{}
Anaesthesia Considerations for LVADs/VADs
Types
- 1st Generation: Pulsatile (large, clumsy, noisy)
- 2nd Generation: Small, impeller/rotator
Principle
LVADs are semi-permanent hemodynamic support devices for end-stage heart failure.
- Implantation: Surgically placed intrathoracically or intrabdominally.
- Models: Heartmate 2/3 (Abbott), HVAD (Medtronic).
- Use cases:
- Bridge-to-transplant (BTT)
- Destination therapy (DT)–no transplant planned.
- Bridge-to-decision–uncertain transplant candidacy
Indications
- NYHA Class IV (EF <25%)
- Maximal medical therapy
- Chronic inotrope dependence
Physiology
LVAD Components
- Inflow cannula: Removes blood from LV.
- Pump
- Outflow cannula: Returns blood to aorta.
Magnetic Centrifugal-Flow LVADs
- Use magnetically levitated rotors
- Enable high flow with low hemolysis/thrombosis risk.
Hemodynamic Effects
- Operate in parallel with native heart
- Unload LV → ↓LV volume & pressure
- ↓LV preload & afterload → ↓SVR → ↑CO
- Eliminate pulsatility → unreliable pulse oximetry
- Note: Aortic valve may not open every beat.
- NB! LVADs are preload dependent and afterload sensitive
Monitoring
Return to Flow
- Difficult to assess BP.
- Manual BP cuff inflated to 120mmHg, Cuff is slowly deflated with doppler over brachial artery.
- The pressure where doppler detect flow is equivalent to MAP
- I.e Doppler: opening pressure ≈ MAP.
- Manual BP cuff inflated to 120mmHg, Cuff is slowly deflated with doppler over brachial artery.
- Manual BP with cuff: target MAP 70–90 mmHg.
- Arterial line preferred if available.
System Monitor
Displays:
