- Approach to Interpretation
- General
- Conditions
- Pacemaker and ICD
{}
Approach to Interpretation
Confirm Details
Begin chest X-ray interpretation by checking the following details:
- Patient details: Name, date of birth, and unique identification number.
- Date and time: When the film was taken.
- Previous imaging: Useful for comparison.
Assess Image Quality
Next, assess the quality of the image using the mnemonic RIPE.
Rotation
- The medial aspect of each clavicle should be equidistant from the spinous processes.
- The spinous processes should be vertically oriented against the vertebral bodies.
Inspiration
- The 5-6 anterior ribs, lung apices, both costophrenic angles, and the lateral rib edges should be visible.
Projection
- Note if the film is AP or PA. If there is no label, assume it is a PA film (if the scapulae are not projected within the chest, it is PA).
Exposure
- The left hemidiaphragm should be visible to the spine, and the vertebrae should be visible behind the heart.
ABCDE Approach
The ABCDE approach can be used for a structured interpretation of a chest X-ray:
- Airway: Trachea, carina, bronchi, and hilar structures.
- Breathing: Lungs and pleura.
- Cardiac: Heart size and borders.
- Diaphragm: Including assessment of costophrenic angles.
- Everything else: Mediastinal contours, bones, soft tissues, tubes, valves, pacemakers, and review areas.
Airway
Trachea
Inspect the trachea for evidence of deviation:
- The trachea is normally located centrally or deviating very slightly to the right.
- If the trachea appears significantly deviated, inspect for anything that could be pushing or pulling the trachea. Check for paratracheal masses and/or lymphadenopathy.
Causes of True and Apparent Tracheal Deviation
True Tracheal Deviation:
- Pushing of the trachea: Large pleural effusion or tension pneumothorax.
- Pulling of the trachea: Consolidation with associated lobar collapse.
Apparent Tracheal Deviation:
- Rotation of the patient can give the appearance of apparent tracheal deviation. Inspect the clavicles to rule out the presence of rotation.
Carina and Bronchi
- The carina is cartilage situated at the point at which the trachea divides into the left and right main bronchus.
- On an appropriately exposed chest X-ray, this division should be clearly visible.
- The carina is an important landmark when assessing nasogastric (NG) tube placement, as the NG tube should bisect the carina if it is correctly placed in the gastrointestinal tract.
- The right main bronchus is generally wider, shorter, and more vertical than the left main bronchus. Consequently, inhaled foreign objects are more likely to become lodged in the right main bronchus.
- Depending on the quality of the chest X-ray, you may be able to see the main bronchi branching into further subdivisions.
Hilar Structures
- The hilar consist of the main pulmonary vasculature and the major bronchi.
- Each hilar also contains a collection of lymph nodes, which are not usually visible in healthy individuals.
- The left hilum is often positioned slightly higher than the right, but there is wide variability between individuals.
- The hilar are usually the same size, so asymmetry should raise suspicion of pathology.
- The hilar point is an important landmark where the descending pulmonary artery intersects the superior pulmonary vein. Loss of this point may suggest a lesion (e.g., lung tumour or enlarged lymph nodes).
Causes of Hilar Enlargement or Abnormal Position
Hilar Enlargement:
- Bilateral symmetrical enlargement is typically associated with sarcoidosis.
- Unilateral/asymmetrical enlargement may be due to underlying malignancy.
Abnormal Hilar Position:
- Pushed hilar: May be caused by an enlarging soft tissue mass.
- Pulled hilar: May be due to lobar collapse.
Breathing
Lungs
Inspect the lungs for abnormalities:
- Divide each lung into three zones, each occupying one-third of the height of the lung. These zones do not equate to lung lobes (e.g., the left lung has three zones but only two lobes).
- Ensure that lung markings are present throughout each zone.
- Compare each zone between lungs, noting any asymmetry (some asymmetry is normal due to anatomical structures such as the heart).
