- Principle of IABP
- Abnormal Waveforms
- Early Balloon Inflation Results in Increased Afterload
- Late Balloon Inflation Results in Decreased Diastolic Augmentation
- Early Balloon Deflation Fails to Decrease Myocardial Oxygen Demand
- Late Balloon Deflation Increases Afterload
- Poor Diastolic Augmentation Results in Suboptimal Coronary Perfusion
- Early Inflation and Late Deflation Increase Afterload; the opposite Fail to Augment
- Links
{}
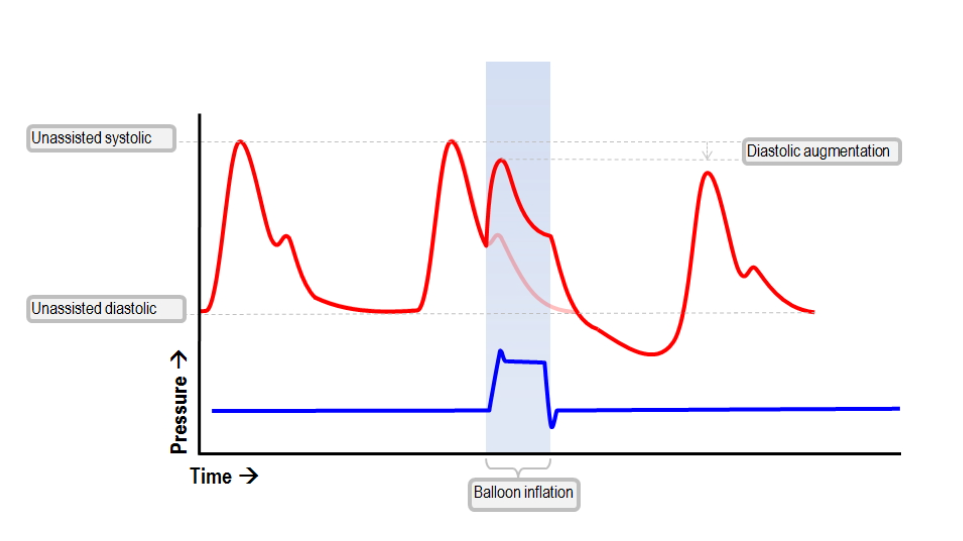
Principle of IABP
- Intra-aortic balloon counter-pulsation is an invasive method of hemodynamic support:
- A catheter with a balloon is placed via an arterial sheath and advanced into the descending thoracic aorta.
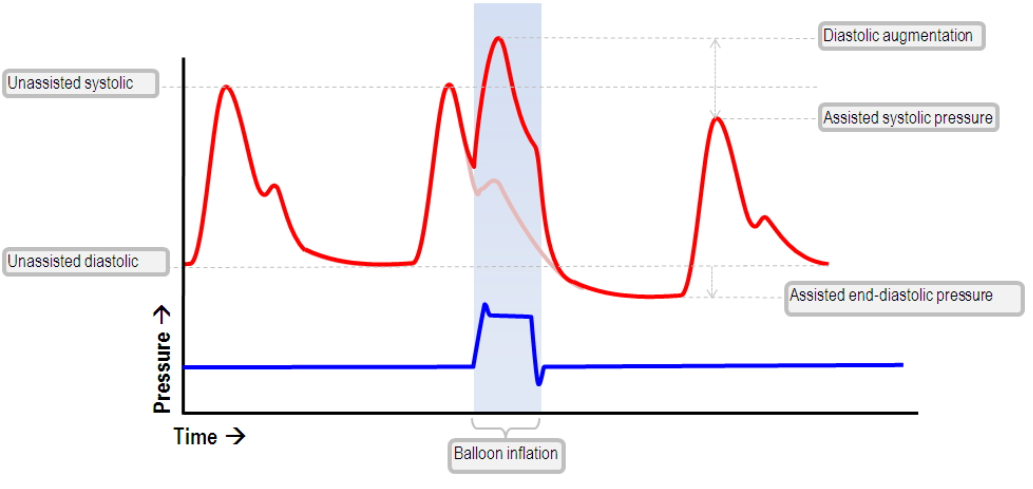
- The balloon inflates in diastole → ↑ coronary perfusion.
