- Endovascular Abdominal Aortic Aneurysm Repair (EVAR)
- Risk of Rupture
- Procedure
- Potential Advantages and Disadvantages of EVAR over Open Surgical Repair
- Patient Factors Favoring Endovascular or Open AAA Repair
- General Anesthesia (GA) vs. Local vs. Regional
- Major Risks and How to Prevent Them
- Conduct of Anaesthesia for EVAR
- Emergency EVAR
{}
Endovascular Abdominal Aortic Aneurysm Repair (EVAR)
Risk of Rupture
- Patients are usually offered surgery once the anteroposterior diameter reaches 5.5 cm (or aneurysm increasing by more than 5 mm in 6 months), as the risks of rupture increase considerably beyond that.
- The elective open AAA repair carries a 5% mortality, whereas the 30-day mortality associated with ruptured AAA is widely believed to be around 80%.
- The 30-day mortality with EVAR ranges from 1.7% in patients deemed fit for open repair to 9% in those deemed unfit for open repair.
- A distinction should be made between simple infra-renal EVAR and complex supra-renal EVAR, which carries a higher perioperative risk.
Annual Risk of Rupture with Size of Aneurysm
| Aneurysm Diameter (cm) | Annual Rupture Risk (%) |
|---|---|
| 4.0-4.9 | 0.5-5 |
| 5.0-5.9 | 3-15 |
| 6.0-6.9 | 10-20 |
| ≥7.0 | 20-50 |
Procedure
- EVAR involves the use of fabric or synthetic tube grafts which are self-expanding or expanded with a ballooning catheter.
- The stent grafts can be classified as “standard” stent grafts and “complex” stent grafts.
- The “complex” stent grafts can be fenestrated, branched, or chimney.
- During the procedure, the stent graft is positioned under fluoroscopic guidance overlying the aneurysm such that blood flows from the normal artery through the stent graft into the normal artery, preventing blood flow in the aneurysmal sac, which will eventually thrombose.
- Stent grafts are usually introduced through the common femoral arteries.
- Most surgeons will perform a surgical cutdown on the vessels due to the size of the sheaths.
- The fluoroscopy time and dose of contrast used tend to be higher, increasing the risk of contrast-induced nephropathy.
Potential Advantages and Disadvantages of EVAR over Open Surgical Repair
| Advantages | Disadvantages |
|---|---|
| Short-term Mortality and Morbidity | Complexity and Anesthesia |
| Aneurysm-related short-term mortality and morbidity 3% lower in the EVAR group | Complex surgery |
| Long-term mortality similar in both groups | Remote site anesthesia |