- Symmetrical changes in lung fields can be difficult to recognize; keep this in mind for pathologies like pulmonary oedema.
- Increased airspace shadowing in a specific lung area may indicate pathology (e.g., consolidation or malignant lesion).
- The complete absence of lung markings should raise suspicion of a pneumothorax.
Pleura
- In healthy individuals, the pleura are not usually visible. Visibility indicates pleural thickening, often associated with mesothelioma.
- Ensure lung markings extend to the lung field edges; absence suggests pneumothorax.
- Fluid (hydrothorax) or blood (haemothorax) in the pleural space results in increased opacity on a chest X-ray. Air and fluid combination (hydropneumothorax) shows mixed opacity patterns.
Tension Pneumothorax
A tension pneumothorax is life-threatening, involving trapped air within the pleural cavity, displacing mediastinal structures (e.g., the trachea) and impairing cardiac function. Immediate intervention is required without waiting for imaging if suspected clinically (shortness of breath and tracheal deviation).
Cardiac
Assess Heart Size
- In a healthy individual, the heart should occupy no more than 50% of the thoracic width (cardiothoracic ratio <0.5). This rule applies to PA chest X-rays only, as AP films exaggerate heart size.
- Cardiomegaly is present if the heart occupies more than 50% of the thoracic width on a PA chest X-ray. Causes include valvular heart disease, cardiomyopathy, pulmonary hypertension, and pericardial effusion.
Assess the Heart’s Borders
- The right atrium forms most of the right heart border.
- The left ventricle forms most of the left heart border.
- Pathology increasing the opacity of overlying lung tissue may obscure heart borders:
- Reduced right heart border definition typically indicates right middle lobe consolidation.
- Reduced left heart border definition typically indicates lingular consolidation.
Diaphragm
- The right hemidiaphragm is usually higher than the left due to the liver. The stomach underlies the left hemidiaphragm, identified by the gastric bubble.
- The diaphragm should be indistinguishable from the underlying liver in healthy individuals. Free gas, often from bowel perforation, separates and lifts the diaphragm, indicating urgent review.
- Pseudo-pneumoperitoneum conditions, like Chilaiditi syndrome, cause the false impression of free gas under the diaphragm, due to abnormal colon positioning. Always discuss suspected free gas with a senior colleague immediately.
Costophrenic Angles
- The costophrenic angles are formed by the dome of each hemidiaphragm and the lateral chest wall.
- In a healthy individual, these angles should be clearly visible as a well-defined acute angle.
- Loss of this acute angle (costophrenic blunting) can indicate fluid or consolidation. Lung hyperinflation from diaphragmatic flattening can also cause blunting (e.g., COPD).
Everything Else
Mediastinal Contours
The mediastinum contains the heart, great vessels, lymphoid tissue, and potential spaces for pathology. Assess important structures:
Aortic Knuckle
- The aortic knuckle is at the left lateral edge of the aorta as it arches over the left main bronchus. Reduced definition may indicate an aneurysm.
Aortopulmonary Window
- The aortopulmonary window is between the arch of the aorta and the pulmonary arteries. Loss of this space can indicate mediastinal lymphadenopathy (e.g., malignancy).
Bones
Inspect the visible skeletal structures for abnormalities (e.g., fractures, lytic lesions).
Soft Tissues
Inspect the soft tissues for abnormalities (e.g., large haematoma).
Tubes, Valves, and Pacemakers
Tubes
- Assess nasogastric tube placement for safe feeding. Refer to guides for detailed placement assessment.
- Various tubes and cables will be visible as radio-opaque lines (e.g., central line, ECG cables).
Artificial Heart Valves
- Artificial heart valves appear as ring-shaped structures within the heart region (e.g., aortic valve replacement).
Pacemaker
- Pacemakers appear as a radio-opaque disc or oval in the infraclavicular region, connected to pacemaker wires positioned within the heart.
