{}
Summary of Considerations
- Patient considerations: Baseline, aspiration risk, ability to lay flat ⇒ Sedation vs GA
- Procedural considerations: Nature, duration, pain, position, immobility requirement, complications
- Environmental and Equipment considerations: Ward-based vs Mobile vs Hybrid vs OR
- Post-Anaesthesia care: Equipment, personnel, discharge criteria
Non-Operating Room Anaesthesia (NORA)
Introduction
- Definition–NORA is the delivery of anaesthetic or sedation care in locations other than a conventional operating theatre (e.g. endoscopy, cardiac catheterisation, interventional radiology, MRI, Etc suites, office-based facilities).
- Epidemiology–The proportion of anaesthetics undertaken in remote locations continues to rise: 28 % of all US anaesthetics were NORA in 2010 and 36 % in 2014, with modelling predicting > 50 % within the next decade.
- Risk profile–Recent closed-claim reviews confirm that severe respiratory events (hypoventilation, hypoxaemia, aspiration) remain the leading cause of morbidity and mortality in NORA; more than half of fatal NORA claims are judged preventable with better monitoring. Average indemnity payments are ≈ 45 % higher than for OR claims, reflecting the higher incidence of catastrophic brain injury and death.
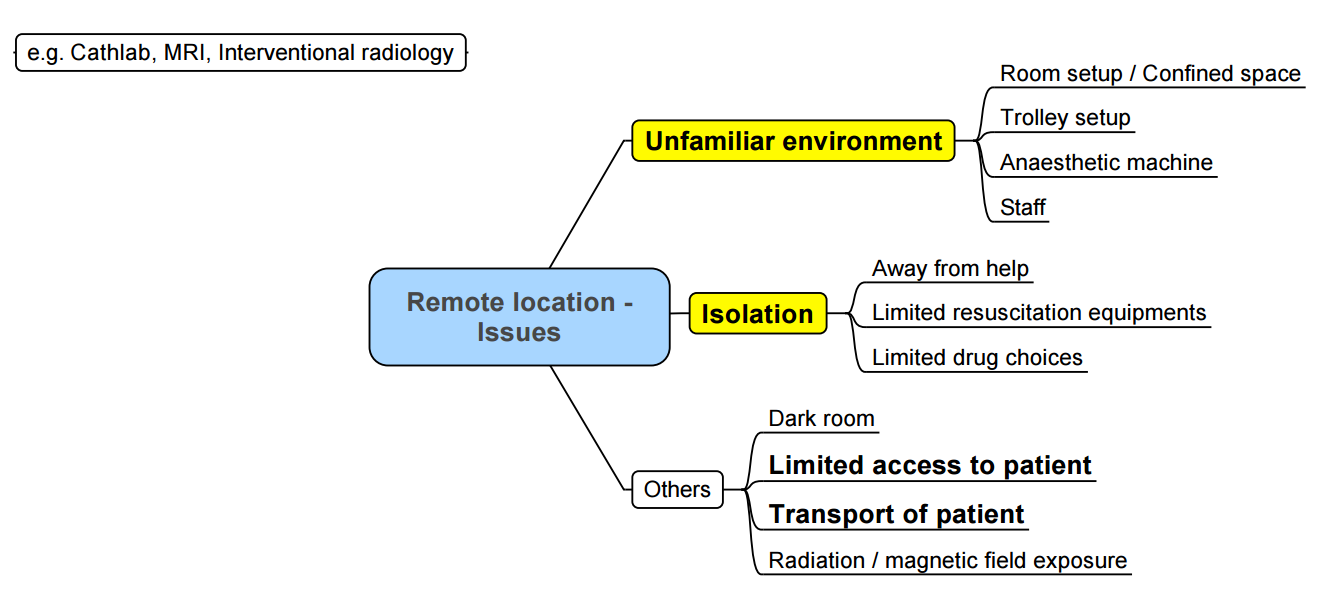
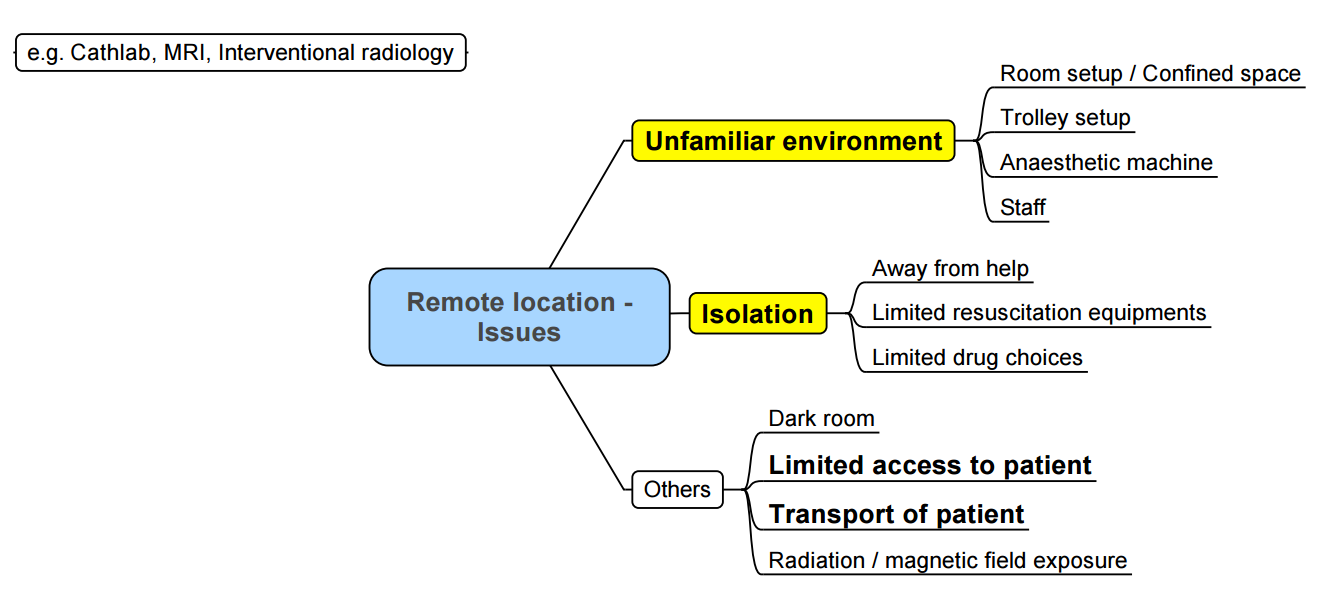
- Contributory factors–remote geography, unfamiliar staff, cramped rooms, limited access to the airway, radiation hazards, ageing/comorbid patients and high case-turnover all challenge routine anaesthetic practice.
Goals of NORA
The overarching aim is safe, smooth and efficient patient care that equals OR standards.