- The balloon deflates in systole → ↓ afterload, ↓ LV stroke work, ↑ cardiac output.
- The thick-walled LV benefits from ↓ afterload and ↑ coronary perfusion during diastole.
Concept
-
Diastolic Pressure Time Index (DPTI):
- A measure of coronary perfusion.
- Calculated as: Coronary perfusion x Diastolic time.
-
Systolic Tension Time Index (STTI):
- Represents oxygen demand.
- Calculated as: Systolic pressure x Systolic time.
- Effect of IABP:
- Increases DPTI (improving coronary perfusion).
- Reduces STTI (decreasing myocardial oxygen demand).
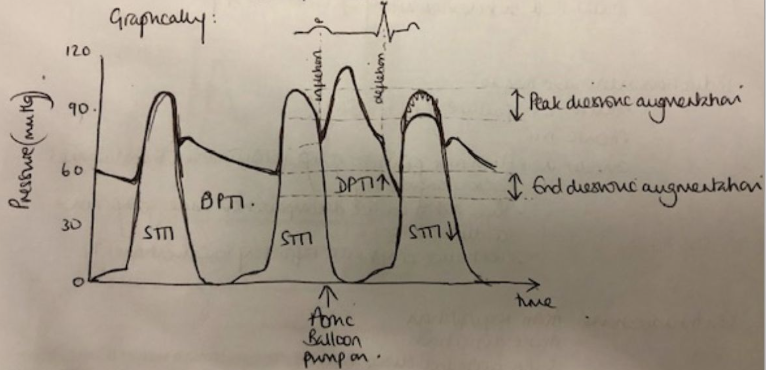
- Top trace = aortic pressure
- Bottom trace = ventricular pressure
Uses
- Cardiogenic shock
- Bridge to intervention/transplant
- Interfacility transfer
- LV vent in patients on VA ECMO
- Meta-analyses show no overall survival benefit, but selected patients (e.g., cardiogenic shock) may benefit.
Placement
- Positioned in descending thoracic aorta, with the tip 2 cm distal to the left subclavian artery.