General
Pre Op Indication
- New / unstable cardiopulmonary symptoms
- Patients at risk of ↑ POPC, only if it will change management
Structures
AP
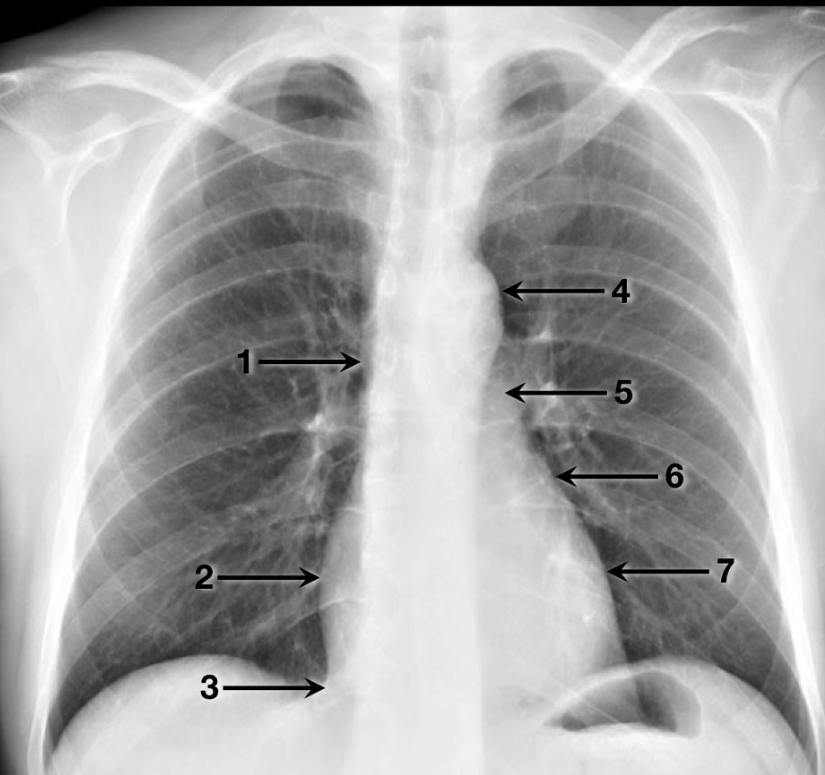
- Superior vena cava
- Right atrium
- Inferior vena cava
- Aortic arch
- Main pulmonary artery
- Left atrial appendage
- Left ventricle
Lateral
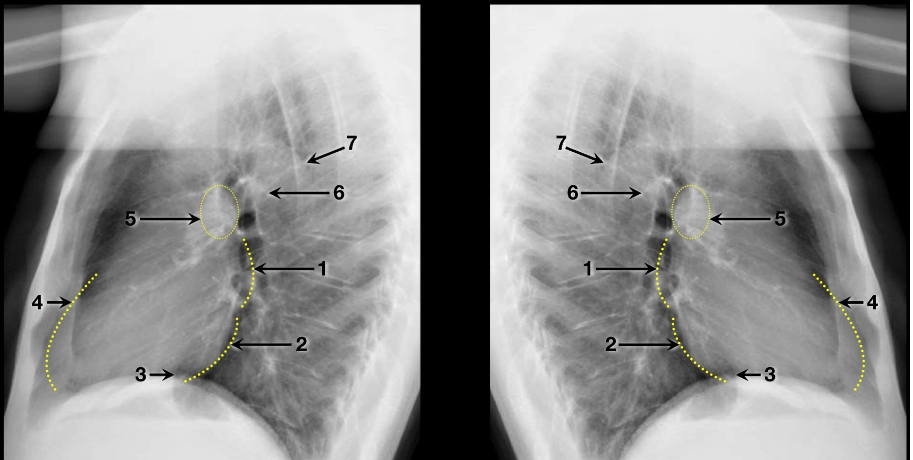
- Left atrium
- Left ventricle
- Inferior vena cava
- Right ventricle
- Right pulmonary artery
- Left pulmonary artery
- Aorta
Lung Lobe Orientation