| Stakeholder |
Key objective |
| Patient |
Minimise anxiety, pain, movement and long-term psychological trauma; maintain physiological homeostasis; achieve timely discharge. |
| Proceduralist |
Optimal procedural conditions (immobilisation, clear communication). |
| Anaesthesia team |
Robust pre-assessment, evidence-based technique, continuous presence, zero harm. |
| Nursing/technicians |
Prepared environment, checklist compliance, rapid escalation pathways. |
| Administration |
Adequate staffing, equipment and budget aligned to case volume. |
A multidisciplinary, checklist-driven approach is mandatory.
Contemporary Safety Data
| Finding (2017-2025 literature) |
NORA vs OR |
| Respiratory complications (airway/ventilation/aspiration) |
Most common NORA injury (≈ 1 in 3 claims) |
| Catastrophic outcome (death/permanent brain damage) |
Higher proportion in NORA closed claims |
| Indemnity payment size |
44 % higher for NORA claims |
| Cardiovascular instability |
Similar frequency, but concentrated in interventional cardiology/radiology suites |
| Nerve or positioning injuries |
Less common in NORA than OR |
- Respiratory compromise under monitored anaesthesia care (MAC) and deep sedation accounts for the majority of adverse events; capnography markedly reduces unrecognised hypoventilation and is now a standard of care.
Classification of Complications
- Minor: inadequate depth of anaesthesia/sedation, PONV, transient haemodynamic swings, mild hypothermia, line-related issues.
- Major: cardiorespiratory arrest, aspiration, anaphylaxis, awareness, severe airway events, wrong-patient/site, burns/falls, neurological injury, escalation to unplanned ICU admission.
