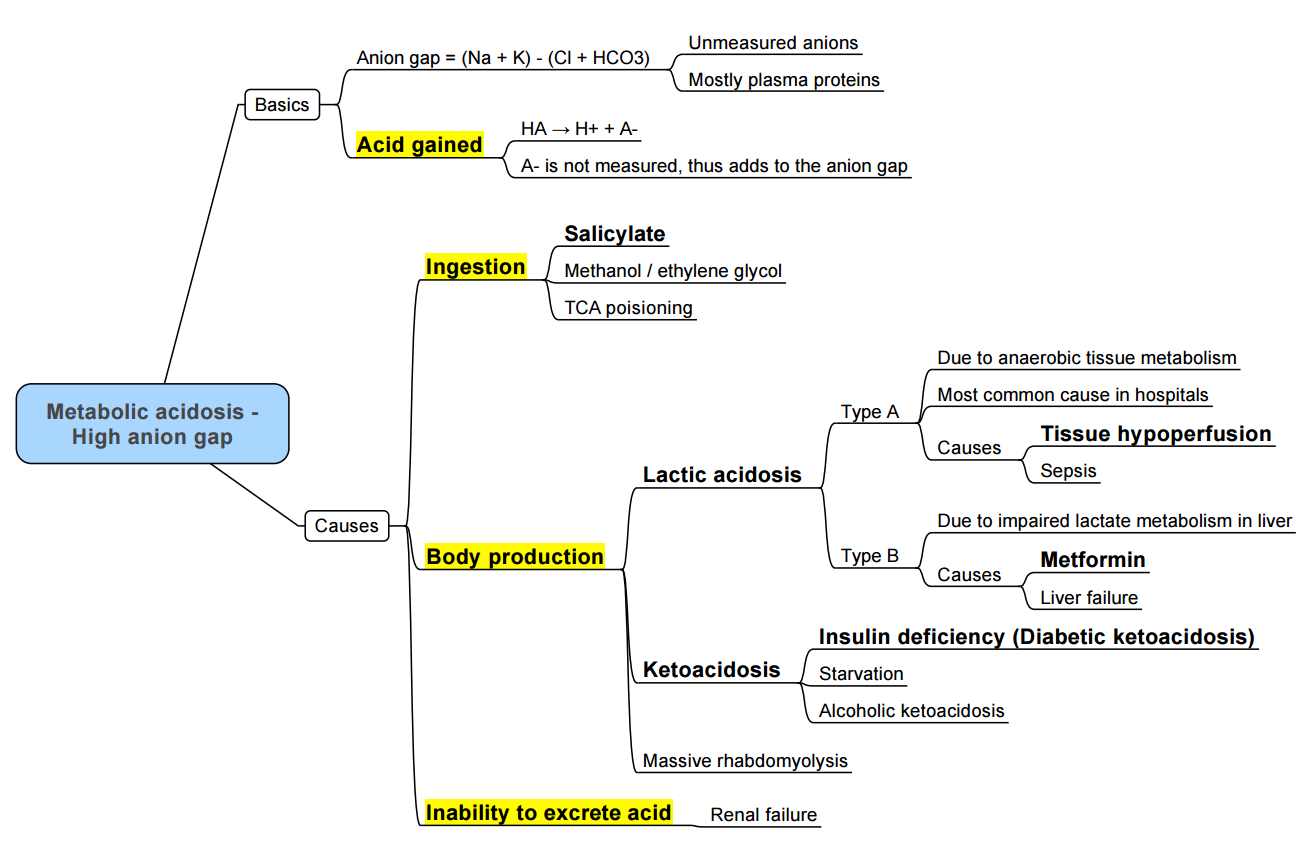
7. High AG Metabolic Acidosis (HAGMA)
- Causes: Accumulation of acids like lactate or ketones, renal failure, toxins.