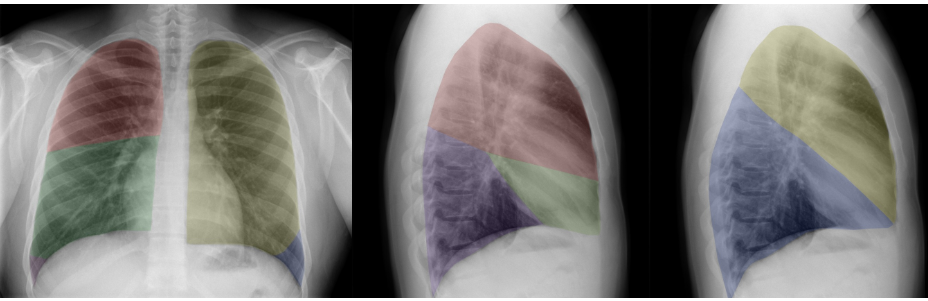
Red: Right upper lobe (RUL)
Green: Right middle lobe (RML)
Purple: Right lower lobe (RLL)
Yellow: Left upper lobe (LUL)
Blue: Left lower lobe (LLL)
Conditions
Mediastinal Mass
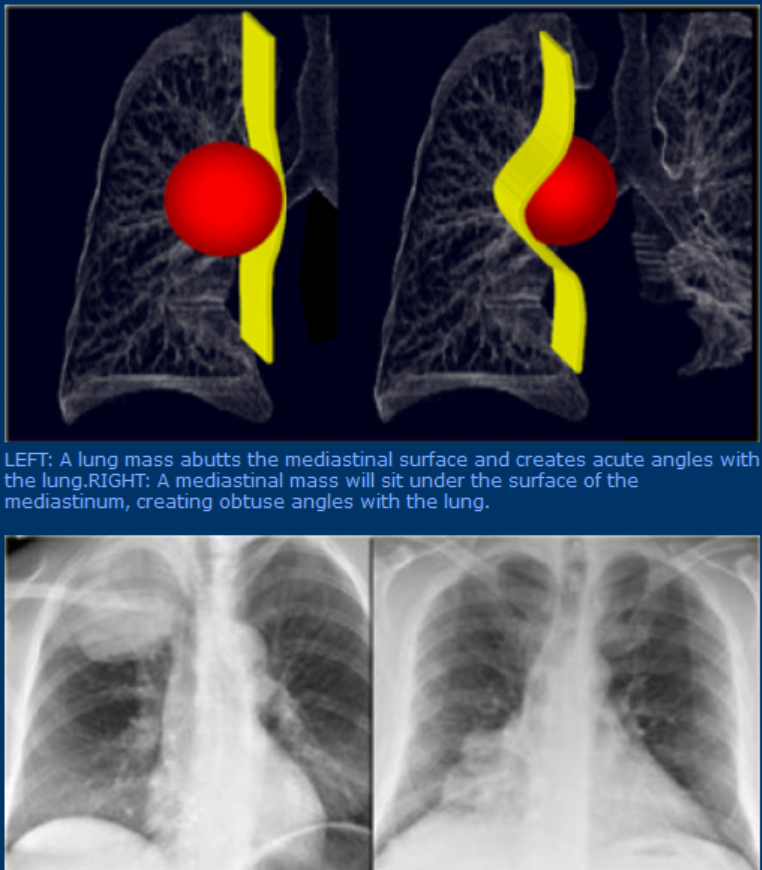
Features
- Unlike lung lesions, a mediastinal mass will not contain air bronchograms.
- The margins with the lung will be obtuse.
- Mediastinal lines (azygoesophageal recess, anterior and posterior junction lines) will be disrupted.
- There can be associated spinal, costal or sternal abnormalities.