Equipment & Environment—SOAPME
| Letter |
Requirement |
| S–Suction |
Two working suction sources; wide-bore Yankauer and paediatric catheters. |
| O–Oxygen |
Primary pipeline supply and full E-cylinder (≥ 2000 psi) onsite, with low-pressure alarm. |
| A–Airway |
Age-appropriate BVM, oral/nasopharyngeal airways, videolaryngoscope, second-generation supraglottic airway, ETTs with stylets/bougie; cricothyrotomy kit if help is distant. |
| P–Pharmacy |
Immediate-use drugs (vasopressors, anticholinergics, sedatives, neuromuscular blockers, reversal agents) stored in tamper-evident tackle box; emergency dantrolene if a volatile agent is available. |
| M–Monitors |
Continuous ECG, NIBP, SpO₂, capnography (mandatory for all moderate/deep sedation and GA), inspired O₂, temperature; audible alarms on. |
| E–Everything else |
OR-equivalent anaesthesia machine with waste-gas scavenging, defibrillator/ pacing pads, forced-air warmer, radiation shielding (where relevant), compliant electrical outlets, reliable two-way communication with main theatre, adequate lighting. |
NORA Safety Time-Out (checklist excerpt)
- Patient–identity, ASA class, weight, fasting status, allergies, relevant labs/imaging.
- Procedure–site/side, position, radiation precautions, anticipated duration.
- Anaesthesia–machine check complete, airway plan (primary & rescue), anticipated blood loss, post-procedure disposition.
- Team roles–introduce all staff; clarify who calls for help.
- Emergency–crash-cart location, code activation number, transport route to OR/ICU.
Minimum Safety Requirements for Remote Anaesthesia (NORA)
Synthesised from ASA Statement on Non‑Operating‑Room Anaesthesia 2023; SASA Procedural Sedation Guidelines 2020‑2025 (adult) & 2021‑2026 (paediatric); SASA Practice Guidelines 2022; HPCSA Ethical Guidance 2022
Personnel & Qualifications
- Anaesthesia provider: HPCSA‑registered specialist anaesthesiologist or medical officer with documented NORA competence; must remain continuously present.
- Assistant: At least one dedicated, trained assistant (anaesthetic nurse/ODA) present throughout, solely for patient care and capable of initiating life‑support.
- Sedationists (non‑anaesthetists) must comply with SASA Sedation Guidelines, hold recognised sedation training, maintain a logbook and current CPD; deep sedation outside anaesthesiologist scope is not permitted.
- Support services: Immediate access to senior airway backup, blood bank and rapid patient transfer pathway to theatre/ICU.
Environment & Equipment
- Procedure room sized to allow 360° patient access; minimum two independent electrical circuits and piped or cylinder O₂ with two independent sources plus back‑up suction.
- Essential equipment (equivalent to OR standards):
- Self‑inflating bag–valve–mask (+ PEEP valve) able to deliver > 90 % O₂.
- Full difficult‑airway cart (video laryngoscope, supraglottic devices, cricothyrotomy kit).
- Defibrillator, drug infuser/syringe pumps, non‑invasive haemodynamic monitor, rapid‑warmer/forced‑air heater.
- MRI‑ / radiation‑compatible equipment where applicable.
- Drug inventory: emergency vasoactives, sugammadex, dantrolene (if volatile agents used) stored with checklists and temperature logs.
- Documented pre‑use equipment check before first case each day and between cases.
Monitoring (minimum continuous)
| Parameter |
Minimal sedation |
Moderate–deep sedation / GA |
| SpO₂ & audible pulse tone |
✓ |
✓ |
| NIBP q5 min (automatic) |
✓ |
✓ |
| 3‑lead ECG |
— |
✓ |
| Capnography |
— |
✓ (mandatory) |
| Inspired/expired agent |
— |
✓ if volatile |
| Temperature |
if >30 min |
✓ |
| Neuromuscular function |
— |
✓ if NMB used |
- Alarms must be audible in room and recovery area with limits pre‑set and never silenced.
Post‑Anaesthesia Care
- Dedicated recovery area meeting operating‑theatre PACU standards; staff‑to‑patient ratio ≤ 1 : 2 for adults (1 : 1 for children < 8 y).
- Continuous SpO₂, ECG, NIBP and capnography in deeply sedated/GA patients until fully awake.
- Discharge when modified Aldrete ≥ 9 (or Paediatric Post‑Anaesthesia Score ≥ 12), pain < 4/10, emesis controlled and escort available.