8. Compensation and Mixed Disorders
- Winter’s Formula for Metabolic Acidosis: Expected pCO2 = 1.5 × (HCO3⁻) + 8 ± 2
- Delta-Delta (Δ/Δ) Ratio: Used to identify mixed disorders
Metabolic Acidosis Considerations
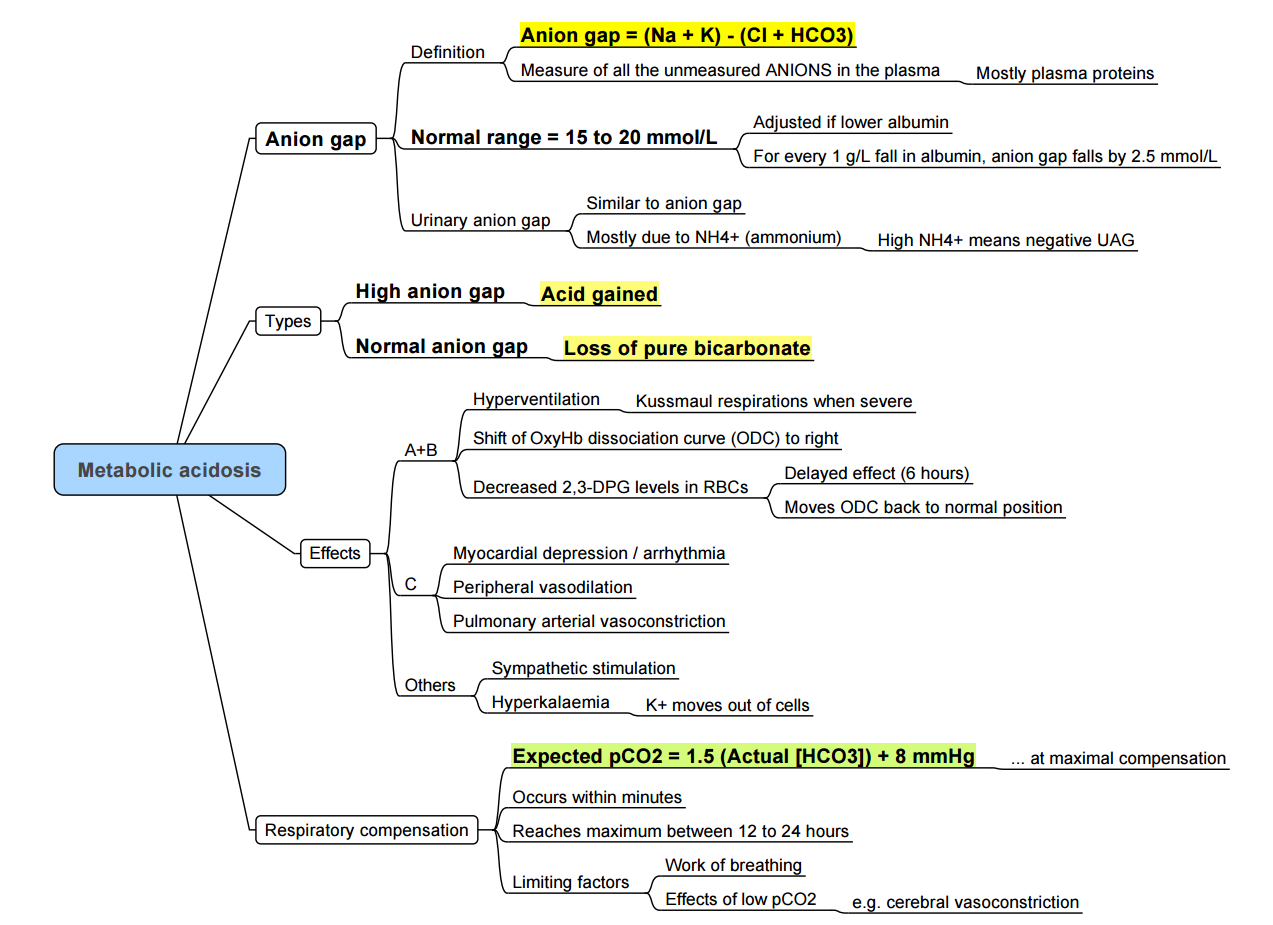
Winter’s Formula
PCO2=(1.5×HCO3)+8
- Interpretation:
- If measured PCO2 > calculated PCO2: Concurrent respiratory acidosis is present.