Pneumothorax
Classification
Pediatric Pneumothorax
- Neonates with Respiratory Distress Syndrome:
- Increased risk if mechanically ventilated with positive end-expiratory pressure.
- Congenital Diaphragmatic Hernia:
- Underdeveloped lung ipsilateral to the diaphragm defect.
- Contralateral lung prone to barotrauma and pneumothorax due to increased compliance.
Spontaneous Pneumothorax
- Primary Spontaneous Pneumothorax:
- Occurs without trauma.
- Most common in males aged 20–40, often tall and slender, frequently smokers.
- High recurrence rate within the first year after the initial event.
- Secondary Spontaneous Pneumothorax:
- Occurs in patients with underlying pulmonary disease.
- More serious presentation with symptoms and sequelae due to comorbid conditions.
Traumatic Pneumothorax
- Caused by blunt or penetrating trauma to the chest wall.
- Iatrogenic Pneumothorax:
- Most commonly caused by subclavian line placement.
- Tension Pneumothorax:
- Air enters the pleural cavity during inspiration but cannot exit, enlarging the pleural space.
- Leads to mediastinal and tracheal shift to the contralateral side and decreased venous return.
- Medical emergency requiring prompt intervention to prevent rapid deterioration and death.
Clinical Presentation
- Sudden, severe pleuritic chest pain, dyspnea, and cough.
- Hyperresonant hemithorax to percussion with tracheal shift away from the affected side.
- Possible neck vein distension.
- Diminished or absent breath sounds.
- Increased airway pressure, decreased pulmonary compliance, cyanosis, and hypotension intraoperatively.
- Blood gases may show hypoxia and hypercarbia in severe cases.
Management
- Chest Tube:
- Indicated when a large amount of lung is collapsed.
- Spontaneous Pneumothorax:
- Typically absorbed if the collapsed lung is less than 20%.
- Supplemental oxygen can accelerate resorption.
- Surgical Intervention:
- Indicated if air leak persists for more than 10 days.
- Recurrent pneumothorax can be treated with chemical pleurodesis, instilling tetracycline into the pleural space without thoracotomy.
Unilateral Lung Whiteout

Differential Diagnosis
- Pneumonia
- Pleural Effusion (including hemothorax)
- Collapse/Atelectasis
Important Diagnostic Indicator
- Tracheal Deviation or Mediastinal Shift
Differential Diagnosis Based on Mediastinal/Tracheal Position
Central Mediastinum
- Conditions: Consolidation/pneumonia, pulmonary edema/ARDS, small to moderate pleural effusions, mesothelioma.
- Characteristics:
- Small and moderate pleural effusions gravitate posteriorly without producing mediastinal shift.
- Mesothelioma causes lung encasement, limiting mediastinal shift.
Tracheal Displacement Away from Opacity
- Conditions: Moderate to large pleural effusion, large pulmonary mass, diaphragmatic hernia.
- Characteristics:
- Diaphragmatic hernias: Right side usually involves liver herniation, left side involves herniated bowel.
Mediastinal Shift Toward the Side of Opacity
- Conditions: Lung collapse (endobronchial intubation, mucus plugging), post-pneumonectomy, pulmonary agenesis/hypoplasia.
Pacemaker and ICD
Pacemaker
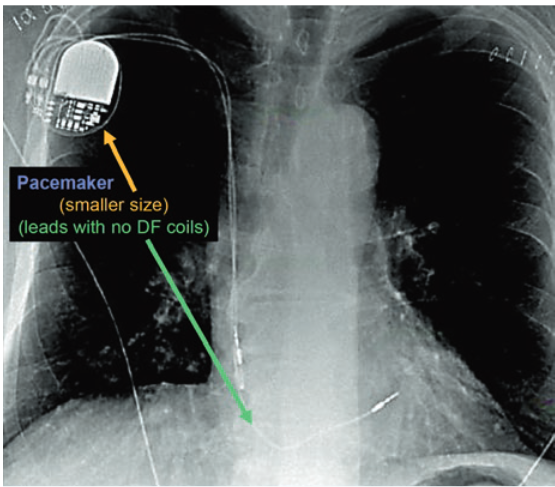
Radiographic Identification
- Smaller generator
- Discreet right ventricular lead: Stable diameter.