- Written emergency contact and 24‑h helpline provided to all day‑case patients.
Documentation & Legal Requirements
- Separate written informed consent covering anaesthesia, remote‑location risks and radiation/contrast where relevant.
- Standardised anaesthetic record incorporating WHO Safe Surgery/NORA checklist, capnography trace, drug & fluid chart, adverse‑event log.
- Daily equipment & drug‑temperature logs; incident reporting to institutional governance and HPCSA where applicable.
- Practitioners must carry adequate malpractice indemnity and comply with HPCSA Good Practice Booklets (1, 2, 5, 10).
- Records kept ≥ 6 years (minors: until age 21 y + 3 y); electronic records must be password‑protected and auditable.
Quality Assurance & Training
- Annual simulation of fire, power failure, MRI quench, airway crisis and massive haemorrhage.
- Morbidity–mortality and NORA incident review ≥ quarterly; data submitted to SASA National Audit when requested.
- Competency‑based continuing professional development: minimum 50 CPD points / 2 years including airway & sedation modules.
Conduct of Anaesthesia for NORA
Pre-operative Planning
- Familiarize yourself with the venue–route for patient transfer, power supply, gas outlets, cell-phone “dead spots”, radiation or MRI restrictions.
- Understand the procedure–position, expected duration, need for absolute immobility, potential for large fluid shifts or blood loss
- Optimise the patient–full medical history, fasting status, investigation review and targeted optimisation (e.g. iron therapy for anaemia, glycaemic control, treatment of acute sepsis).
- A structured checklist (location, procedure, personnel, patient, plan B) completed before the list starts reduces last-minute delays and near-misses.
Patient Selection & risk Stratification
| High-risk features |
Examples |
Action |
| Extremes of age |
< 2 years; > 75 years |
Consultant cover, capnography, temperature control |
| ASA ≥ III / significant cardiorespiratory disease |
CAD, heart failure, severe COPD, pulmonary hypertension |
Pre-op anaesthesia consult, optimisation, invasive monitoring if needed |
| Difficult airway predictors |
Cranio-facial abnormality, OSA, limited neck movement |
Videolaryngoscope, second-generation SGA, rescue kit |
| Obesity (BMI > 35 kg m⁻²) |
Often co-existing OSA |
Ramp position, high-flow nasal oxygen, delayed emergence plan |
| Emergency/after-hours cases |
Haemorrhage, sepsis |
Activate full theatre response team |
| Pregnancy, pacemaker/ICD, MH history, substance dependence, failed previous sedation |
|
Mandatory anaesthetist involvement |
- Endocarditis prophylaxis–unchanged from 2023 AHA/ACC guidance: prosthetic valves, previous infective endocarditis, selected congenital heart disease and cardiac transplant recipients with valvulopathy.
Peri-operative Medication Management (day-case or short GA)
| Drug / class |
Continue |
| Aspirin & P2Y₁₂ inhibitors |
unless neuraxial, ophthalmic or skull-base surgery–liaise with proceduralist |
| β-blockers, calcium-channel blockers |
morning dose with sip of water |
| ACE-Is / ARBs |
Hold morning dose if general anaesthesia or expected fluid shifts (reduces refractory hypotension) |
| Diuretics |
Omit morning dose (↓ intravascular depletion) |
| SGLT-2 inhibitors |
Stop 3 days pre-procedure to avoid euglycaemic keto-acidosis |
| Oral hypoglycaemics |
Hold on day; stop metformin if eGFR < 30 mL min⁻¹ 1.73 m⁻² or intra-arterial contrast |
| Insulin |
Give 50 % usual long-acting dose; omit rapid-acting; schedule first on list |
| Anticoagulants |
Follow local bridging protocol (CHADS-VASC, procedure bleeding risk) |
| Inhalers, anti-epileptics, anti-Parkinsonian drugs, steroids, opioids |
Continue and bring to hospital |
| Herbal / OTC supplements |
Stop ≥ 7 days prior (variable platelet effect) |
Monitoring
- Apply ASA Basic Monitoring plus:
- Continuous capnography for all deep sedation and GA (SASA Adult Sedation Guidelines 2020–2025).
- Core temperature for cases > 30 min or infants.
- Neuromuscular function if paralytics used.
- In MRI: use MRI-compatible NIBP, pulse oximetry and gas sampling extensions.
