- Cardiovascular Disease (CVD) in Pregnancy
- Introduction
- Physiology Recap
- General Principles
- Mode of Delivery and Anaesthesia
- Basic Approach (Must Be Tailored to Each patient)
- Risk Prediction
- Foetal Complications
- Postpartum Period
- Specific Conditions
- Coronary Artery Disease
- Severe LV Dysfunction (e.g., Dilated or Peripartum cardiomyopathy)
- Pulmonary Hypertension
- Unstable Arrhythmia History
- Aortopathy (e.g., Marfan Syndrome)
- Mechanical Prosthetic Valve
- Mitral Stenosis
- Mitral/Aortic Insufficiency
- Aortic Stenosis
- Hypertrophic Obstructive Cardiomyopathy (HOCM) in Pregnancy
- Physiologic Considerations
- Goals
- Anaesthetic Management
- Aortic Dissection
- Presentation
- Congenital Heart Disease (CHD)
- Management Summary
- Links
- Past Exam Questions
{}
Cardiovascular Disease (CVD) in Pregnancy
Introduction
Cardiovascular disease (CVD) is the leading cause of maternal mortality in much of the developed world.
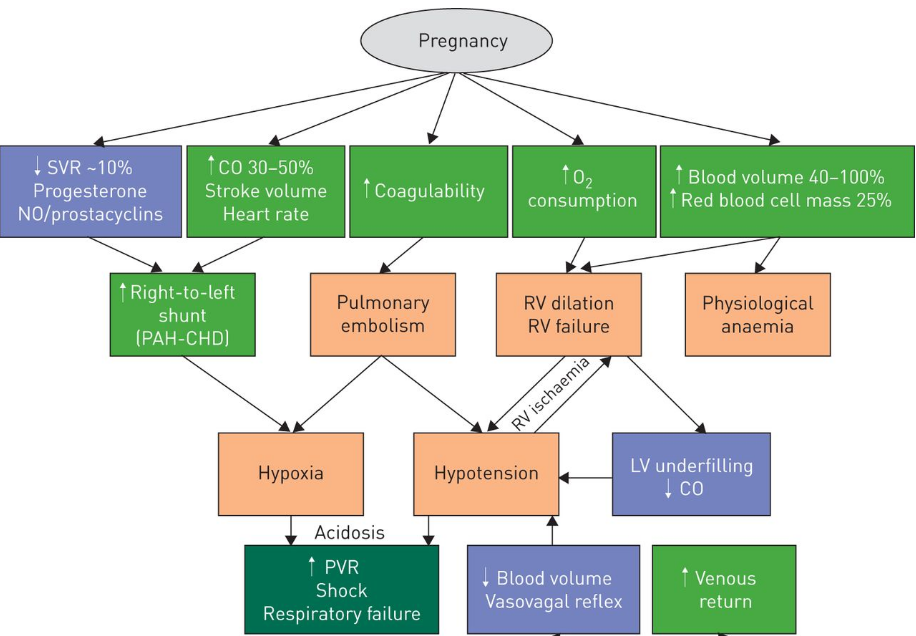
Physiology Recap
| Parameter | Change in Pregnancy |
|---|---|
| SVR | ↓ Early due to progesterone |
| Cardiac Output | ↑ 20% (8 weeks), ↑ 40–50% (20–28 weeks) |
| Stroke Volume | ↑ via increased preload and contractility |
| Heart Rate | ↑ Slightly |
| Labour (Stage 1) | CO ↑ ~15% |
| Labour (Stage 2) | CO ↑ ~50% |
| Post-delivery | CO ↑ 60–80%, normalises in ~1 h |
Clinical Implications for Cardiac Disease
- The severity and type of cardiac disease influences the risk and timing of decompensation
High-Risk Periods
- Early pregnancy:
- Those with limited cardiac reserve may decompensate before 28 weeks, as CO peaks.
- Labour and Delivery:
- Increased risk due to:
- Sympathetic stimulation.
- Repeated auto-transfusion.
- Fluid shifts.
- Increased risk due to:
- Immediate postpartum period:
- Highest risk of pulmonary oedema, especially with:
- Excessive IV fluids (↑ preload)
- Pre-eclampsia (↑ capillary permeability).
- ↓ serum colloid osmotic pressure.
- Highest risk of pulmonary oedema, especially with:
General Principles
- Multidisciplinary approach is essential: includes obstetricians, cardiologists, and anaesthetists.
- Key objectives:
- Optimise maternal condition during pregnancy (e.g., beta-blockers).
- Early recognition and management of complications.
- Minimise cardiovascular load during labour and postpartum.
- NYHA Classification
- NYHA I–II: generally tolerate pregnancy well.
