{}
Central Venous Pressure (CVP)
- Normal range (supine, spontaneous ventilation): 2–6 mm Hg (≈3–8 cm H₂O). Mechanically ventilated or positive end-expiratory pressure (PEEP) ≥10 cm H₂O can raise baseline values by ~3 cm H₂O. CVP ≃ right-atrial pressure (RAP).
Physiology & Determinants
| Variable | Effect on CVP |
|---|---|
| Venous return (VR) = (MSFP–RAP)/Rv | ↑ MSFP (fluid, venous tone) or ↓ Rv → ↑ CVP |
| Rightand left-ventricular compliance & function | RV failure, tamponade, pulmonary hypertension → ↑ CVP |
| Intrathoracic & pleural pressures | PEEP, Valsalva, pneumothorax ↑ CVP; spontaneous inspiration ↓ CVP |
| Intra-abdominal pressure | Abdominal compartment syndrome ↑ CVP without ↑ preload |
- ΔCVP = ΔV / Cᵥ, where Cᵥ = venous compliance.
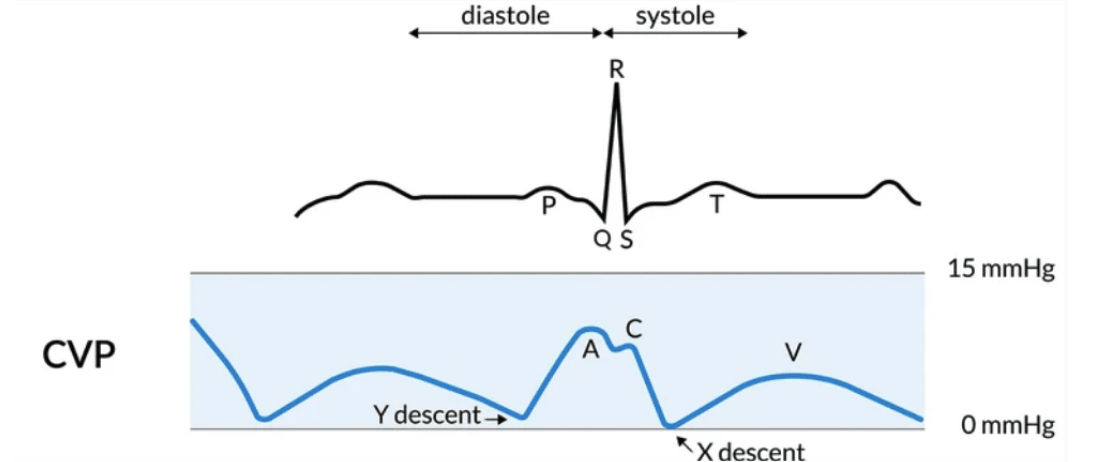
Waveform
- a wave–atrial contraction
- c wave–bulging tricuspid valve in early systole
- x desent–atrial relaxation/downward RV contraction
- v wave–passive atrial filling with closed tricuspid valve
- y descent–rapid ventricular filling after valve opens
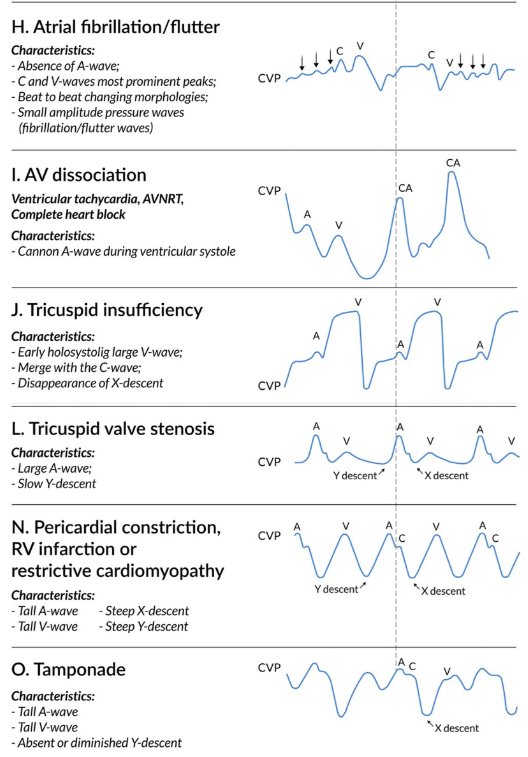
Abnormal Patterns
| Finding | Typical aetiology |
|---|---|
| Dominant a | Pulmonary HTN, tricuspid stenosis |
| Cannon a | Complete heart block, VT with AV dissociation |
| Dominant v | Tricuspid regurgitation |
| Absent x | Atrial fibrillation |
| Deep x | Tamponade, constrictive pericarditis |
| Steep y | Severe TR, constrictive pericarditis |
| Slow y | Tricuspid stenosis, atrial myxoma |
Measurement Best Practice
- Zero transducer at phlebostatic axis (4th ICS mid-axillary).
- Read end-expiration (mean of several cycles).
- Flush test: optimal damping coefficient 0.6-0.8.
- Avoid infusions through the measuring lumen.
- Ultrasound confirmation of tip in lower SVC/RA junction reduces arrhythmia & malposition.
- PEEP of 10 cm H₂O → ↑CVP ≈ 3 cm H₂O (compliance-dependent); adjust interpretation accordingly.
Clinical Utility
Diagnostic Waveform Clues
- RV infarction, cor pulmonale, tamponade, tricuspid disease, constrictive pericarditis, complete heart block.
Procedural/monitoring Roles
- Confirm atrial capture during AV pacing.