- ASA basic monitoring: Oxygenation, ventilation, Circulation, temperature
Anaesthetic Technique
Desired Attributes
- Rapid onset, titratability, haemodynamic stability, minimal respiratory depression, short recovery and low PONV incidence. A dedicated anaesthesia provider must be able to rescue a patient who drifts to a deeper level than intended.
Common Agents (adult Doses Are Titrated to effect)
| Drug |
Typical bolus / infusion |
Onset |
Recovery* |
Comments |
| Propofol |
0.5–1 mg kg⁻¹ bolus then 50–150 µg kg⁻¹ min⁻¹ |
< 1 min |
5–15 min |
Gold-standard; hypotension, injection pain |
| Remimazolam |
5 mg over 1 min then 2.5 mg as needed / 3–10 µg kg⁻¹ min⁻¹ |
1–2 min |
10 min |
Organ-independent metabolism; reversed with flumazenil; lower cardiovascular depression |
| Dexmedetomidine |
0.5–1 µg kg⁻¹ over 10 min then 0.4–1 µg kg⁻¹ h⁻¹ |
10 min |
20–30 min |
Analgesia, minimal respiratory effect; brady-hypotension, longer discharge time |
| Ketamine |
0.25–0.5 mg kg⁻¹ bolus / 0.2 mg kg⁻¹ h⁻¹ |
30 s |
10–20 min |
Sympathomimetic, preserves airway; psychomimetic – use with midazolam |
| Etomidate |
0.2 mg kg⁻¹ bolus |
30 s |
5–10 min |
Haemodynamic stability; adrenal suppression limits infusions |
*Awakening after brief infusion (context-sensitive half-time).
Continuum of Depth of Anaesthesia (ASA 2018)
| – |
Minimal |
Moderate |
Deep |
General |
| Responsiveness |
Normal |
Purposeful to verbal/tactile stimulus |
Purposeful after repeated/painful stimulus |
None |
| Airway |
Unaffected |
Maintained |
May require assistance |
Often requires device |
| Ventilation |
Unaffected |
Adequate |
May be inadequate |
Frequently inadequate |
| Cardiovascular |
Unaffected |
Usually maintained |
Usually maintained |
May be impaired |
Medication Safety
- Most NORA drug errors stem from unfamiliar layouts and rapid turnover. Mitigation: pre-filled colour-coded syringes, barcode scanning, two-person check for high-alert meds, and a “just culture” incident-reporting system.
Iodinated Contrast & Kidney Injury
- Terminology: post-contrast acute kidney injury (PC-AKI). Current evidence shows IV contrast seldom causes clinically significant AKI when eGFR ≥ 30 mL min⁻¹ 1.73 m⁻².
| eGFR (mL min⁻¹ 1.73 m²) |
PC-AKI risk |
Prophylaxis |
| ≥ 45 |
Very low |
None |
| 30–44 |
Low (IV) / Moderate (intra-arterial first-pass) |
IV isotonic saline 1 mL kg⁻¹ h⁻¹ for 3 h pre- & 6 h post-procedure |
| < 30 or AKI |
High |
Hydration ± sodium bicarbonate; discuss contrast volume; consider non-contrast imaging |
- N-acetylcysteine–not recommended (no proven benefit).
- Hold nephrotoxics (NSAIDs, ACE-I/ARB, SGLT-2 inhibitors) on day of contrast if eGFR < 45.
- Dialysis patients: schedule usual dialysis after contrast, no extra hydration needed.
NORA by Specific Locations
The same airway, monitoring and staffing standards that apply in the operating theatre must follow the patient to every remote location.
Common NORA Venues
| Imaging & Therapy |
Endoscopy |
Cardiac |
Miscellaneous |
| Interventional radiology, CT, MRI, nuclear medicine, radiation oncology |
Upper & lower GI endoscopy, ERCP, EUS |
Cath-lab, electrophysiology, structural heart (TAVI, MitraClip), TOE |
Lithotripsy, electro-convulsive therapy, emergency department, ICU, labour ward, ward bedside procedures |
Location-specific Considerations
Gastrointestinal Endoscopy
- Shared airway & aspiration risk
- Topical lignocaine abolishes the gag reflex; large-bore endoscopes occlude > 50 % of the oropharyngeal cross-section.
- Positioning
- ERCP often prone or semi-prone; secure all lines before turning.