- NYHA III–IV: poor tolerance; require meticulous, individualised anaesthetic planning.
- Anaesthetic goals:
- Provide effective analgesia.
- Effective labor analgesia ensures greater cardiopulmonary and hemodynamic stability.
- Continuous haemodynamic monitoring (e.g., ASA monitors, arterial line, CVP).
- Optimise preload, systemic vascular resistance (SVR), heart rate, contractility, and pulmonary vascular resistance (PVR).
- Tailor anaesthesia based on lesion type and fetal considerations.
- Provide effective analgesia.
Mode of Delivery and Anaesthesia
- Vaginal delivery: preferred for most; lower risk of blood loss, infection, and thromboembolism.
- Segmental epidural analgesia: favoured for labour.
- Early initiation of epidural labor analgesia is recommended.
- Consider intrathecal opioid-only CSE or dural puncture epidural (DPE) techniques.
- Use saline for epidural loss-of-resistance technique to avoid air embolism risk.
- Consider local anesthetic-only test dose for epidural catheter.
- Caesarean Section (CS):
- Neuraxial anaesthesia preferred.
- Segmental epidural superior to intrathecal in high-risk lesions.
- Indications for GA: active thromboembolism, decompensated cardiopulmonary status, thrombocytopenia, neuraxial anaesthesia refusal.
Basic Approach (Must Be Tailored to Each patient)
- Consultant-led care in tertiary centres with HDUs or ICUs and invasive monitoring capabilities.
- Early admission and planning
- Goal: Minimise maternal cardiovascular stress while preserving placental and fetal perfusion
Regional Anaesthesia
- Avoid single-shot spinal due to risk of rapid SVR drop.
- Options:
- Carefully titrated epidural.
- Combined spinal-epidural (CSE).
- Considerations:
- SVR-lowering effects may be hazardous in:
- Left-sided stenotic lesions.
- Patients with shunt physiology.
- Anticoagulation status:
- Evaluate risk of epidural haematoma.
- Consider withholding vs. continuation of anticoagulation.
- Maternal/fetal risk perceptions and preferences
- SVR-lowering effects may be hazardous in:
Combined Spinal-Epidural (CSE) Analgesia for C/S
- Intrathecal Hyperbaric Bupivacaine: 2.5–5 mg.
- Fentanyl: 15–25 μg.
- Followed by 2–3 mL epidural boluses of plain 0.5% bupivacaine or 2% lidocaine over 15-30 minutes.
General Anaesthesia (GA) Cardiac Recipe
- Premedicate with opioids or lidocaine and titrate induction agents slowly.
- Consider remifentanil premedication for caesarean delivery.
- For high-risk cardiac patients, use etomidate induction (0.1–0.3 mg/kg) with remifentanil either as a pre-induction infusion (0.2–0.5 μg/kg/min for 5–10 min) or as a single bolus (2–4 μg/kg).
Monitoring
- Standard plus:
- Arterial line (A-line)
- Transthoracic echocardiography (TTE)
- Cardiac output (CO) monitor
- Pulmonary artery catheter (PAC) for pulmonary hypertension (PHT)
Infective Endocarditis Prophylaxis
- AHA (2007) and NICE (2008) guidelines:
- Do not recommend routine antibiotics for obstetric/gynaecological procedures for endocarditis prevention.
- No evidence of benefit.
Anticoagulation in Pregnancy
Warfarin
- Teratogenic (contraindicated in 1st trimester)
- Crosses placenta (avoid in 3rd trimester)
- Precludes regional anaesthesia
- Difficult to reverse in emergencies
Low Molecular Weight Heparin (LMWH)
- Preferred throughout pregnancy
- Timing for neuraxial procedures:
- Prophylactic LMWH:
- ≥12 h after last dose before neuraxial insertion or catheter removal
- 4 h post-procedure before next dose
- Therapeutic LMWH:
- ≥24 h after last dose before neuraxial insertion or catheter removal
- 4 h post-procedure before next dose
- Prophylactic LMWH:
Uterine Atony
Oxytocics – Use with Caution
| Agent | Considerations |
|---|---|
| Oxytocin | Avoid IV bolus due to ↓SVR, tachycardia, hypotension. Use as infusion: 5U in 20mL over 5–10 min. Continuous infusion (10U/hr) post-delivery may be safer. |
| Ergometrine | Avoid – causes ↑ PVR and hypertension. Contraindicated especially in PHT. |
| Carboprost (PGF₂α) | Avoid – causes bronchospasm, ↑BP, CV collapse, and pulmonary oedema. ↑ PVR |
Mechanical/Surgical Alternatives
- Uterine massage
- Intrauterine balloon tamponade
- Uterine compression sutures (e.g. B-Lynch)
- Internal iliac artery ligation or balloon catheterisation
- Hysterectomy in refractory cases
Supraventricular Tachycardia (SVT) Treatment
- First-line: Vagal maneuvers and adenosine.
