{}
Anaesthesia for the Cardiac Catheterisation Laboratory (“Cath Lab”)
Environmental & Safety Challenges (NORA)
| Issue | Anaesthetic implications & mitigation |
|---|---|
| Radiation | Annual occupational limit 20 mSv (ICRP 2020); wear 0.5 mmPb apron + thyroid collar, keep ≥ 2 m from X-ray source, stand behind ceiling-mounted acrylic shield; document personal dosimetry. |
| Remote location | Check crash cart, airway cart and defibrillator before first case; arrange skilled runner to theatre/ICU. |
| Restricted access & cramped workspace | Tuck arms or abduct < 90°, secure lines with 360° visibility, use extra-long circuits (3 m) and extension sets. |
| Cold ambient temperature | Forced-air warmer, warmed fluids; inadvertent hypothermia → coagulopathy & shivering artefacts during mapping. |
| Inexperienced assistants | Pre-case briefing on airway plan, ACT targets, cardioversion/pacing drills, allergic reactions. |
Radiation & Contrast Practice
| Parameter | Current recommendation (2024) |
|---|---|
| Scatter dose | 2–4 mSv yr⁻¹ typical with shielding; double without. |
| ALARA | Collimate beam, minimise fluoroscopy time, prefer low-dose & fluoroscopy-store modes. |
| Iodinated contrast | Iohexol, iopromide or iodixanol; hydrate high-risk patients; metformin may be continued if eGFR ≥ 30 mL min⁻¹ and patient haemodynamically stable. |
| ACT targets | Left-side PCI 250–300 s; complex structural (TAVR, LAAC, MitraClip) 300–350 s; heparin reversal with protamine 0.5–1 mg per 100 IU at procedure end if bleeding risk. |
General Anaesthetic Principles
| Phase | Key actions |
|---|---|
| Pre-procedure | Full airway & comorbidity review; recent creatinine; confirm anticoagulant management plan (DOAC stop 24 h standard risk, 48–72 h if renal impairment). |
| Induction | In adjacent anaesthetic bay; rapid-acting IV induction (propofol ± etomidate for EF < 30 %); secure airway before transfer unless purely MAC. |
| Maintenance | TIVA Remifentanil 0.05–0.2 µg kg⁻¹ min⁻¹ + propofol infusion ± HFNO; BIS target 45–60 to avoid patient movement or 0.8–1 MAC sevoflurane |
| Monitoring | Standard ASA + capnography; invasive A-line for TAVR, trans-septal puncture, pulmonary hypertension or LV assist cases; TOE if structural guidance. |
| Anticoagulation | Check ACT 5 min after initial heparin bolus (70–100 IU kg⁻¹) then q 30 min. |
| Immobilisation | Avoid neuromuscular block when phrenic nerve pacing/monitoring (atrial flutter, cryo-AF) is required; otherwise low-dose rocuronium enhances image stability. |
Procedure-Specific Notes
Diagnostic Coronary Angiography / PCI
- Usually LA ± fentanyl 50 µg; TIVA with propofol 25–75 µg kg⁻¹ min⁻¹ for anxious patients.
- Radial access preferred → lower bleeding & earlier ambulation.
- Treat contrast-induced spasm with IV nitrates 100–200 µg.