- Identify P waves in narrow-complex tachyarrhythmias.
- Rapid confirmation of central line placement.
Limits as a Preload Guide
- Static CVP poorly predicts fluid responsiveness; use trends, ∆CVP with fluid challenge, or dynamic indices (PPV, SVV, echo Doppler) for decision-making.
Pulmonary Capillary Wedge Pressure (PCWP)
Definition–Pressure measured with a balloon-tipped pulmonary artery catheter (PAC) wedged in zone 3; reflects left-atrial pressure and approximates LV end-diastolic pressure (LVEDP) when mitral valve is normal. Normal 4–12 mm Hg.
Indications for PAC/PCWP
- Cardiogenic vs non-cardiogenic pulmonary oedema.
- Refractory or undifferentiated shock (especially rightor left-sided).
- Complex heart failure, advanced pulmonary hypertension, peri-transplant evaluation.
- Mixed venous oxygen saturation and thermodilution cardiac output monitoring when less invasive modalities are unreliable.
Technique Tips
- Zone 3 placement (PA diastolic > PCWP) avoids false low readings.
- Measure at end-expiration in supine 30 ° head-up; over-wedging may occlude flow and cause infarct.
- Large v waves during occlusion suggest severe MR or non-compliant LA.
Factors Causing PCWP ≠ LVEDP
| Situation | Effect |
|---|---|
| Mitral stenosis/atrial myxoma | PCWP > LVEDP |
| ↓ LA or LV compliance (ischaemia, hypertrophy) | PCWP > LVEDP |
| Positive-pressure ventilation, PEEP | PCWP overestimates true filling pressure |
| Pulmonary veno-occlusive disease / ↑ PVR | PCWP < LVEDP |
| Intracardiac shunts | Variable error |
Complications of PAC
- Dysrhythmia (PVCs, VT, VF)
- RBBB & potential complete heart block in pre-existing LBBB.
- PA rupture or infarction (balloon inflation distal).
- Infection, thrombosis, catheter knotting
- Risk is reduced by ultrasound-guided insertion, balloon inflation under waveform guidance only, limiting wedging time to ≤15 s, and daily need assessment.
Evidence & Current Position
Robust RCTs show no outcome benefit from routine PAC use in general ICU/surgical patients; selective use in cardiogenic shock, pulmonary hypertension and complex peri-cardiac surgery may improve short-term haemodynamics and, in observational studies, survival. Clinicians should integrate PAC data with echocardiography and less invasive monitors rather than rely on single parameters.
Links
- Arterial line and blood gas (ABG)
- Vascular physiology
- Cardiac physiology
- Pulmonary artery catheter (PAC)
References:
- Chambers D, Huang CLH, Matthews G. Basic physiology for anaesthetists. Cambridge, United Kingdom: Cambridge University Press; 2015.
- Bootsma, I. T., Boerma, E. C., Lange, F. d., & Scheeren, T. (2021). The contemporary pulmonary artery catheter. part 1: placement and waveform analysis. Journal of Clinical Monitoring and Computing, 36(1), 5-15. https://doi.org/10.1007/s10877-021-00662-8
- Nickson, C. (2024, November 8). CVP Measurement. Life in the Fast Lane. Retrieved March 16, 2025, from https://litfl.com/cvp-measurement/
- Raj, T. D. (2017). Data interpretation in anesthesia.. https://doi.org/10.1007/978-3-319-55862-2
- Hensley FA, Gravlee GP, Martin DE. Practical Approach to Cardiac Anesthesia. 5th Ed. Philadelphia Wolters Kluwer. Ann Arbor, Michigan. Proquest; 2014: 118-37.
- Nickson C. CVP Measurement. LITFL 2024. Available from: https://litfl.com/cvp-measurement/ litfl.com
- StatPearls Publishing. Physiology, Central Venous Pressure. Updated 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK519493/ ncbi.nlm.nih.gov
- Oostendorp N et al. Haemodynamic monitoring during non-cardiac surgery: past, present and future. J Clin Monit Comput 2024;38:123-134. link.springer.com
- Bishop DG, Dyer RA, Crowther M. Balancing haemodynamic priorities in obstetrics. SAJAA 2024;30:72-75. Available from: http://www.sajaa.co.za sajaa.co.za
- Van Zyl-Smith M. Haemodynamic monitoring in high-risk surgery. SAJAA 2020;26:68-74. sajaa.co.za
- Nair R, Lamaa N. Pulmonary Capillary Wedge Pressure. StatPearls 2023. Available from: https://www.ncbi.nlm.nih.gov/books/NBK557748/ ncbi.nlm.nih.gov
- Lee J et al. Effectiveness of pulmonary artery catheter monitoring for cardiogenic shock: systematic review & meta-analysis. J Thorac Dis 2023;15:1115-1123. Available from: https://pubmed.ncbi.nlm.nih.gov/37065575/ pubmed.ncbi.nlm.nih.gov
- StatPearls Publishing. Pulmonary Artery Catheterization. Updated 2024. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482170/ ncbi.nlm.nih.gov
- Raisi-Estabragh Z et al. Relationship between PEEP and CVP in ventilated adults. Crit Care Res Pract 2017; Article ID 5941312.
- Connor C, Conley C. Commonly Used Monitoring Techniques. In: Barash PG. et al (ed). Clinical Anesthesia. 8th Ed. Philadelphia; Wolters Kluwer; 2017: 706-30.
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “b2e2e5bf-725c-4be4-a390-d09f759618f6”