- If unsuccessful: Intravenous metoprolol or propranolol.
- If beta blockade fails: Verapamil and/or procainamide.
- Amiodarone is a last resort if SVT is life-threatening.
- For unstable patients: Perform immediate electrical cardioversion.
- Bradyarrhythmias: Temporary external or esophageal pacing is safe.
Risk Prediction
Risk stratification should ideally be done preconceptionally. Various risk scores are used, including CARPREG I, CARPREG II, and ZAHARA, which correlate with major adverse cardiovascular events (MACE).
Predictors of Adverse Events in Pregnant Women with Heart Disease (MACE)
CARPREG II Predictors
- A score of >4 indicates a 41% risk of a cardiovascular event
| Predictor | Points |
|---|---|
| Prior cardiac events or arrhythmias | 3 |
| Baseline NYHA III-IV or cyanosis | 3 |
| Mechanical valve | 3 |
| Ventricular dysfunction | 2 |
| High risk left-sided valve disease/left ventricular outflow tract obstruction | 2 |
| Pulmonary hypertension | 2 |
| Coronary artery disease | 2 |
| High risk aortopathy | 2 |
| No prior cardiac intervention | 1 |
| Late pregnancy assessment | 1 |
- The World Health Organization (WHO) risk stratification model uses cumulative knowledge of lesion-specific risks to divide patients into four risk groups:
- I: Risk no greater than the general population
- II: Small increased risk of maternal death/complications
- III: Significant risk of maternal death/complications; requires expert cardiovascular and obstetric care
- IV: Pregnancy contraindicated due to very high risk
WHO Class 4 Conditions (Counsel Patients Not to Fall Pregnant)
- Mortality rates if pregnant:
- Pulmonary Hypertension (30-60%):
- Continue PDE-5 inhibitors, prostacyclins, calcium channel blockers, and nitric oxide.
- Stop endothelin receptor antagonist (teratogenic).
- Eisenmenger Syndrome
- Ejection Fraction (EF) < 30%:
- Stop ACE inhibitors/ARBs/Spironolactone, can use hydralazine for afterload reduction.
- Beta-blockers (BB) can be used.
- NYHA Class 3-4
- Severe Mitral Stenosis (MS)/Aortic Stenosis (AS):
- Consider balloon valvuloplasty.
- Marfan Syndrome
- Bicuspid Aortic Valve (AV)
- Coarctation of the Aorta
- Previous Peripartum Cardiomyopathy with Residual Symptoms (25%)
- Pulmonary Hypertension (30-60%):
Foetal Complications
- Spontaneous abortions (20%)
- Intrauterine fetal demise
- Preterm birth rate (11%)
- Neonatal events (28%): Small for gestational age (SGA), respiratory distress syndrome (RDS), intraventricular hemorrhage (IVH), and neonatal death
Postpartum Period
- High risk for maternal cardiac complications due to increased preload and “auto-transfusion” from the contracting uterus.
- Elevated preload persists due to extravascular fluid mobilization, with systemic vascular resistance rising over the first few weeks.
- Monitor oxygen saturation (>95%) and investigate any oxygen requirements.
- Use BNP or NT-proBNP to differentiate between normal pregnancy physiology and heart failure.
- Carefully titrate oxytocin to avoid hypotension and other complications.
- For postpartum hemorrhage, use oxytocin infusion and rectal/buccal misoprostol. Avoid carboprost and methylergonovine.
Specific Conditions
Coronary Artery Disease
Physiologic Effects of Pregnancy and Delivery
- Decreased SVR can lead to lesser coronary perfusion to myocardium.
- Increased HR can result in decreased coronary filling time.
- Cardiac work increases significantly during labor, especially painful labor.
Anaesthetic Goals
- Normal heart rate (avoid tachycardia)
- Excellent labor analgesia
- Continue beta blockade through labor and delivery
- Avoid beta agonist agents (e.g., terbutaline)
- Maintain afterload
- Intra-arterial BP monitoring
- Phenylephrine is vasopressor of choice
- Careful titration of neuraxial anaesthetic for labor or CD (Caesarean delivery)
- Phenylephrine infusion for CD
- Titrate oxytocin carefully
- Monitor for and avoid ischemia
- 5-lead ECG monitoring for CD or labor
- Avoid methylergonovine
- Postpartum monitoring
- Monitor for postpartum ischemia or heart failure
Severe LV Dysfunction (e.g., Dilated or Peripartum cardiomyopathy)
Diagnosis
The 2010 position statement of the European Society of Cardiology defines PPCM as an ‘idiopathic cardiomyopathy that causes heart failure secondary to left ventricular (LV) systolic dysfunction and occurs towards the end of pregnancy, or in the months following pregnancy, in the absence of other causes of heart failure
History & Examination
- Symptoms and signs of biventricular failure.