Structural Heart Interventions
| Procedure | Anaesthetic choice | Pearls / pitfalls |
|---|---|---|
| TAVR (average age 84 yr) | GA or conscious sedation; recent RCTs (SOLVE-TAVI, 2023 meta-analysis) show lower 30-d mortality & shorter LOS with conscious sedation when feasible. | GA still advised for alternative access (axillary, trans-apical), unfavourable airway, severe frailty, need for TOE. Rapid-pacing via RV wire 180–200 bpm. |
| Balloon mitral / pulmonary valvotomy | GA with ETT; TOE guidance; anticipate pulmonary oedema on balloon inflation; keep FiO₂ 0.4. | |
| MitraClip / TriClip | GA mandatory (continuous TOE, trans-septal puncture). Maintain MAP 65–75 mmHg for clip stability. | |
| Left-atrial-appendage closure (Watchman/Amulet) | GA with TOE or intracardiac echo; reversed heparin at end; post-op DOAC + aspirin per protocol. | |
| Trans-catheter pulmonary valve (Melody/Harmony) | Paediatric/ACHD cohort; GA, muscle relaxation, FiO₂ 0.3–0.4 to permit TOE. Prepare for RVOT arrhythmias. |
Electrophysiology (EP) & Ablation
| Ablation type | Anaesthesia | Specific considerations |
|---|---|---|
| AF radiofrequency or cryo-balloon | GA (TIVA) preferred–↓ patient motion → ↑ success and ↓ fluoro time (MANTRA-PAF update 2022). | Avoid volatile-induced QT prolongation; no NMB if diaphragmatic/phrenic integrity testing. |
| VT ablation in structural heart disease | GA with secure airway; invasive BP + arterial waveform for sympathetic surges. Have external cardioversion pads and isoprenaline & phenylephrine ready. | |
| CIED extraction | GA; large-bore IV x2; blood products on hold; consider TOE to detect tamponade. |
Complication Recognition & Rescue
| Complication | Early sign | Management |
|---|---|---|
| Cardiac tamponade | Sudden hypotension, ↓ ETCO₂, electrical alternans | Stop anticoagulation, IV fluids, phenylephrine; bedside echo; pericardiocentesis < 5 min. |
| Air / thrombo-embolism | ST-elevation, desaturation | 100 % O₂, heparin, aspiration via catheter; consider intra-coronary adrenaline. |
| Contrast anaphylaxis | Urticaria → bronchospasm | Stop contrast, IM adrenaline 10 µg kg⁻¹ (max 0.5 mg), IV fluids, H₁/H₂ antagonists. |
| High-grade AV block | Bradycardia/asystole | Atropine 0.5 mg, trans-venous pacing wire or external pads; treat electrolytes. |