| Potential conversion to general anesthesia in a patient possibly unfit for GA | |
| Re-intervention and Cost | |
| Minimally Invasive | Increased need for re-intervention (4%) (EVAR 1 trial) |
| Less blood loss and fewer transfusions | Increased cost per case |
| Less fluid shifts | |
| Less pain | Long-term Mortality |
| Minimal cardiovascular and metabolic stress response intraoperatively | Higher all-cause and aneurysm (rupture)-related mortality beyond 8 years |
| Less hemodynamic perturbations | |
| No cross clamp | Surveillance Requirements |
| Less distal tissue ischemia | Requirement of lifelong yearly surveillance by CT scan or duplex ultrasound |
| Less end-organ damage | |
| Fewer complications: Cardiac, Pulmonary, Renal | |
| Recovery and Hospital Stay | |
| Earlier ambulation | |
| Reduced procedural time | |
| Shorter hospital stay | |
| Reduced need for intensive care facilities | |
| Survival and Operability | |
| More favorable 30-day survival | |
| May be suitable for patients otherwise considered “inoperable” | |
| Avoidance of general anesthesia (in infrarenal EVAR) |
Patient Factors Favoring Endovascular or Open AAA Repair
| Favors Open Repair | Favors EVAR |
|---|---|
| Younger patient | Older patient |
| Few medical comorbidities | Multiple medical comorbidities |
| Connective tissue disorder | Prior aortic surgery |
| Anatomy not favorable for EVAR | Prior abdominal surgery |
General Anesthesia (GA) vs. Local vs. Regional
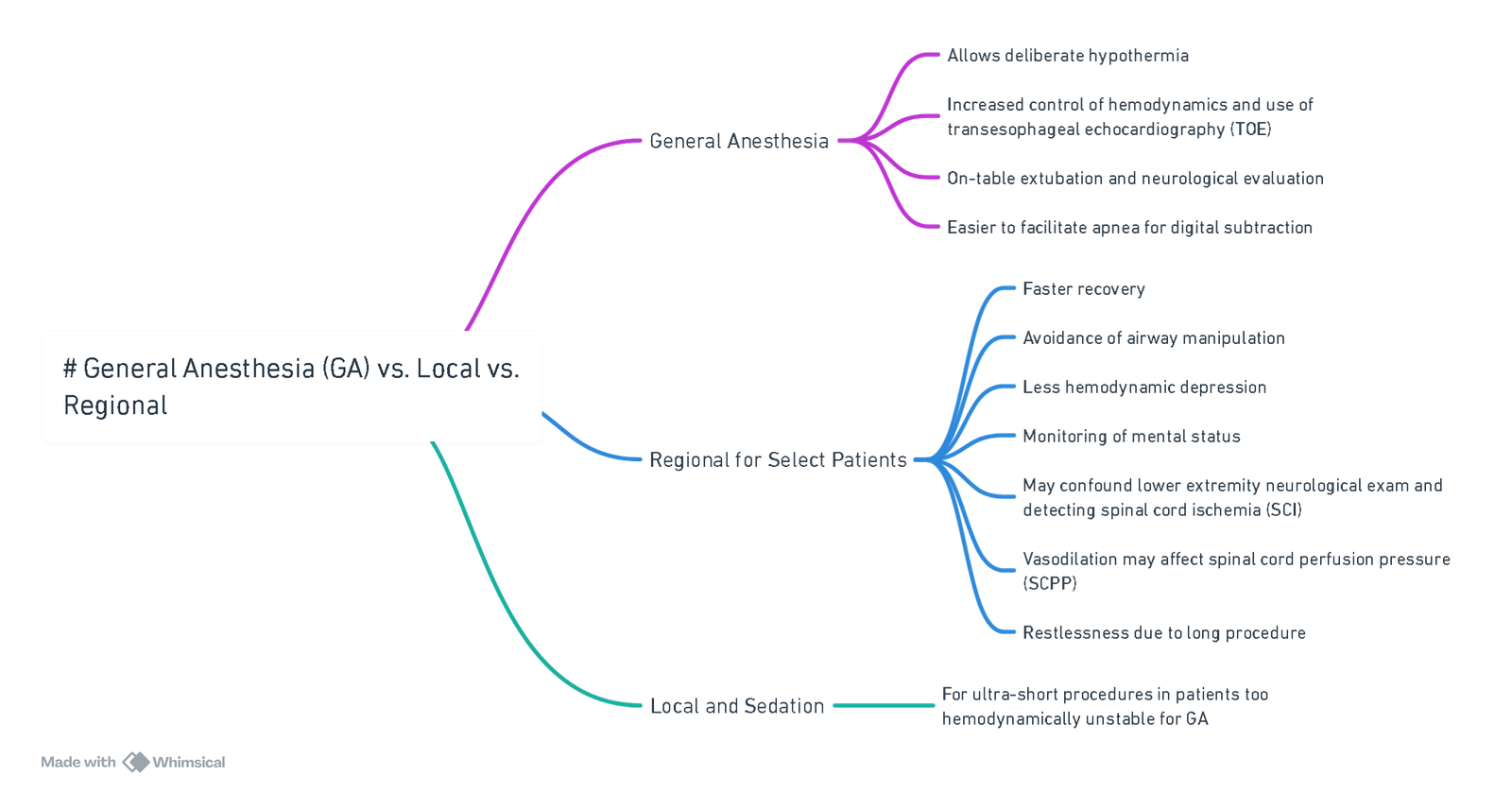
View or edit this diagram in Whimsical.
Major Risks and How to Prevent Them
- Spinal Cord Ischaemia
- Monitoring of evoked potentials: Sensory monitoring of posterior columns only; motor monitoring is technically difficult.
- Maintaining pressures:
- Mean Arterial Pressure (MAP): 90-110 mmHg after stent deployment.
- Cerebrospinal Fluid Pressure (CSFP) / Central Venous Pressure (CVP): < 10 mmHg.
- Body temperature: Maintain around 35.5°C to decrease mortality risk and paraplegia.
- Spinal (lumbar) drainage: Pre-operative drainage if there is an increased risk.
- Distal circulatory support: Use shunt, left heart bypass, or partial cardiopulmonary bypass (CPB) to maintain distal aortic pressure at 60-70 mmHg.
- Papaverine: Some evidence supports its use.
- High Risk Perioperative Acute Kidney Injury (AKI)
- Refer to renal protection strategies in the aortic surgery note.