Investigations
- CXR: Cardiomegaly/infiltrates.
- ECG: Sinus tachycardia.
- Echocardiography: Dilated left ventricular (LV) chamber, EF < 45%, increased left ventricular end-diastolic dimension (LVEDD).
- Biopsy: Myocarditis (76% of cases).
Physiologic Effects of Pregnancy and Delivery
- Increased cardiac output and blood volume can result in heart failure/pulmonary edema.
- Decreased oncotic pressure can lead to pulmonary edema.
- ACE inhibitors must be stopped during pregnancy due to teratogenicity.
- Patients with prior peripartum cardiomyopathy are at risk for further LV function deterioration.
Anaesthetic Goals
- Normal heart rate (avoid bradycardia)
- Treat bradycardia with ephedrine or glycopyrrolate
- Maintain afterload (avoid hypertension or hypotension)
- Intra-arterial BP monitoring
- Excellent labor analgesia
- Careful titration of regional anesthetic for labor or CD
- Treat hypotension with ephedrine or norepinephrine
- Titrate oxytocin carefully
- Maintain contractility
- Ephedrine is vasopressor of choice
- If low cardiac output syndrome develops, consider milrinone or dobutamine with epinephrine or norepinephrine
- Maintain normovolemia
- Strict monitoring of fluid balance
- Prevent/Monitor for pulmonary edema
- Careful fluid balance
- Continuous pulse oximetry throughout labor and postpartum
- Manage pulmonary edema
- Consider diuresis
- Administer supplemental oxygen
- If necessary, consider intubation with PEEP and controlled ventilation
- Manage AICD if present
- Keep anti-tachyarrhythmia function active in labor
- Prepare to suspend this function for emergent CD
- Minimize pulmonary vascular resistance
- Supplemental oxygen throughout labor and delivery
- Avoid over-sedation
- Assure well-controlled ventilation if intubated
- Avoid carboprost
- Postpartum monitoring
- Monitor for postpartum heart failure
Pulmonary Hypertension
Introduction
- High mortality risk (5–25%); pregnancy often contraindicated.
- Symptoms from RV hypertrophy, low CO.
Physiologic Effects of Pregnancy and Delivery
- Increased cardiac output may not be accommodated by fixed pulmonary vasculature, risking right heart failure and death.
- Decreased SVR can decrease coronary filling to a dilating and failing right ventricle.
- Hypercoagulable state can result in pulmonary emboli, which are lethal in patients with pulmonary hypertension.
Anaesthetic Goals
- Minimize pulmonary vascular resistance
- Supplemental oxygen throughout labor and delivery
- Avoid over-sedation
- Assure well-controlled ventilation if intubated
- Avoid carboprost
- Avoid hypercarbia, acidosis, stress, hypoxia and excessive PEEP
- Maintain adequate blood volume and venous return
- Strict monitoring of fluid balance
- Avoid myocardial depressants
- Avoid beta blockade if possible
- 5-lead ECG monitoring for CD or labor
- Maintain afterload
- Intra-arterial BP monitoring
- Careful titration of neuraxial anaesthetic for labor or CD
- Phenylephrine is vasopressor of choice
- Titrate oxytocin carefully
- Invasive pulmonary artery catheter monitoring and vasoactive agents
- Consider partnership with cardiovascular anaesthesiologist
- Postpartum monitoring
- Monitor for postpartum right heart failure
Physiological Changes Influence on PHT
Unstable Arrhythmia History
Physiologic Effects of Pregnancy and Delivery
- Pregnancy, labor, and delivery can trigger tachyarrhythmias.