- If measured PCO2 < calculated PCO2: Concurrent respiratory alkalosis is present.
Delta Gap (Δ gap)
Δgap=AG−12+HCO3
- Interpretation:
- If Δ gap < 22 mEq/L: Concurrent non-gap metabolic acidosis exists.
- If Δ gap > 26 mEq/L: Concurrent metabolic alkalosis exists.
MUDPILES (High Anion Gap Metabolic Acidosis – HIGMA)
- M: Methanol
- U: Uremia
- D: Diabetic ketoacidosis
- P: Paraldehyde
- I: Infection, In therapy
- L: Lactic acidosis
- E: Ethanol, ethylene glycol
- S: Salicylates (aspirin)
Causes of Normal Anion Gap Metabolic Acidosis (NAGMA)
- Excessive administration of 0.9% normal saline
- Gastrointestinal losses: Diarrhea, ileostomy, neobladder, pancreatic fistula
- Renal losses: Renal tubular acidosis
- Drugs: Acetazolamide
Lactic Acidosis
Definition and Types
- Lactic Acidosis: Elevated blood lactate levels > 2 mmol/L
- Type A: Impaired oxygen delivery (e.g., shock, hypoxia)
- Type B: Impaired oxygen utilization (e.g., mitochondrial dysfunction)
- Type D: Bacterial overgrowth
Pathophysiology
- Anaerobic Glycolysis: Pyruvate converted to lactate when oxygen is scarce
- Lactate Clearance: Liver and kidneys play major roles
Causes of Increased Lactate Production
- Hypoxia: Decreased oxygen delivery (e.g., cardiac arrest, sepsis)
- Increased Oxygen Demand: Exercise, seizures
- Impaired Clearance: Liver disease, renal failure
Treatment Approaches
- Address Underlying Cause: Oxygen delivery, removal of toxins