- Aneurysm Rupture
- Invasive pressure monitoring
- Blood availability
- Large bore IV lines
- Stroke
- Cardiovascular
Conduct of Anaesthesia for EVAR
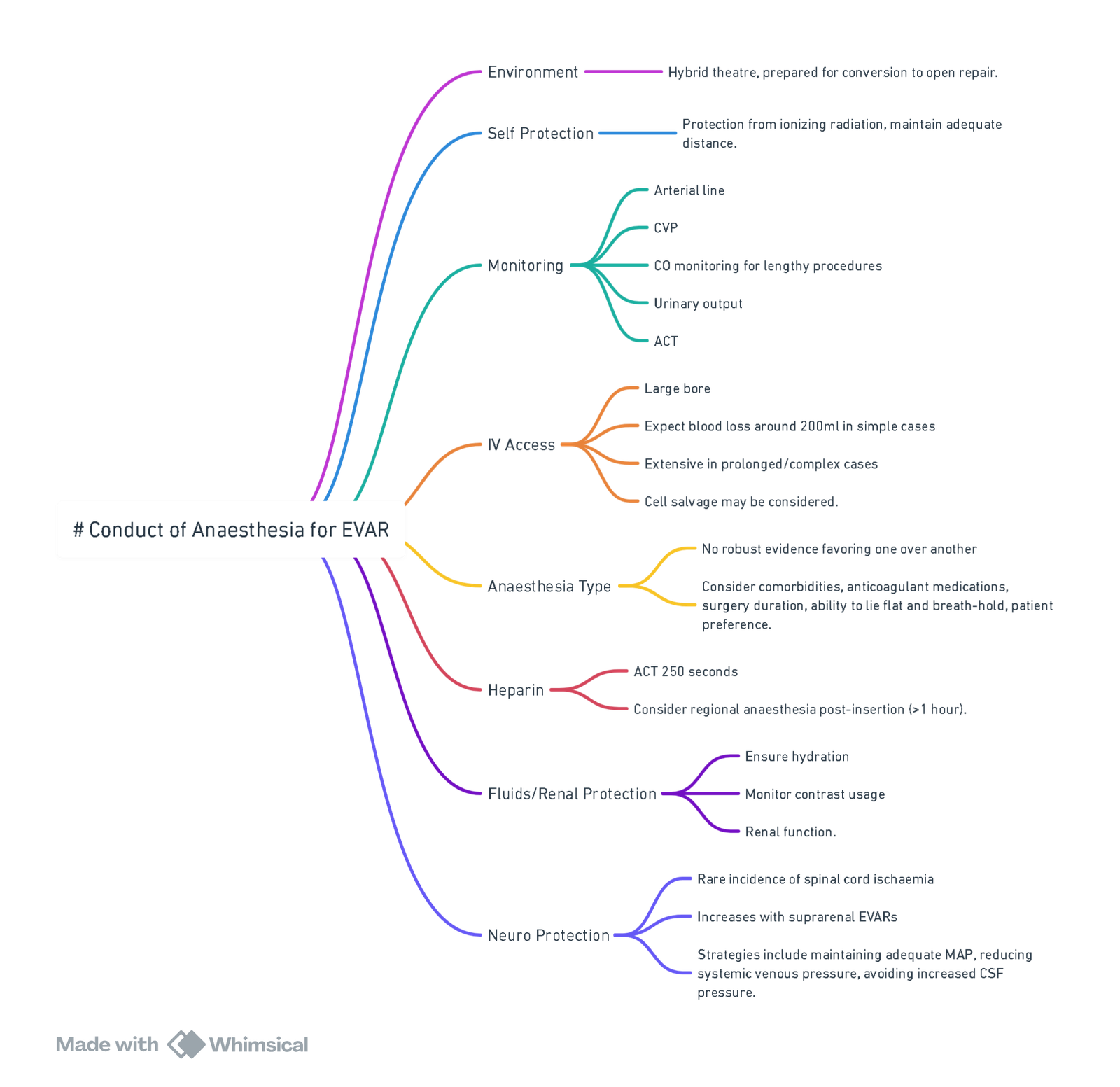
View or edit this diagram in Whimsical.
Pre-op
- Identify high-risk patients for preoperative optimization and devise strategies for perioperative management.
- Multiple comorbidities
- Remote (angio-suite)
Risk Factors
- The risk factors for 30-day mortality with endovascular procedures are
- Renal failure (especially if associated with need for dialysis)
- Age >80 years
- The presence of lower limb ischemia
- Congestive cardiac failure.
- The American College of Cardiology and American Heart Association (ACC/AHA) guidelines regard endovascular procedures as intermediate-risk, but complex endovascular aneurysm repair should be considered high-risk procedures.