- Technique pointers
- Propofol TCI ± short-acting opioid is usual; secure the airway (second-generation supraglottic or ETT) if ASA ≥ III, BMI > 40 kg m⁻², anticipated prolonged ERCP or GI bleed.
- Continuous capnography and audible SpO₂ alarms are mandatory.
- Observe strict 2 h clear-fluid / 6 h solids fasting despite bowel prep.
- Complications
- Perforation, bleeding, post-ERCP pancreatitis: agree escalation protocol and have IV antibiotics and vasopressors ready
Cardiac Catheterisation Laboratory
- Patient profile–extremes of age with limited cardiopulmonary reserve.
- Hazards
- Arrhythmias → defibrillator pads on before draping; MgSO₄ and amiodarone drawn up.
- Anticoagulation & large-bore sheaths → cross-matched blood available; gentle emergence to avoid coughing.
- Radiation → stand > 2 m from beam, 0.5 mm Pb apron, dosimeter badge.
- Anaesthetic tips
- GA with controlled ventilation for trans-septal or structural heart work; invasive BP and central access for high-risk PCI.
- Dexmedetomidine-propofol combinations maintain haemodynamic stability for electrophysiology studies.
Magnetic Resonance Imaging (MRI)
- Safety zones
- screen staff & equipment; only MR-conditional devices cross the 5 gauss line.
- Environmental challenges
- 95 dB acoustic noise, poor access (patient 1 m inside bore), long extension lines, strong fringe fields that distort capnography traces.
- Best practice
- Induce and secure airway outside Zone IV; use long breathing circuit, MR-safe syringe pumps and fibre-optic SpO₂ cable.
- Keep a spare non-ferromagnetic oxygen cylinder in the room; arrest management protocol stipulates move patient to Zone II for CPR.
Paediatric NORA
- Higher metabolic rate and smaller FRC → rapid desaturation: pre-oxygenate with high-flow nasal oxygen where feasible.
- Drug safety: weight-based, double-checked doses; pre-print dilution charts.
- Preferred regimens–propofol infusion (150–250 µg kg⁻¹ min⁻¹) with natural airway; ketamine-dexmedetomidine for MRI or CT when spontaneous ventilation is essential.
- Radiation: use pulsed fluoro, thyroid shields, and document cumulative dose.
Setting-up a Remote Site — “PP-DD-SSET-CG-F” Mnemonic
| Element |
Key tasks |
| Patient |
Selection criteria, fasting & consent verified on arrival |
| Post-anaesthetic care |
PACU or ward bay with trained nurse, capnography & oxygen |
| Drugs |
Locked drug box; emergency agents (dantrolene, intralipid) on site |
| Disposables |
IV sets, airway kits, infusion lines, warming blankets |
| Sustainability |
Audit, M&M meetings, equipment maintenance schedule |
| Staff |
Named clinical lead, competency training, emergency drills |
| Equipment |
Full ASA monitors, OR-equivalent machine, scavenging |
| Transfer |
Protocol & trolley for rapid move to OR/ICU |
| Complications |
Written algorithms (MH, local-anaesthetic toxicity, anaphylaxis) |
| Guidelines |
Latest ASA/SASA/discipline-specific policies accessible |
| Finance |
Capital budgeting and ongoing supply chain plan |
Cross-cutting Challenges and Mitigation
| Domain |
Common problems |
Safety strategies |
| Equipment |
Outdated machines, limited outlets, dark/cold rooms, MR incompatibility |
Pre-procedure checklist (SOAPME), battery back-up, forced-air warming, MR-safe monitors |
| Location |
Long distance from theatre, cramped around gantries |
Clear evacuation route, portable gas & suction, slim carts, simulation of code blue |
| Staffing |
Unfamiliar nurses/techs, poor communication |
Standard briefing huddle, role cards, closed-loop communication drills |
| Procedure |
Bulky devices occlude airway, contrast reactions, high turnover |
Extra-long circuits/lines, pre-diluted adrenaline, contrast-AKI bundle, enforce turnaround time for checks |
| Patient |
Inadequate pre-assessment, unverified NPO, implants |
Pre-visit telephone screening, electronic checklist, MRI implant database cross-check |
| Radiation |
Exposure to staff, lead apron fatigue |
Time–distance–shielding principle, wrap-around apron with thyroid collar, annual dosimetry review |
Links
References:
- Chang B, Urman RD. Non-operating Room Anesthesia: The Principles of Patient Assessment and Preparation. Anesthesiol Clin. 2016 Mar;34(1):223-40. doi: 10.1016/j.anclin.2015.10.017. PMID: 26927750.