Anaesthetic Goals
- Identify arrhythmias early
- 5-lead ECG monitoring during CD or vaginal delivery and postpartum
- Qualified nursing staff for cardiac telemetry
- Cardiovert unstable arrhythmias rapidly
- Cardioversion is safe in pregnancy
- Consider fetal distress indication for cardioversion
- Manage pacemaker/AICD if present
- Keep anti-tachyarrhythmia function active in labor
- Prepare to suspend function and initiate VOO mode for emergent CD
- Postpartum monitoring
- Monitor for postpartum arrhythmia
Aortopathy (e.g., Marfan Syndrome)
Physiologic Effects of Pregnancy and Delivery
- Pregnancy, labor, and delivery may increase dilation of the aortic root and increase risk of aortic rupture in women with Marfan syndrome
Anaesthetic Goals
- Minimize aortic wall tension
- Excellent labor analgesia
- Continue beta blockade through labor and delivery
- CD or no Valsalva during second stage labor
- Minimize hemodynamic swings
- Careful titration of neuraxial anesthetic for labor or CD
- Intra-arterial BP monitoring
- Avoid methylergonovine and carboprost
- Titrate oxytocin carefully
- Postpartum monitoring
- Monitor for postpartum hemodynamic instability
Mechanical Prosthetic Valve
Physiologic Effects of Pregnancy and Delivery
- Hypercoagulable state increases risk of valve thrombosis.
- Vitamin K antagonists are teratogenic and often result in suboptimal anticoagulation during pregnancy.
Anesthetic Goals
- Balance anticoagulation therapy and anesthesia technique
- Perform general anesthesia for CD in anticoagulated patients
- Recognize increased risk of intrapartum and postpartum hemorrhage
- Select/titrate uterotonics carefully, recognizing oxytocin decreases SVR, methylergonovine behaves as an adrenergic agonist, and carboprost significantly increases pulmonary vascular resistance
- Postpartum monitoring
- Monitor for postpartum valvular clotting or obstetric bleeding
Mitral Stenosis
Introduction
- Aetiology: predominantly post-RHD (90%)
- Symptoms: exertional dyspnoea, orthopnoea, pulmonary oedema.
- Signs: mid-diastolic murmur, enlarged LA, atrial fibrillation (AF).
Medical Management
- Beta-blockers and heparin (for AF prophylaxis).
- Avoid fluid overload, anaemia, and sepsis.
- Severe stenosis (<1.0 cm²): may require percutaneous balloon valvotomy.
Physiologic Effects of Pregnancy and Delivery
- Fixed preload to LV may lead to increased cardiac output and pulmonary edema.
- Decreased oncotic pressure further increases risk of pulmonary edema.
- Increased blood volume and HR during pregnancy may lead to atrial fibrillation and pulmonary edema.
Anaesthetic Goals
- Normal heart rate (avoid tachycardia)
- Excellent labor analgesia
- Continue beta blockade through labor and delivery
- 5-lead ECG monitoring for CD or labor
- Avoid beta agonist agents (e.g., terbutaline)
- Avoid atrial fibrillation
- Consider cardioversion in new atrial fibrillation
- Decrease rapid ventricular rate in chronic atrial fibrillation
- Maintain normovolemia
- Strict monitoring of fluid balance
- Prevent/Monitor for pulmonary edema
- Careful fluid balance
- Continuous pulse oximetry throughout labor and postpartum
- Manage pulmonary edema
- Consider diuresis
- Administer supplemental oxygen
- If necessary, consider intubation with PEEP and controlled ventilation
- Postpartum monitoring
- Monitor for postpartum pulmonary edema
Labour and Delivery
- Labour analgesia: segmental lumbar epidural (slow titration).
- Caesarean section:
- Epidural preferred over spinal (better haemodynamic control).
- GA with high-dose opioids and short-acting agents may be used; avoid sympathetic stimulation.
Mitral/Aortic Insufficiency
Physiologic Effects of Pregnancy and Delivery
- Decreased SVR results in lesser regurgitant volume.
- Pregnancy can worsen ventricular dilation.
Anesthetic Goals
- Avoid increases in SVR and decreases in contractility
- Excellent labor analgesia
- Avoid bradycardia
- Careful titration of vasopressors (e.g., phenylephrine) with spinal for CD
- Maintain sinus rhythm
- Excellent labor analgesia
- Consider afterload reduction
- Neuraxial analgesia/anesthesia typically well tolerated if ventricular function is preserved
Aortic Stenosis
Introduction
- Causes: RHD, bicuspid valve, infective endocarditis.
- Symptoms: angina, syncope, heart failure.
- Management: beta-blockers, diuretics; valvuloplasty or valve replacement in severe cases.
Physiologic Effects of Pregnancy and Delivery
- Decreased SVR can lead to lesser coronary perfusion pressure to thickened LV myocardium.
- LV diastolic dysfunction can lead to pulmonary edema.
Anaesthetic Goals
- Maintain afterload (avoid hypotension)
- Intra-arterial BP monitoring
- Careful titration of neuraxial anesthetic for labor or CD
- Treat hypotension with phenylephrine
- Avoid beta agonist agents (e.g., terbutaline)
- Titrate oxytocin carefully
- Normal heart rate (avoid tachycardia)
- Excellent labor analgesia
- Monitor for ischemia
- 5-lead ECG monitoring for CD or labor
- Maintain normovolemia
- Strict monitoring of fluid balance
- Postpartum monitoring
- Monitor for postpartum hypotension or ischemia
Labour and Delivery
- Neuraxial analgesia controversial; can be used in low concentrations.