- Pump Flow (L/min): Surrogate for cardiac output (4-6L/min)
- Pump Speed (rpm)–typically 3000–9000 rpm
- Pulse Index (PI)–dimensionless measure of the magnitude of pulsatile flow generated by the native heart, 3–7
- Lower PI: Reduced Native heart functioning
- Higher PI: Increased Native heart functioning
- Pump Power (Watts)–Amount of Power required to maintain pump flow. Typically 4–7 W. To high could lead to thrombosis
Complications
1. Suction Events
- Occurs when preload is inadequate → LV collapse
- May cause pump stopping
- Tx: Stop LVAD, transfuse
2. Stroke
- Ischemic & hemorrhagic stroke = major mortality cause
- Incidence:
- Gen 2/3: 2–4%/year
- Gen 1: ~10–17%
3. Infection
- Driveline infections (20–30% cases)
- Pathogens: Staph spp.
- Mediastinitis & pump pocket infections: severe
4. Pump Thrombosis
- Risk ↓ in newer gen (2nd/3rd) LVADs (~1%)
- Gen 1: ↑ incidence (~13%)
- Tx: LVAD exchange or transplantation
5. Device Failure
- Electrical, controller, battery issues
- Check controller/power source if pump not working
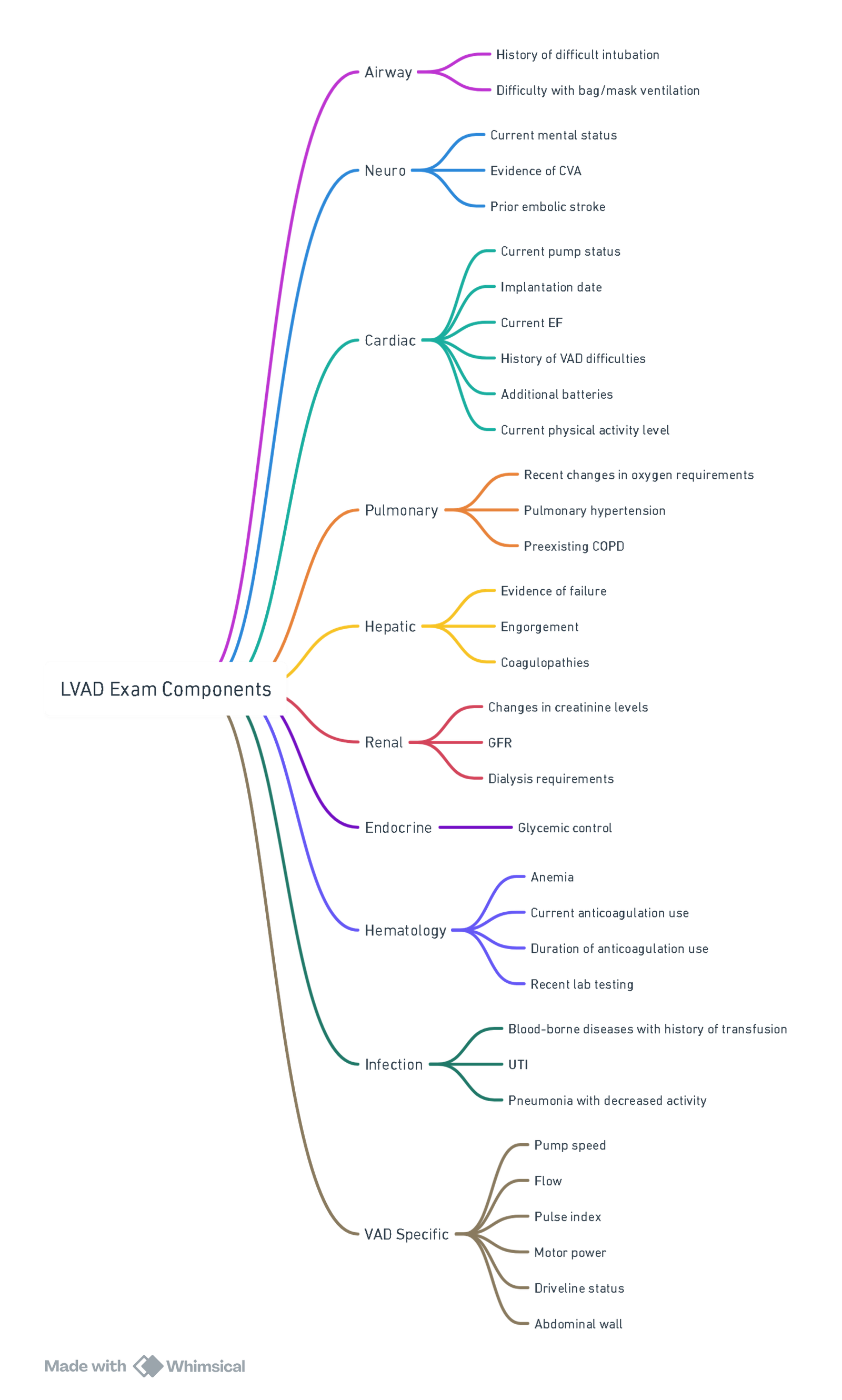
Preoperative Evaluation
The clinical status of an LVAD-supported patient depends on:
- Extent of end-organ damage from low-output states before VAD implantation
- Post-implantation complications
- Present surgical problem
Anaesthetic Considerations and Goals
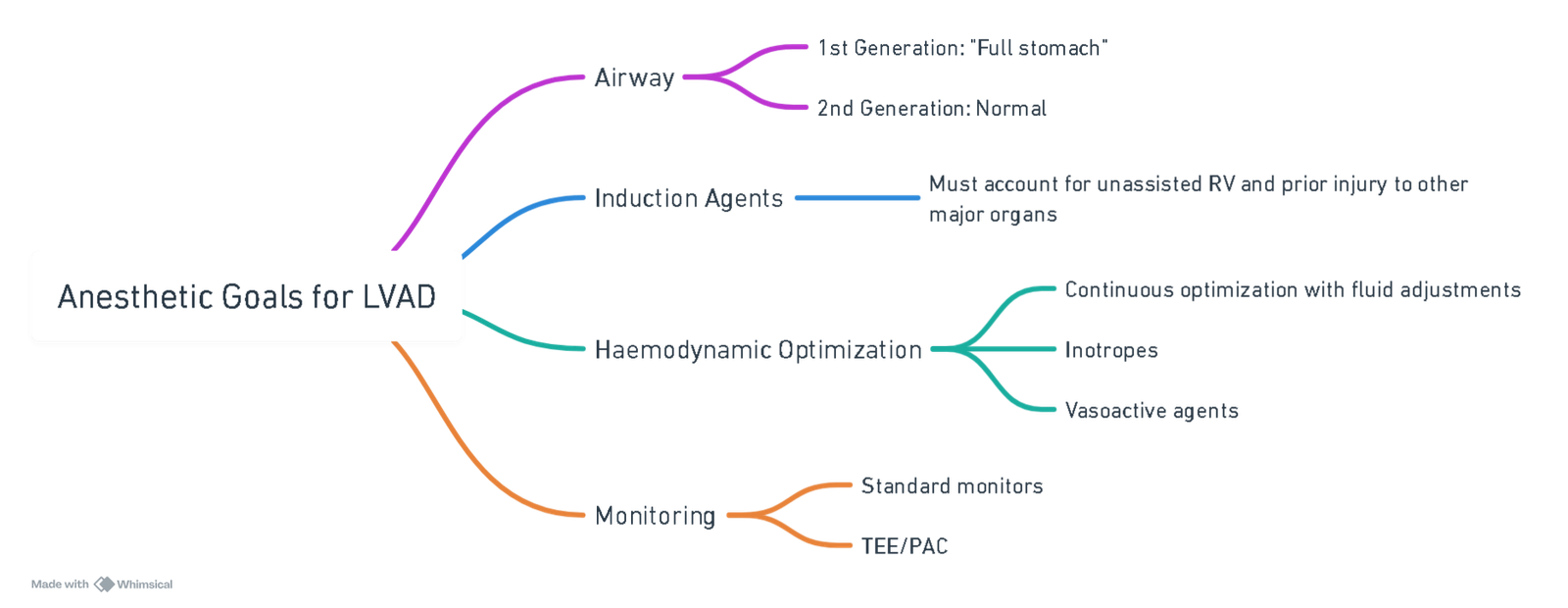
VAD-Specific Considerations
- VADs do not operate on the Starling curve and only pump the volume delivered to them. Factors that decrease preload will affect pump flow and decrease output, such as drugs, dehydration, hemorrhage, lateral decubitus, increased abdominal pressures (insufflation), and bed position.