Haemodynamic Effects
Aorta
- ↓ SBP
- ↑ DBP
Left Ventricle
- ↓ Systolic pressure
- ↓ End-diastolic pressure
- ↓ LV volume and wall tension
Heart
- ↓ Afterload
- ↓ Preload
- ↑ Cardiac output
Coronary Flow
- ↑ or preserved coronary perfusion
Indications
- Acute MI with mechanical/valvular complications
- Cardiogenic shock
- Unstable angina
- High-risk PCI
- Weaning from cardiopulmonary bypass
- Bridge to cardiac transplant
- Adjunct in cardiac surgery
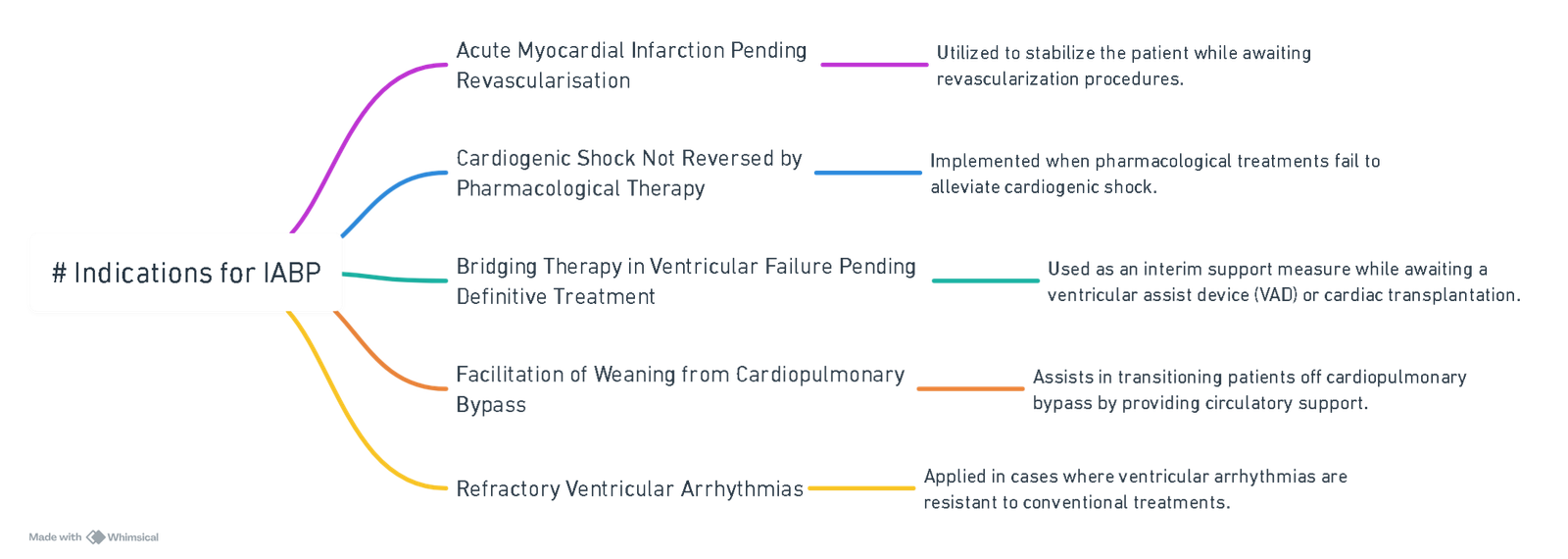
View or edit this diagram in Whimsical.
Contraindications (CI)
Absolute
- Aortic regurgitation
- Aortic dissection
- Aortic stents
- End-stage cardiac disease
- Patient refusal
Relative
- Abdominal aortic aneurysm (AAA)
- Severe peripheral vascular disease (PVD)
- Tachyarrhythmias
- Major arterial reconstruction
Triggering Mechanisms
ECG Triggering
- Preferred method.
- Inflation: Mid-T wave
- Deflation: Peak of R wave
- Susceptible to interference from pacing or arrhythmias.