Acute Kidney Injury (AKI)
- These patients are at high risk for acute kidney injury postoperatively due to intravenous (IV) contrast and para-renal stents, increasing age, multiple comorbidities, complexity of EVAR, perioperative dehydration, and medications such as ACE inhibitors, aminoglycosides, and diuretics in the perioperative period.
Investigations
- CXR: Usually for smoking history
- ABG: Preoperative ABG helpful in guiding intraoperative ventilator management and predicting postoperative mechanical ventilation.
- Consider Lung FT
- According to the ACC/AHA perioperative guidelines, if the patients have at least two clinical predictors, poor functional capacity, and require revascularization as part of their general management, noninvasive cardiac testing (dobutamine stress echocardiography or myocardial perfusion imaging) is indicated preoperatively.
- Functional capacity assessment is recommended before major vascular surgery. Cardiopulmonary exercise testing is increasingly used to provide an objective assessment of functional status and is useful for risk stratification (using anaerobic threshold and peak oxygen consumption) in predicting adverse outcomes in major vascular surgery.
Optimization
- Perioperative optimization should include a review of the patient’s medications. High-risk patients undergoing major vascular surgery should be on aspirin, beta-blocker, and statin preoperatively.
Intra-op
Location
- Specialized radiology suite (special anesthetic considerations needed for remote-site anesthesia) or hybrid operating theater with appropriate angiography facilities and the ability to convert to an open procedure if required. All necessary precautions should be undertaken to protect theater staff from ionizing radiation with appropriate measures (lead aprons, thyroid shields, and protective screens).
Monitors and IV Access
- Standard monitoring
- Arterial line (enables ABG monitoring and should be inserted contralateral to the upper limb surgical access, usually the right hand)
- Hourly urine output
- Core temperature monitoring
- A 5-lead electrocardiogram should be applied to detect ischemic ST changes.
- Air warming devices and IV fluid warmers
- Large bore venous access due to potential significant blood loss
- Patients are cross-matched the same as for open repair.
- All IV tubings and monitoring cables should be of sufficient length.
- Immediate access to rapid infusion devices
- Central venous access should be considered in complex or long procedures.
- Available close to the theatre: ABC, TEG
- Evoked potentials monitoring is sometimes requested if there is a high risk of spinal cord ischemia (SCI) during the operation.
Goals
(a) To provide hemodynamic stability and preserve perfusion to vital organs including the brain, heart, spinal cord, kidneys, and splanchnic vessels
(b) To avoid imbalance in myocardial oxygen supply and demand
(c) Maintenance of intravascular volume and early identification and management of bleeding
(d) Normothermia
Techniques in Anaesthesia for Endovascular Aneurysm Repair (EVAR)
Considerations
- The choice of anaesthetic technique is determined by the patient and anaesthesiologist, taking into account the vascular team’s experience, the procedure type, aneurysm complexity, and the patient’s premorbid condition.
- Endovascular repair can last between 4 and 12 hours. Patient comfort under regional anaesthesia is difficult due to the necessity of arterial access from axillary, femoral, and occasionally subclavian arteries, making general anaesthesia preferable.
- Although conversion to open repair is rare (<2%), anaesthesiologists must be prepared for open repair and manage massive bleeding.
- Use of an arterial line in the right arm is recommended as the left subclavian artery can be involved or blocked during the procedure.
- Administer heparin to achieve an ACT of 250 seconds.
- Muscle relaxants are required for apnoea to optimize visualization.
- Hypotension is necessary prior to stent deployment, typically managed with remifentanil.
Types of Anaesthesia
- General Anaesthesia (GA), Regional, Local:
- No significant evidence indicates superiority in mortality or morbidity among techniques.
- Considerations include patient’s premorbid states, procedure duration, use of antiplatelets and anticoagulants, and ability to remain supine. The success of EVAR is not dependent on the mode of anaesthesia.
Regional Anaesthesia
- Combined Spinal-Epidural (CSE):
- Provides a fast and dense block with the option for top-ups during prolonged procedures and offers excellent postoperative analgesia.
- Benefits include reduced stress and inflammatory response, avoidance of mechanical ventilation, and effective postoperative analgesia.
General Anaesthesia (GA)
- GA is often more practical due to:
- Preoperative antiplatelet medication use and intraoperative heparinization.
- Easier blood pressure control through titration of anaesthetic agents and vasopressors.
- Secure airway management if aneurysm rupture occurs.
- Facilitation of breath-holding to improve digital subtraction angiography image quality.
- Better tolerance of lengthy procedures involving iliac bifurcated devices, complex fenestrated grafts, or concomitant surgeries.
Heparin Administration
- Administer 5000 IU of IV heparin post-cannulation.