- Supportive Measures: IV fluids, bicarbonate in severe cases
Respiratory Acidosis Considerations
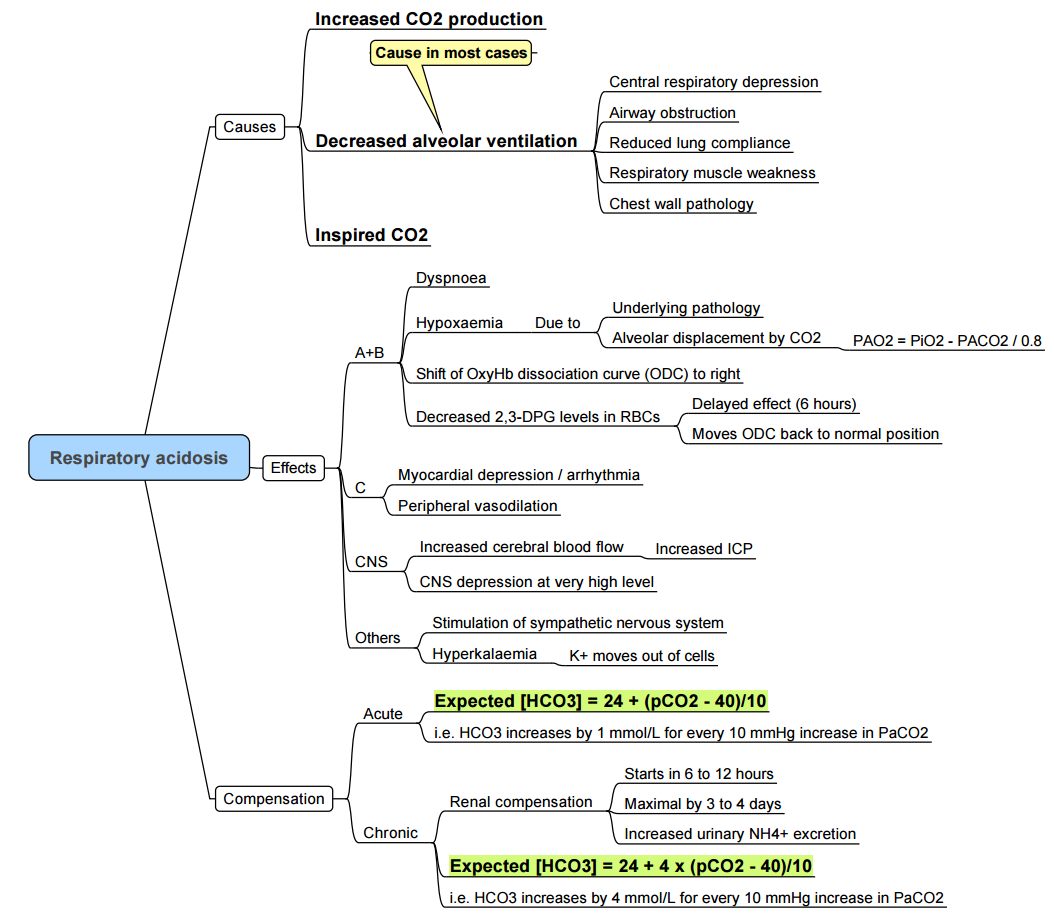
Increased CO2 Production
- Malignant hyperthermia
- Hyperthyroidism
- Sepsis
- Overfeeding
Decreased CO2 Elimination
- Intrinsic pulmonary disease: Pneumonia, ARDS, fibrosis, edema
- Upper airway obstruction: Laryngospasm, foreign body, OSA
- Lower airway obstruction: Asthma, COPD
- Chest wall restriction: Obesity, scoliosis, burns
- CNS depression: Anesthetics, opioids, CNS lesions
- Decreased skeletal muscle strength: Myopathy, neuropathy, residual effects of neuromuscular blocking drugs
- Rarely, an exhausted soda–lime or incompetent one-way valve in an anesthesia delivery system can contribute to respiratory acidosis.
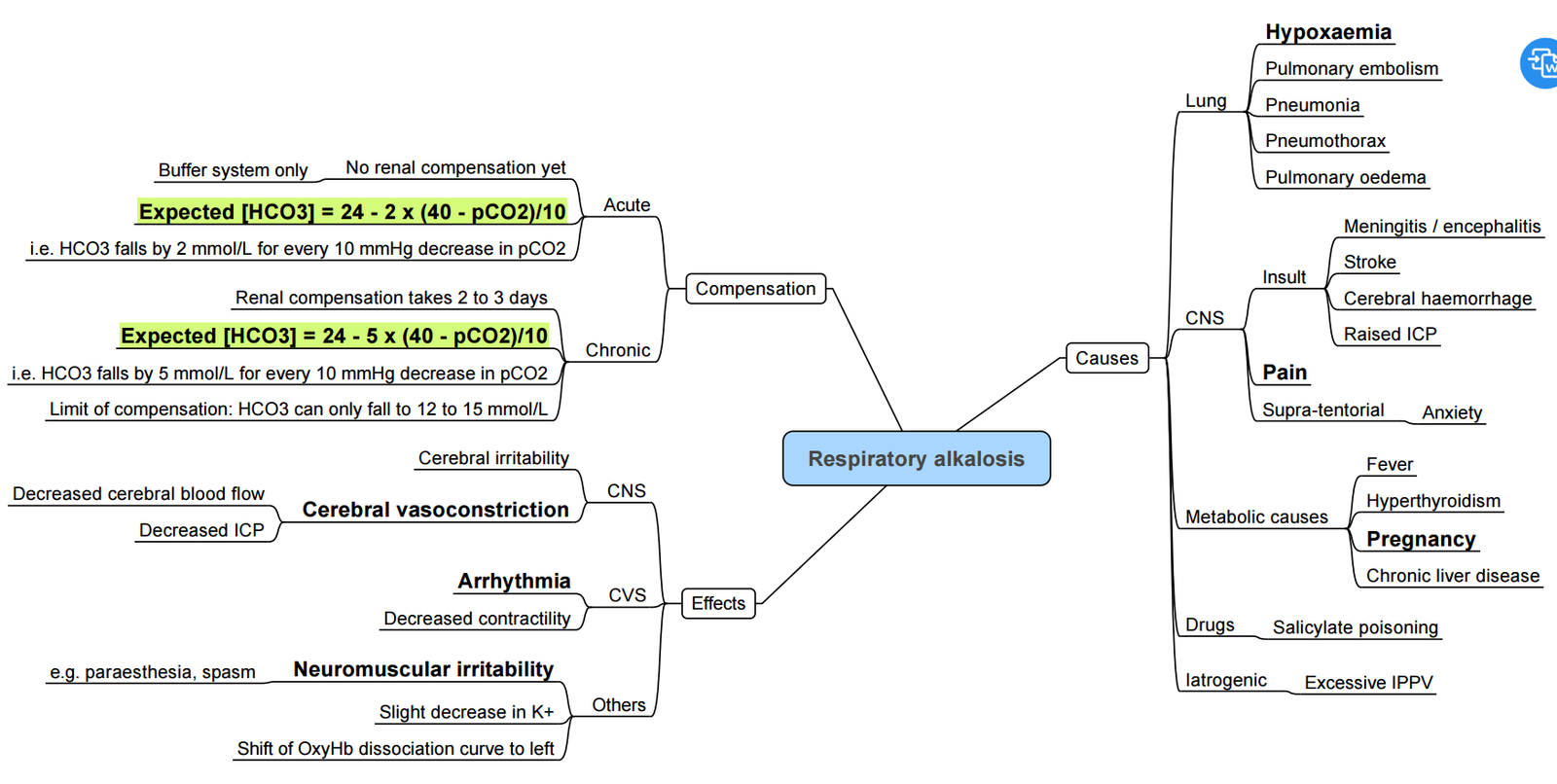
Respiratory Alkalosis
Metabolic Alkalosis
Links
References:
- ICU One Pager. (2024). Retrieved June 5, 2024, from https://onepagericu.com/
- Hager HH, Burns B. Artery Cannulation. [Updated 2023 Jul 24]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482242/
- Pierre L, Pasrija D, Keenaghan M. Arterial Lines. [Updated 2024 Jan 19]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499989/
- Raj, T. D. (2017). Data interpretation in anesthesia.. https://doi.org/10.1007/978-3-319-55862-2
- Chambers D, Huang CLH, Matthews G. Basic physiology for anaesthetists. Cambridge, United Kingdom: Cambridge University Press; 2015.