- Additional leads: With or without right atrial lead or coronary sinus lead.
Indications
- Symptomatic sinus node dysfunction and bradycardia
- Complete AV block: Symptoms are less relevant.
- Hypersensitive carotid sinus syndrome and neurocardiogenic syncope
Effect of Magnet
- Suspend sensing of intrinsic rhythm
- Asynchronous pacing: The rate depends on the manufacturer and battery life. If the battery life is low, the rate may not be adequate for surgery.
- Turns off “rate response”
Other Effects
- Electrocautery:
- Faulty sensing of intrinsic activity causing inappropriate inhibition of pacemaker activity, more prominent with monopolar cautery, and more likely with surgery above the waist.
- Possible device reset or damage to the generator or leads, though this is unlikely.
- Radiation therapy:
- Possible device reset when performed near the device.
- Radiofrequency:
- Electrocautery-like electromagnetic interference that could cause inappropriate inhibition of pacemaker activity, more likely with procedures above the waist.
- Possible device reset or damage to the generator or leads, though this is unlikely.
ICD
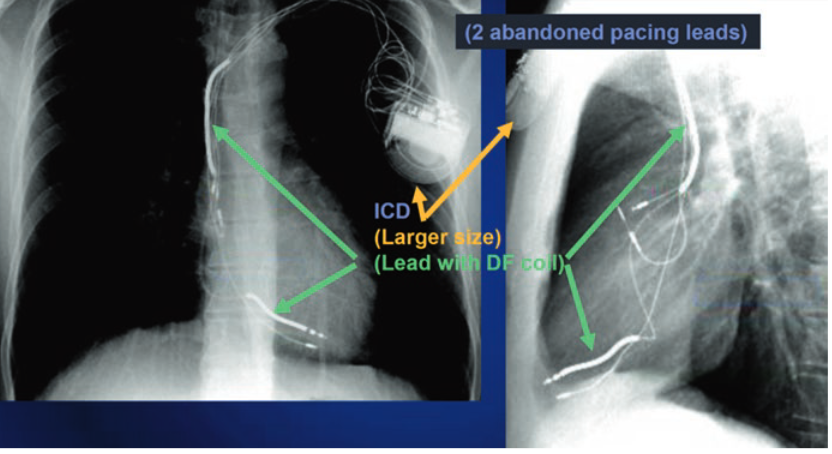
Radiographic Identification
- Larger generator
- Prominent right ventricular lead: Known as shock coils, these appear as two metallic segments along the length of the ICD lead.
Indications
- Patients at risk of sudden cardiac death: Prior ventricular tachycardia or fibrillation, low ejection fraction.
- Long QT syndrome
- Hypertrophic cardiomyopathy
- Arrhythmogenic right ventricular dysplasia
- Cardiac transplantation
- Primary electrical disease:
- Idiopathic ventricular fibrillation
- Short QT syndrome
- Brugada syndrome
- Catecholaminergic polymorphic ventricular tachycardia
Effects of Magnet
- Varies depending on the device, manufacturer, and programming.
- General effects:
- Turns off detection of tachycardia and tachycardia therapy (discharge and pacing).
- Typically, it has no effect on the pacemaker function (pacing will not become asynchronous).
- Pacemaker-dependent patients: Due to the risk of electrical interference and pacemaker malfunction, it is best to reprogram the device to address both tachycardia and bradycardia therapy.
Other Effects
- Electrocautery:
- Faulty sensing of intrinsic activity causing inappropriate sensing of arrhythmias, more prominent with monopolar cautery.
- Possible device reset or damage to the generator or leads, though this is unlikely.