- CS may be necessary; epidural or GA acceptable with careful monitoring.
Hypertrophic Obstructive Cardiomyopathy (HOCM) in Pregnancy
Physiologic Considerations
- HOCM: Depends on a well-filled LV to maintain output and decrease dynamic obstruction.
- Pregnancy Exacerbations: Increased HR, increased contractility, decreased SVR, aortocaval compression.
- Management:
- Chronic beta-blockade should be continued throughout pregnancy.
- Prefer vaginal delivery (NVD) to tolerate the second stage well due to increase in SVR.
- Use ergometrine over oxytocin for uterotonic management.
Goals
- Maintain intravascular volume and venous return:
- Avoid aortocaval compression.
- Maintain SVR.
- Slow HR, maintaining sinus rhythm.
- Aggressive treatment of tachyarrhythmias.
- Prevent increases in myocardial contractility.
Anaesthetic Management
- Avoid single-shot spinal.
- Invasive haemodynamic monitoring.
- Gradual Epidural and Combined Spinal-Epidural:
- Slow graded epidural and combined spinal epidural with intrathecal opioid have been used safely.
- Labour Analgesia:
- Epidural analgesia attenuates catecholamine release, reducing increases in heart rate and contractility.
- Vasopressor Choice:
- Phenylephrine is the preferred vasopressor.
- Ephedrine should be avoided due to potential increases in myocardial contractility.
- Postpartum Management:
- Postpartum diuresis poses a risk for worsening of outflow tract obstruction.
Aortic Dissection
Presentation
Asymptomatic
- Typical or atypical chest pain
Examination
- Signs of acute left ventricular failure (usually due to aortic regurgitation secondary to aortic root dilatation)
- Signs of end organ damage depending on the level of the dissection
Investigation
- Chest X-ray (CXR): Widened mediastinum
- Electrocardiogram (ECG):
- Sinus tachycardia
- Arrhythmia
- T wave inversion
- ST segment depression
- New left bundle branch block (LBBB)
- Ectopic beats
- Echocardiography (Echo):
- Dissection
- Aortic root dilatation
- Aortic regurgitation
- Computed Tomography (CT): Dissection
Anaesthetic Goals
- Minimize aortic wall tension
- Excellent labor analgesia
- Continue beta blockade through labor and delivery
- CD or no Valsalva during second stage labor
- Minimize hemodynamic swings
- Careful titration of neuraxial anesthetic for labor or CD
- Intra-arterial BP monitoring
- Avoid methylergonovine and carboprost
- Titrate oxytocin carefully
- Postpartum monitoring
- Monitor for postpartum hemodynamic instability
Congenital Heart Disease (CHD)
Acyanotic Lesions
- Common: ASD, VSD, PDA.
- Generally well-tolerated if no pulmonary hypertension.
- Risks: fluid overload → LV failure, arrhythmias.
Anaesthetic goals:
- Prevent air embolism.
- Avoid decrease in SVR (esp. with PHT).
- Avoid increases in PVR: Prevent hypoxia, hypercarbia, acidosis.
- Segmental epidural preferred.
- GA acceptable if SVR increase is controlled.
Cyanotic Lesions
Tetralogy of Fallot (TOF)
- Features: VSD, RVOT obstruction, overriding aorta, RV hypertrophy.
- Symptoms: cyanosis, polycythaemia, fatigue.
Anaesthetic goals:
- Avoid drop in SVR and venous return.
- Maintain haemodynamic stability.
- Labour: systemic opioids preferred.
- CS: GA with ketamine often indicated; avoid neuraxial if haemodynamically unstable.
Eisenmenger Syndrome
- Occurs when PHT develops over a left-to-right shunt.
- Symptoms: hypoxaemia, cyanosis, right-to-left shunt.
Anaesthetic goals:
- Balance SVR and PVR.
- Avoid significant SVR drop.
- Segmental epidural safe with careful titration.
- GA reserved for emergencies.