| Radiation skin injury | Procedure > 5 h, peak‐skin dose > 5 Gy | Document dose; inform patient; dermatology follow-up. |
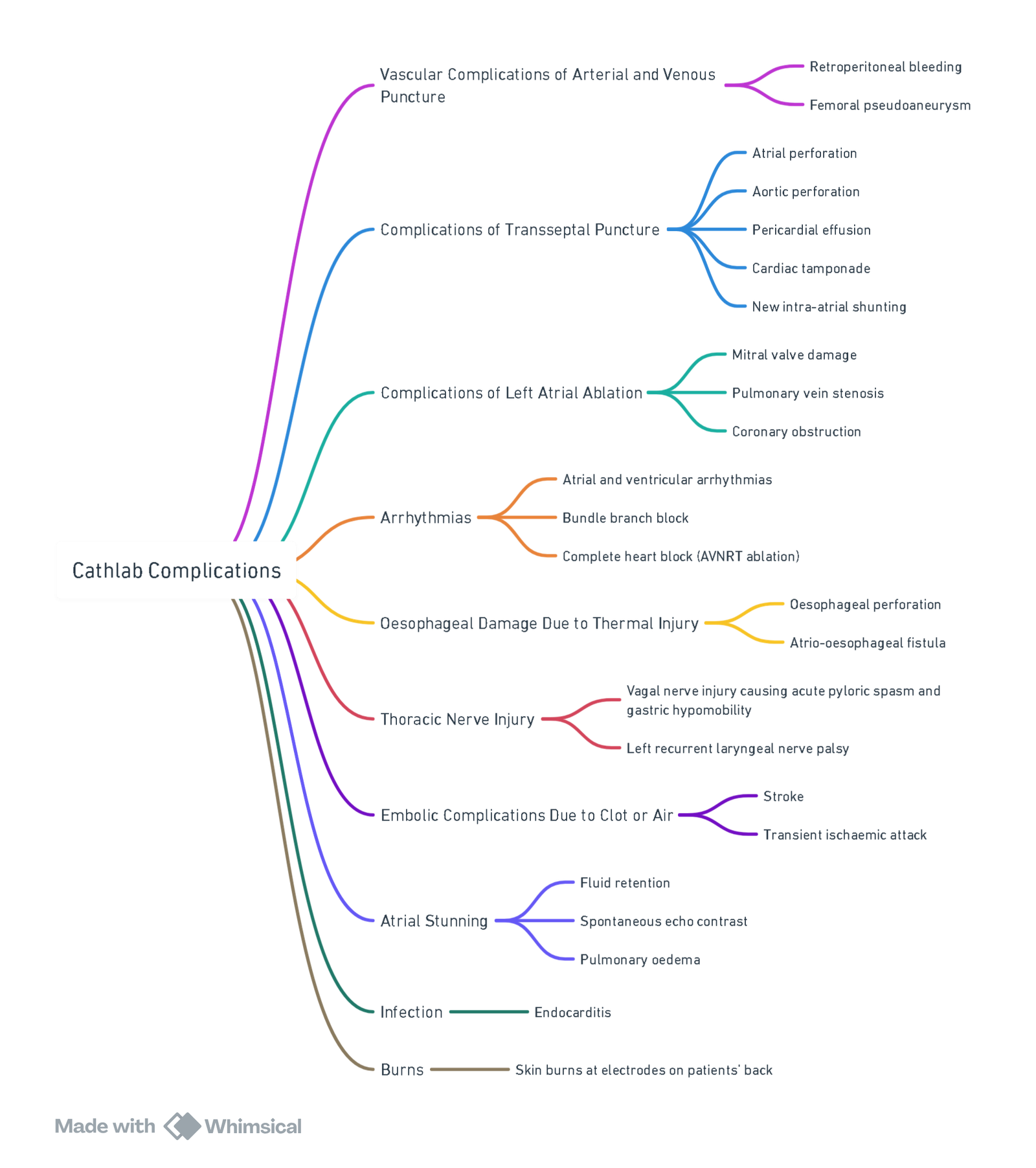
View or edit this diagram in Whimsical.
Post-procedural Care
- Extubate in lab if haemodynamically stable and ACT < 180 s; otherwise transfer intubated to ICU.
- Observe in recovery with SpO₂, ECG, puncture-site checks q 15 min × 1 h, then hourly.
- Resume DOAC 12 h after sheath removal (institutional protocol); dual antiplatelet therapy per cardiology.
Links
- Remote anaesthesia
- Endovascular Abdominal Aortic Aneurysm Repair (EVAR)
- Stroke
- Neuroradiology
- Off Pump CABG
References:
- Shetti AN, Karigar SL, Mustilwar RG, Singh DR, Nag K. Anesthesiologist in cardiac catheterization laboratory; the roles and goals!! A postgraduate educational review [corrected]. Anesth Essays Res. 2017 Oct-Dec;11(4):811-815. doi: 10.4103/0259-1162.186866. Erratum in: Anesth Essays Res. 2017 Oct-Dec;11(4):1129. doi: 10.4103/0259-1162.219355. PMID: 29284831; PMCID: PMC5735470.
- Lakkireddy D, et al. Anesthesia and AF ablation outcome: MANTRA-PAF 10-year follow-up. JACC EP 2022;8:1215
- Zawar P, et al. Conscious sedation vs general anaesthesia in TAVR: updated meta-analysis. Heart 2023;109:1372-80.
- Cholley B, et al. SOLVE-TAVI trial: anaesthesia strategy outcomes. Eur Heart J 2022;43:299-308.
- Bessoudo M, et al. Radiation dose reduction in EP labs–2024 EHRA consensus. Europace 2024;26:1045-60.
- ACR Committee on Contrast Media. Manual on Contrast Media v17. Reston (VA); 2024.
- ASA Task Force. Practice guidelines for moderate sedation/analgesia in NORA. Anesthesiology 2023;139:479-505.
- Nihoyannopoulos P, et al. Anaesthesia for structural heart interventions–BJA Education 2022;22:513-22.
- Hulme, A. P., Tharion, J. G., & Cordery, R. A. (2024). Anaesthesia in the cardiac catheterization laboratory. Anaesthesia &Amp; Intensive Care Medicine, 25(3), 198-206. https://doi.org/10.1016/j.mpaic.2024.01.013
- Hamid A. Anesthesia for cardiac catheterization procedures. Heart Lung Vessel. 2014;6(4):225-31. PMID: 25436204; PMCID: PMC4246841.
- Kemp – 2018 – Anaesthesia and the cardiac catheterisation laboratory.(https://www.sajaa.co.za/index.php/sajaa/article/view/2113)
Summaries:
Cath lab anaesthesia-video
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “53b5dc31-d2ae-4703-bd5b-2b08200c9869”