- Check ACT baseline, then 3 minutes after heparin administration, and every 30 minutes thereafter.
- Maintain ACT at 2-2.5 times the baseline (approx. 200-250 seconds). Protamine may be required for reversal post-procedure.
Renal Protection
- Chronic renal impairment prevalence ranges from 3% to 20%.
- Strategies include maintaining adequate hydration, limiting contrast load, and avoiding nephrotoxic drugs (e.g., NSAIDs and aminoglycosides).
Blood Pressure Control
- Hemodynamic instability is minimal unless aortic occlusion balloons are used (typically in ruptured aneurysms).
- Persistent hypertension is managed with beta-blockers like metoprolol or labetalol, with nitrates and/or short-acting beta-blockers for immediate control.
- Hypotension is common post-induction, managed with low-dose vasopressors such as phenylephrine.
Spinal Cord Ischaemia (SCI)
- Incidence: 0.21%
- Risk factors include prolonged procedural time (>150 min), extensive catheter manipulation, and perioperative embolization of hypogastric and lumbar arteries.
- Therapeutic strategies: CSF drainage, hypothermia, steroids, and arterial pressure augmentation.
- Preoperative spinal drains may be inserted for high-risk patients.
- Postoperative spinal drains may be used if neurological issues develop.
- Prevention strategies: adequate MAP (90-110 mmHg post-stent deployment), reduced systemic venous pressure (CVP <10 mmHg), and avoiding increased CSF pressure.
Postoperative Complications of EVAR
| Surgical | Medical |
|---|---|
| Maldeployment or malposition of graft | Acute coronary syndromes |
| Arterial rupture/arterial dissection | Acute congestive cardiac failure |
| Delayed AAA rupture | Acute renal failure/CIN |
| Stent-graft limb thrombosis leading to lower limb ischemia | Arrhythmia |
| Graft migration (uncommon with new stent grafts) | Respiratory infection |
| Endoleak | Venous thromboembolism |
| Rupture of iliac artery (more common in women) | Cerebrovascular accident |
| Ischaemia of: spinal cord, kidneys, liver, bowel, legs | Postimplantation syndrome |
| Graft infection (rare) | |
| Paralysis (rare) |
Postimplantation Syndrome
- Common but usually benign, characterized by pyrexia, leukocytosis, and elevated inflammatory markers.
- Clinically resembles sepsis but without infection evidence.
- Majority of cases are self-limiting, resolving within two weeks.
Types of Endoleaks After EVAR
- Type 1: Leak due to poor graft attachment at proximal or distal end.
- Type 2: Leak into aneurysmal sac from collateral branches (e.g., lumbar or inferior mesenteric arteries).
- Type 3: Leak through graft due to separation or defect.
- Type 4: Leak through graft due to graft material porosity.
- Type 5: Leak of unknown origin but continued expansion of the aneurysmal sac (endotension).
Emergency EVAR
- EVAR is increasingly used for ruptured AAA as the first-line treatment.
- Potential advantages: avoiding general or deep anaesthesia, minimizing damage to abdominal structures, and reducing bleeding from surgical dissection.
- Preparation for possible conversion to open surgery is essential.
- Preoperative management includes fast evaluation, large-bore venous cannula, blood cross-match, and restrictive resuscitation.
- Standardized unit protocols ensure effective decision-making and coordination in emergencies.
- Preoperative CT scan (if stable) helps determine EVAR suitability.
- Procedure involves femoral vessel cannulation and aortic occlusion balloon placement under local anaesthesia.
Links
Past Exam Questions
Anaesthetic Management for Endovascular Aneurysm Repair (EVAR)
List the advantages and disadvantages of local, regional, and general anaesthesia management for endovascular aneurysm repair (EVAR). (10)
EVAR and Anaesthetic Considerations
a) What is his annual risk of rupture and why is this important? (1)
b) List your anaesthetic considerations for an EVAR. (7)
c) Name two risk factors for spinal cord ischaemia and how would you try to prevent it? (2)
References:
- Burdett, E. and Patel, A. (2014). Anaesthesia for endoscopic surgery. Anaesthesia &Amp; Intensive Care Medicine, 15(5), 238-241. https://doi.org/10.1016/j.mpaic.2014.02.004
- Berry, K., Gudgeon, J., & Taylor, J. F. (2022). Anaesthesia for endovascular repair of ruptured abdominal aortic aneurysms. BJA Education, 22(6), 208-215. https://doi.org/10.1016/j.bjae.2022.02.001
Summaries:
EVAR-video
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “74323250-155b-47b7-ade1-4206a1589951”