Management Summary
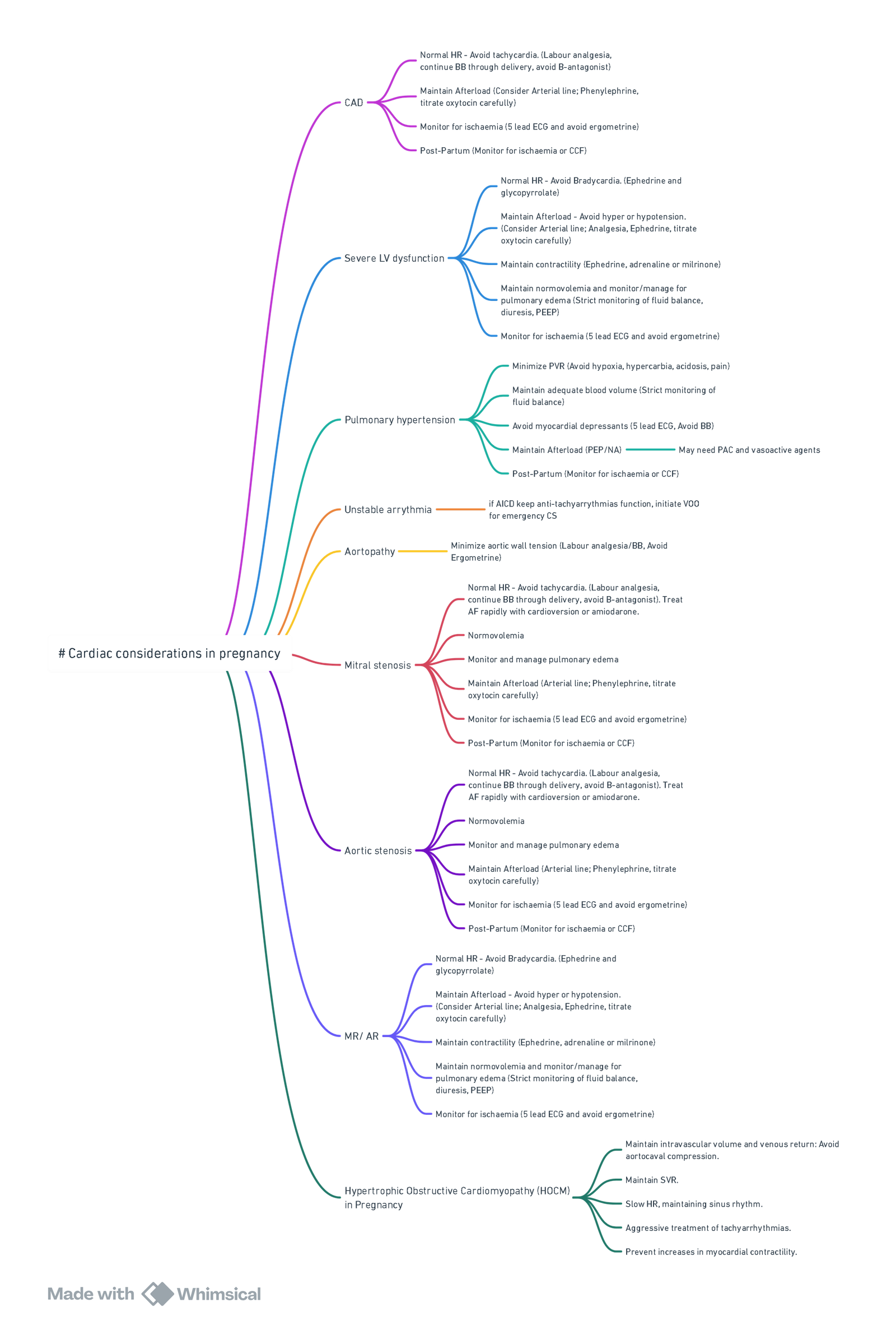
View or edit this diagram in Whimsical.