- Michael A Phelps WDB. 10-year trends in non-operating room anaesthesia case volumes at an American academic medical center. 2018.
- Lanahan JK, Desai SP. A History of Non-Operating Room Anesthesia (NORA). ASA Monitor. 2019;83(11):28-30.
- Bell C. NORA: Non-O.R. Anesthesia. ASA Newsletter. 2013;77(11):10-.
- Dabu-Bondoc SM. Standard procedures in nonoperating room anesthesia. Current Opinion in Anesthesiology. 2020;33(4):539-47.
- Nagrebetsky A, Gabriel RA, Dutton RP, Urman RD. Growth of non-operating room anaesthesia care in the United States: a contemporary trends analysis. Anesth Analg. 2017;124:1261-1267.
- Webster CS. Systems, safety, and anaesthesia outside the operating room. Br J Anaesth. 2023;131:429-431.
- Wanner A, Klimke R, Luedi MM, Urman RD. Closed claims analysis in non-operating room anaesthesia. Curr Opin Anaesthesiol. 2025;38:418-424.
- Anesthesia Patient Safety Foundation. Non-Operating Room Anaesthesia: Closed Claim Review and Analysis. APSF Newsletter. 2023;38(1):22-26.
- Chang C, Dudley R. Time-out checklists promote safety in non-operating room anaesthesia (NORA). APSF Newsletter. 2021;36(3):120-124.
- American Society of Anesthesiologists. Statement on Non-Operating Room Anaesthesia Services. ASA; 2023.
- American Society of Anesthesiologists. Standards for Basic Anesthetic Monitoring. ASA; 2020.
- Roelofse J, Jansen van Rensburg M. SASA Guidelines for the safe use of procedural sedation and analgesia for diagnostic and therapeutic procedures in adults 2020–2025. S Afr J Anaesth Analg. 2020;26(Suppl 1):S1-75.
- Roelofse J et al. SASA Paediatric guidelines for procedural sedation and analgesia 2021–2026. S Afr J Anaesth Analg. 2021;27(Suppl 2):S1-83.
- Ahuja V et al. Comparative haemodynamic effects of ciprofol and propofol during outpatient anaesthesia. JAMA Surg. 2025;160:1125-1133.
- Borkett KM, Riff DS, Schwartz HI. Remimazolam versus midazolam for procedural sedation: a randomised trial. Anesth Analg. 2024;138:702-711.
- Van der Molen AJ,; ESUR Contrast Media Safety Committee. Guidelines on PC-AKI prevention. Eur Radiol. 2023;33:2402-2415.
- Polderman JA, Hollmann MW. Dexmedetomidine for non-OR procedures: a systematic review. Br J Anaesth. 2022;129:289-301.
- Liesenfeld O, Abrams K. Ciprofol for procedural sedation–meta-analysis. Anaesthesia. 2024;79:557-568.
- Park JH et al. Withholding versus continuing ACE-Is/ARBs before surgery: outcomes meta-analysis. Anesth Analg. 2023;136:1021-1031.
- SASA. Guidelines for the Safe Use of Procedural Sedation and Analgesia in Adults 2020–2025. SASA; 2020.
- American Society of Anesthesiologists. Practice Guidelines for Moderate Procedural Sedation and Analgesia. ASA; 2018 (reaffirmed 2023).
- Mehran R, Weisbord S. Contrast-Associated AKI. N Engl J Med. 2019;380:2146-2155.
- Anesthesia Patient Safety Foundation. Remimazolam–a novel benzodiazepine. APSF Newsletter. 2023;38(3):60-64.
- Kaye AD et al. Safety of non-operating room anaesthesia: a narrative review. Curr Opin Anaesthesiol. 2025;38:425-434.
- Bader AM, Pothier MM. Out-of-operating room procedures: preprocedure assessment. Anesthesiol Clin 2009;27(1):121-6.
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- Non-Operating Room Anaesthesia: An Overview G Malleck. 2023
- Weiss MS, Fleisher LA. Non-Operating Room Anesthesia: Elsevier; 2015.
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “8221af9b-803b-45a8-ba0b-7c1a88d1d5e2”