Pressure Triggering
- Alternative option.
- Based on dicrotic notch (aortic valve closure).
- Less accurate due to slower propagation of pressure waves compared to electrical conduction.
Timing
Optimal Timing:
- Inflation: ~40 ms after dicrotic notch (start of diastole).
- Deflation: Just before systole.
Improper Timing Consequences:
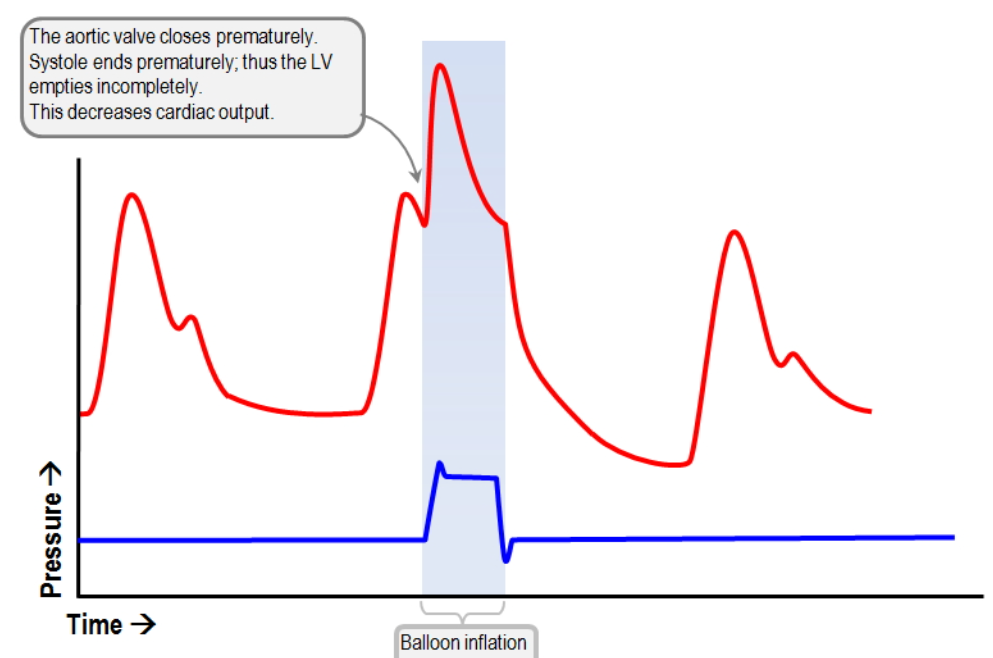
- Early inflation → ↑ afterload
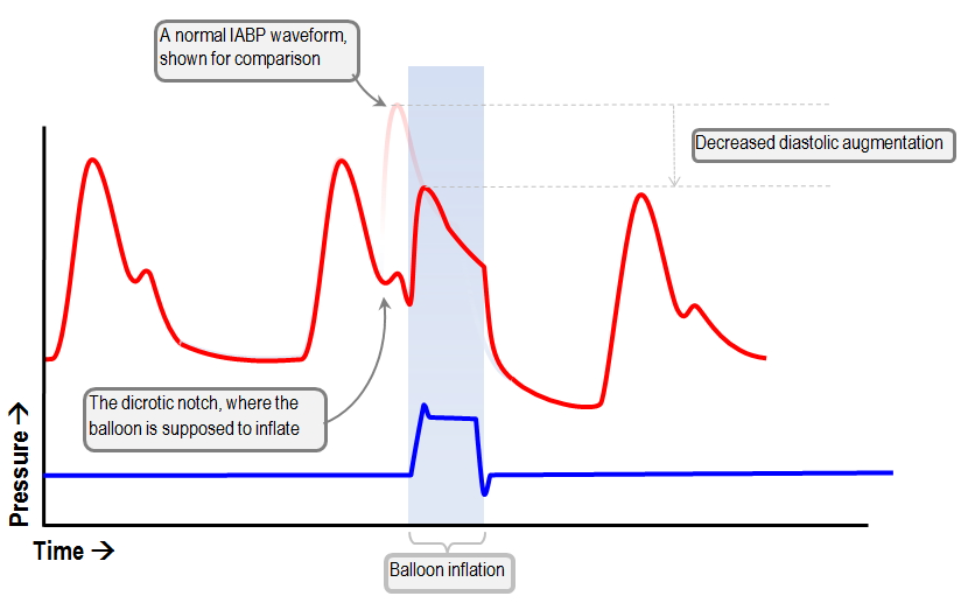
- Late inflation → ↓ diastolic augmentation
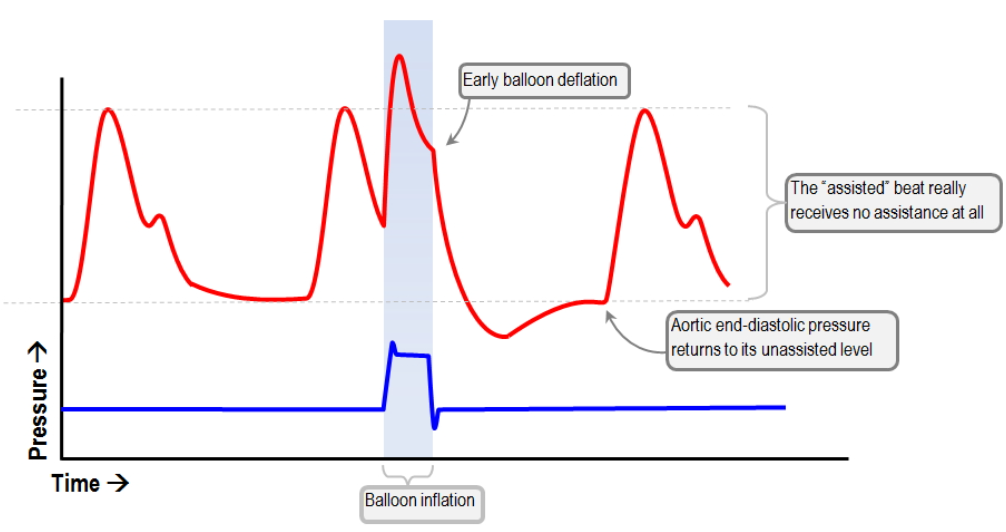
- Early deflation → ↓ O₂ demand benefit
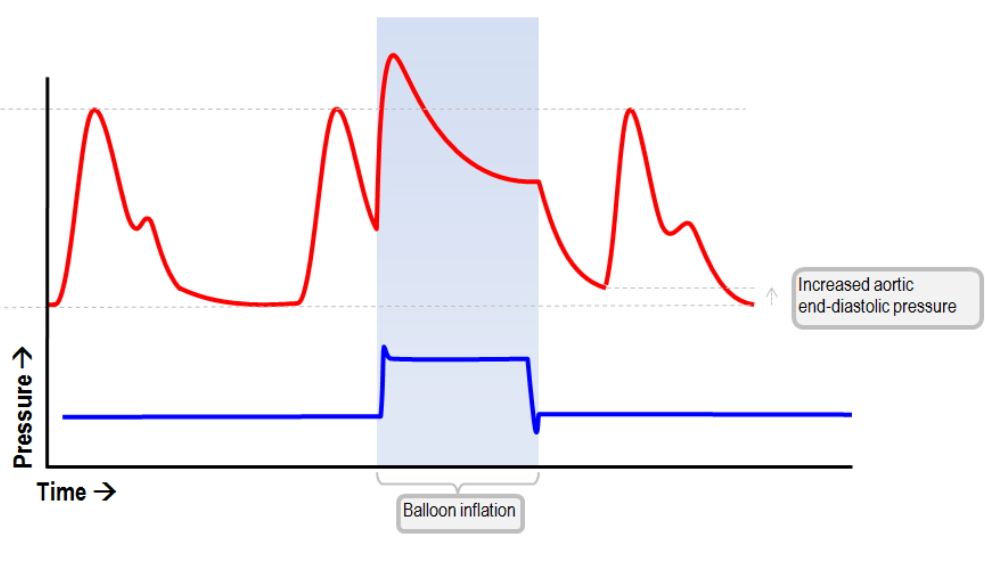
- Late deflation → ↑ afterload
- Poor timing → ↓ perfusion
Target ratio: 1:2 mode for initial assessment
Augmentation & Weaning
- Default mode: 1:1 augmentation (every cardiac cycle)
- Can be adjusted to:
- 1:2 (every other beat)
- 1:3 (every third beat)
- Weaning: Gradual reduction (1:1 → 1:2 → 1:3) over 6–12 hours
- Note: In 1:3 mode, coronary perfusion benefit may be negligible.