Cardiac Arrest
- Similar to normal with ACLS principles, except:
- Cardioversion: Do not place pads directly over the device
- Compressions: Evaluate in the moment (dislodgement of cannula may cause certain death). Avoid chest compressions only if LVAD manufacturer advises. Need to ensure that LVAD is not functioning
Postoperative Analgesia
- Avoid hypertension/tachycardia to prevent increased afterload and ensure the patient is not too sedated to prevent pulmonary hypertension and decreased preload.
Notes on Indexes
Pulse Index
- Reflects LV pulsatility
- High = native LV function present
- Low = full LVAD support or low native contractilit
Pump Power
- Reflects pump’s energy demand
- ↑Power = ↑Flow, speed, or thrombosis risk
Key Concepts
- Full preload, reduced pulmonary pressures, not fast, forward (reduce afterload)
- Preload dependent: LVAD function relies on adequate venous return.
- Afterload sensitive: High afterload decreases flow.
- Non-pulsatile flow: May require Doppler or arterial line for MAP.
- Multidisciplinary approach
- Monitor battery, anticoagulation, and other critical factors
Links
References:
- Management of the Patient With Ventricular Assist Device for Non-Cardiac Surgery Michael Manning, M.D., Ph.D. Duke University, Durham, NC. 2017 Anaesthesia Boston
- ICU One Pager. (2024). Retrieved June 5, 2024, from https://onepagericu.com/
Summaries:
LVAD
Copyright**
© 2025 Francois Uys. All Rights Reserved.
id: “ec9361eb-967b-48fe-bf05-ff8493d6e414”