- Radiation therapy:
- Possible device reset when performed near the device.
- Radiofrequency:
- Electrocautery-like electromagnetic interference that could cause inappropriate arrhythmia sensing inhibition.
- Possible device reset or damage to the generator or leads, though this is unlikely.
The Radiographic Image of a BiV ICD
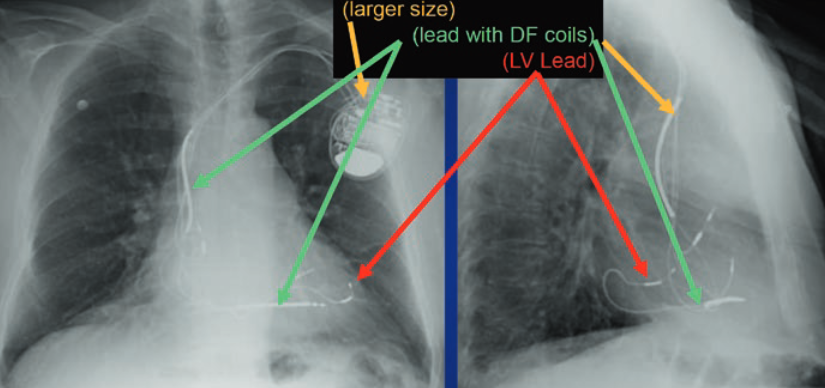
Radiographic ID
- Larger Generator
- Prominent Right Ventricular Lead: Shock coils
- Right Atrium Lead
- Coronary Sinus Lead
Indications
- Left Ventricular Dysfunction and Heart Failure: With prolonged ventricular conduction and heart failure symptoms.
- Required Ventricular Pacing and Low Ejection Fraction (EF): RV pacing in patients with low EF increases CHF admissions and mortality.
- Cardiac Resynchronization Therapy: Improves exercise tolerance and mortality. Continuous pacing provides better hemodynamic stability.
Pulselessness with a Magnet
- A BiV ICD patient with low ejection fraction and pacemaker dependency might experience pulselessness due to the magnet suspending tachyarrhythmia detection. Prolonged electrocautery use can inhibit pacing, and returning to an unresponsive myocardium after asystole may lead to PEA arrest.
Device Type and Information Gathering
- Patient History: Cardiac arrest, arrhythmias, or VT/VF?
- Medical Records and Registration Card: Evaluate thoroughly.
- Manufacturer Contact: Obtain specific device information.
Procedure Type
- Electromagnetic Interference: Consider location and presence.
Patient Characteristics
- Pacemaker Dependence:
- Monitor or EKG review can indicate dependence.
- Pacing spikes in front of most P waves and/or QRS complexes suggest dependency.
- Paced Chambers: Identify which chambers are being paced.
- Low EF Presence: Assess for this condition.
Urgency of the Case
- Elective Cases:
- Contact the patient’s provider.
- Pacemakers should be checked annually, ICDs biannually.
- Follow specific recommendations.
- Emergency Cases:
General Recommendations
a. Magnet Availability:
- Must call EP if magnet placement is impossible; device may require reprogramming.
b. Patient Monitoring: - Use plethysmography or arterial line.
- Other monitoring forms are unreliable due to electromagnetic interference.
c. Transcutaneous Pacing and Defibrillation Pads: Place anterior/posterior.
d. Pre-Discharge Evaluation: Assess pacemaker or ICD before leaving a cardiac-monitored environment.
e. Continuous Monitoring for ICD Patients: Until device reactivation.
f. Specific Surgery Programming: Patients must remain monitored until device reprogramming.
Recommendations for Non-Pacemaker Dependent Patients
a. No ICD Present:
- Surgery >6 inches (15 cm) from the device: No further action needed.
- Surgery <6 inches from the device: Use a magnet or reprogram to asynchronous mode (AOO, VOO, DOO).
b. ICD or BiV ICD Present:
- Place magnet to stop tachyarrhythmia detection.