- Castro D, Patil SM, Zubair M, et al. Arterial Blood Gas. [Updated 2024 Jan 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK536919/
- Soni KD. Ultrasound-guided arterial cannulation: what are we missing and where are we headed? Indian J Crit Care Med 2024;28:632-633. Available from: https://pmc.ncbi.nlm.nih.gov/articles/PMC11234131/ pmc.ncbi.nlm.nih.gov
- Card S, Piersa A, Kaplon A, et al. Infectious risk of arterial lines: a narrative review. J Cardiothorac Vasc Anesth 2023;37:2050-2056. Available from: https://pubmed.ncbi.nlm.nih.gov/37500369/ pubmed.ncbi.nlm.nih.gov
- Nethathe GD, Mbeki M. Heparin flush vs saline flush for maintenance of adult intra-arterial catheters: potential harm, too little gain? SAJAA 2016;22:70-71. Available from: https://www.sajaa.co.za/index.php/sajaa/article/view/1861 sajaa.co.za
- Rezaie S. Damping and arterial lines. REBEL EM blog. 4 Jul 2022. Available from: https://rebelem.com/damping-and-arterial-lines/ rebelem.com
- Williams C, Pasrija D, Pierre L, Keenaghan M. Arterial lines. StatPearls [Internet]. Updated 23 Mar 2025. Available from: https://www.ncbi.nlm.nih.gov/books/NBK499989/
- The Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries:
ICU OP- ABG
ICU One pager Acid base
ICU One pager Lactic acidosis)
Acid/base
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “6918f516-b271-44d2-b561-0945cb2c03d1”