| Condition | Heart Rate | Preload | Contractility | Afterload | Pulmonary Vascular Resistance (PVR) | Inotrope/Vasopressor of Choice | Oxytocics to Avoid | Additional Notes |
|---|---|---|---|---|---|---|---|---|
| Coronary Artery Disease | Normal (avoid tachycardia) | Maintain normovolemia | Maintain | Increase | Avoid increase | Phenylephrine | Methylergonovine, Terbutaline (B2 agonist) | Continue beta-blockers, careful ECG & ischemia monitoring |
| Severe LV Dysfunction | Normal (avoid bradycardia) | Maintain normovolemia (strict). Avoid fluid overload | Maintain | Maintain (avoid swings) | Minimize | Ephedrine; consider Milrinone with adrenaline | Carboprost | Avoid pulmonary edema, manage ICD |
| Pulmonary Hypertension | Normal | Maintain adequate normovolemia | Maintain | Maintain to increase | Aggressively minimize | Phenylephrine | Carboprost | Avoid hypercarbia, acidosis, stress, hypoxia and high PEEP |
| Unstable Arrhythmia History | Avoid extremes | Maintain normovolemia | Maintain | Maintain | Normal | Based on arrhythmia type (Rapid cardioversion in unastable) | – | Rapid cardioversion safe; manage pacemaker/ICD |
| Aortopathy (Marfan Syndrome) | Avoid tachycardia | Maintain normovolemia | Maintain, avoid increase | Maintain | Normal | Phenylephrine | Methylergonovine, Carboprost, Terbutaline (B2 agonist) | Minimize aortic wall tension, avoid Valsalva |
| Mechanical Prosthetic Valve | Normal | Maintain normovolemia | Maintain | Maintain | Avoid significant increase | Phenylephrine | – | Balance anticoagulation; general anesthesia if anticoagulated |
| Mitral Stenosis | Normal (avoid tachycardia) | Maintain normovolemia (strict) | Maintain | Maintain, to increased | Normal | Phenylephrine | Terbutaline | Prevent atrial fibrillation & pulmonary edema |
| Mitral/Aortic Insufficiency | Normal (avoid bradycardia) | Maintain normovolemia | Maintain | Decrease SVR | Normal | Ephidrine | – | Good ventricular function necessary; afterload reduction |
| Aortic Stenosis | Normal (avoid tachycardia) | Maintain normovolemia | Maintain | Maintain to increased | Normal | Phenylephrine | Terbutaline | Controversial neuraxial analgesia; ischemia monitoring |
| HOCM | Slow, sinus rhythm | Maintain normovolemia (strict) | Avoid increases | Maintain (critical) to increased | Normal | Phenylephrine | Avoid Oxytocin (prefer Ergometrine), Terbutaline | Aggressively manage tachyarrhythmias, avoid single-shot spinal |
| Aortic Dissection | Normal (avoid tachycardia) | Maintain normovolemia | Maintain, avoid increase | Maintain | Normal | Phenylephrine | Methylergonovine, Carboprost | Minimize aortic wall tension, intra-arterial monitoring |
| Congenital Heart Disease (Acyanotic) | Normal | Maintain normovolemia | Maintain | Maintain to increase | Decrease | Phenylephrine (careful titration) | – | Avoid air embolism, maintain SVR, segmental epidural |
| TOF (Cyanotic) | Normal | Maintain normovolemia | Maintain | Maintain | Avoid significant increase | Phenylephrine | – | Avoid neuraxial if unstable, systemic opioids preferred |
| Eisenmenger Syndrome | Normal | Maintain normovolemia (critical) | Maintain | Balance carefully (avoid drop) | Aggressively minimize | Phenylephrine | – | Segmental epidural with caution, avoid SVR drop |
Links
- Cardiac physiology
- Anaesthetic management of specific cardiac conditions
- Valvular heart disease
- Rheumatic heart disease
- Cardiomyopathy
- Obstetric emergencies
Past Exam Questions
Anaesthesia for a Parturient with PDA
a) Name 4 cardiovascular changes during normal pregnancy at term relevant to this patient. (4)
b) What monitoring is needed above standard monitoring? (2)
c) Briefly explain the main reasoning behind your chosen anaesthesia technique. (4)
References:
- The pregnant cardiac patient and anaesthesia AV Nkuna. Wist refresher 2022
- Hussey H, Hussey P, Meng ML. Peripartum considerations for women with cardiac disease. Curr Opin Anaesthesiol. 2021;34(3):218-25. https://doi. org/10.1097/ACO.0000000000000992.
- Meng ML, Arendt KW. Obstetric anesthesia and heart disease: practical clinical considerations. Anesthesiology. 2021;135(1):164-83. https://doi.org/10.1097/ ALN.0000000000003833.
- Kuczkowski KM, van Zundert A. Anesthesia for pregnant women with valvular heart disease: the state-of-the-art. J Anesth. 2007;21(2):252-7. https://doi. org/10.1007/s00540-007-0504-3.
- Bhatia P, Chhabra S. Physiological and anatomical changes of pregnancy: Implications for anaesthesia. Indian J Anaesth. 2018;62(9):651-7. https://doi. org/10.4103/ija.IJA_458_18.
- Burt, C. and Durbridge, J. (2009). Management of cardiac disease in pregnancy. Continuing Education in Anaesthesia Critical Care &Amp; Pain, 9(2), 44-47. https://doi.org/10.1093/bjaceaccp/mkp005
- Arendt, K. W. and Lindley, K. J. (2019). Obstetric anesthesia management of the patient with cardiac disease. International Journal of Obstetric Anesthesia, 37, 73-85. https://doi.org/10.1016/j.ijoa.2018.09.011
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries
Obstetric cardiac disease
Heart disease in pregnancy videos
—
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “c4590df8-b1dc-43d7-9546-1539089e5762”