Monitoring and Position Confirmation
- Renal blood flow should improve post-insertion. Persistent oliguria or no improvement → suspect malposition.
Complications
- Bleeding
- Thrombosis
- Limb ischemia
- Aortic dissection
- Infection
- Balloon rupture → risk of helium gas embolism
- Cardiac tamponade
- Haemolysis
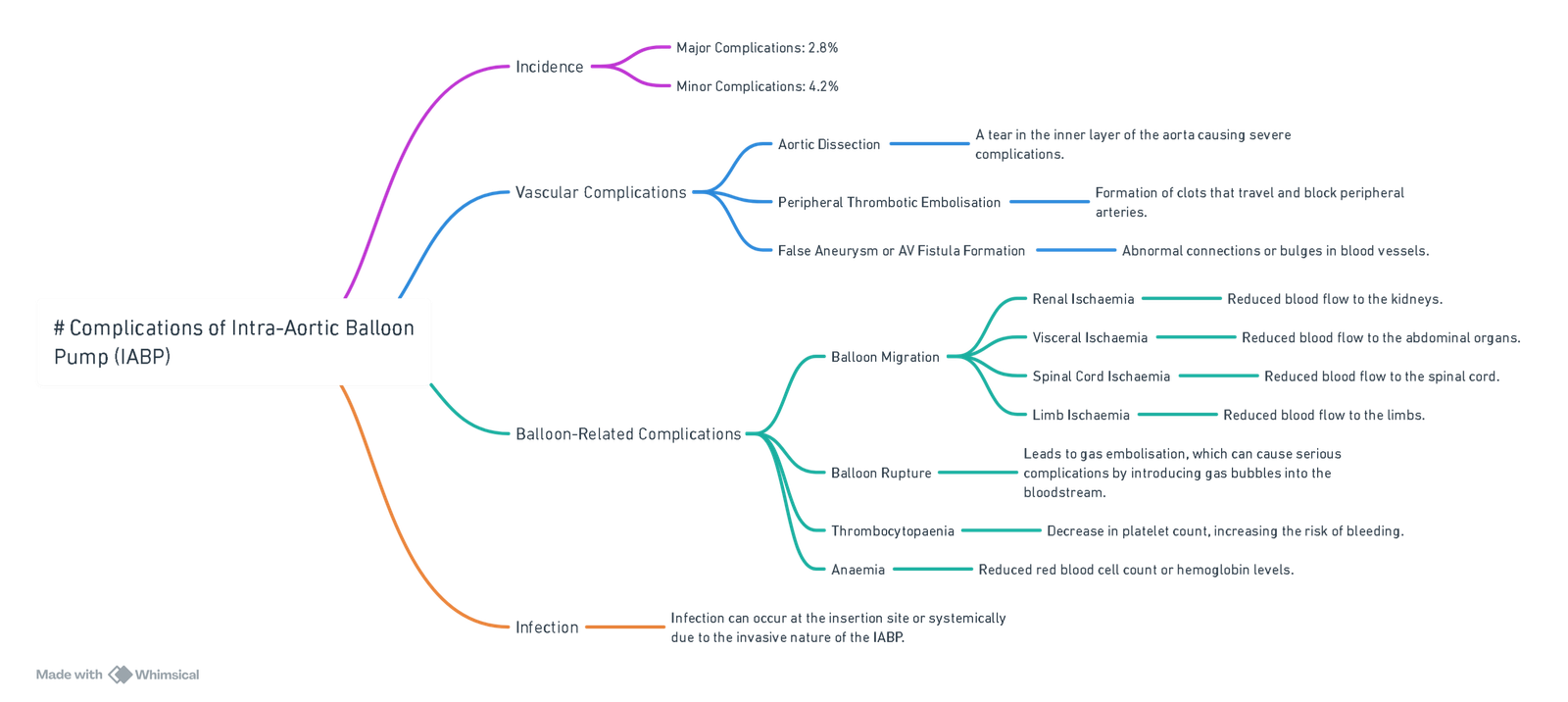
View or edit this diagram in Whimsical.
Anticoagulation
- Routine anticoagulation not required in 1:1 support.
- Consider anticoagulation in 1:2 or 1:3 modes due to ↑ thrombotic risk.
ECG and Pressure Waveform Interpretation
Features
- Augmented diastolic pressure: Post-inflation
- Assisted systolic pressure: ↓ compared to unassisted
- “V” shape at dicrotic notch = proper timing
Abnormal Waveforms
Early Balloon Inflation Results in Increased Afterload
Late Balloon Inflation Results in Decreased Diastolic Augmentation
Early Balloon Deflation Fails to Decrease Myocardial Oxygen Demand
Late Balloon Deflation Increases Afterload
Poor Diastolic Augmentation Results in Suboptimal Coronary Perfusion
Early Inflation and Late Deflation Increase Afterload; the opposite Fail to Augment
Links
References:
- Krishna, M. and Zacharowski, K. (2009). Principles of intra-aortic balloon pump counterpulsation. Continuing Education in Anaesthesia Critical Care &Amp; Pain, 9(1), 24-28. https://doi.org/10.1093/bjaceaccp/mkn051
- Figaro R, Thornton I, Scott JP, Sluhoski J. Anesthetic Management of Intra-aortic Balloon Pump-Induced Systolic Anterior Motion of the Mitral Valve During Coronary Artery Bypass Grafting. Cureus. 2024 Mar 24;16(3):e56815. doi: 10.7759/cureus.56815. PMID: 38654781; PMCID: PMC11036903.
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- ICU One Pager. (2024). Retrieved June 5, 2024, from https://onepagericu.com/
Summaries:
ICU_One_pager_IABP.pdf (squarespace.com)
IABP
Cardiothoracic anaesthesia video
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “58730334-30b9-4c56-8d96-bc6ccdbe7171”