- If magnet placement is impossible, or surgery <6 inches from the device, or is a cardiac/thoracic procedure, call the device specialist to deactivate tachyarrhythmia detection.
Recommendations for Pacemaker Dependent Patients
a. No ICD Present:
- Use short electrosurgical bursts.
- Place magnet over the device if surgery >6 inches from the device.
- If magnet placement is impossible or surgery <6 inches from the device, call device specialists to reprogram to an asynchronous mode.
b. ICD or BiV ICD Present:
- Use short electrosurgical bursts.
- Surgery >6 inches from the device: Place magnet over device to suspend tachyarrhythmia detection and contact device specialist for asynchronous mode reprogramming.
- If magnet placement is impossible or surgery <6 inches from the device, contact in-hospital device specialist for reprogramming to avoid electrical interference and deactivate tachyarrhythmia detection.
Heart Failure CXR
Systolic or Diastolic Heart Dysfunction
- Systolic Dysfunction: Inability to pump blood effectively out of the left ventricle (LV) → Blood pools in LV, backs up into left atrium (LA).
- Diastolic Dysfunction: Inability of LV to fully relax → Blood backs up in left atrium (LA).
Cardiomegaly
- Over time, LV and LA enlarge.
- Cardiomegaly: Cardiothoracic ratio > 0.5 on PA CXR.
- Note: Cardiomegaly cannot be assessed on AP CXR due to the nature of how an AP film is taken.
Increased Pulmonary Capillary Wedge Pressure (PCWP)
- Reflects blood pressure in the LA (Normal = 8-12 mmHg).
- Progressively increased PCWP: Indicates elevated left atrial pressure.
- Increased pressure in pulmonary vasculature: Due to systolic or diastolic dysfunction, the pressure backs up into the pulmonary vessels.
Hydrostatic Pressure in Pulmonary Capillaries
- PCWP (12-20 mmHg): Fluid pushed out of lung capillaries into lung interstitium → Interstitial edema.
- Fluid accumulates in peribronchovascular interstitium:
- Findings: Opacification of the area surrounding the hilar vasculature, perihilar haze, and peribronchial cuffing.
Further Increase in PCWP
- PCWP (20-25 mmHg): Fluid accumulates in interlobular interstitium.
- Findings:
- Kerley B lines: Small 1-2 cm horizontal lines at the periphery of the lung (often near costophrenic angles).
- Fluid in interlobular septa visible on CXR.
- Opacified/white interlobular fissures.
Advanced Left Heart Failure (LHF)
- PCWP (>25 mmHg): Fluid enters pleural spaces and alveoli.
- Findings:
- Pleural effusion: Fluid enters pleural spaces, causing opacities on CXR.
- Bilateral blunting of costophrenic angles on upright CXR (both PA and lateral views).
- Alveolar edema: Fluid spills into alveoli, leading to widespread airspace opacification.
Cephalization
- Cephalization: Increased blood flow to the upper lung fields due to redistribution from lower lung fields.
- Findings: On an upright CXR, upper lung vasculature appears enlarged compared to lower lung vasculature.
Paediatric Chest X-ray
Differences Vs Adults
- Limited Cooperation: Obtaining chest X-rays in children is challenging due to limited cooperation.
- Age-Related Changes: Chest X-rays change with age.
- Different Conditions: Children present with different conditions.
- Specific Areas to Review: There are specific areas to review when interpreting a pediatric chest X-ray.
- Thymus Confusion: The thymus can cause confusion in interpretation.
Approach
Check ID and Quality
- Age: Age will guide interpretation.
- Quality: Assess rotation, inspiration, and exposure. Overor underexposed films impair judgment on parenchymal density and vascularity.
- Position: Note AP, PA, and supine positions. Important in neonates due to different lung mechanics and rib angles. Poor positioning affects results.
- Orientation Markers: Ensure correct R and L markers to detect situs inversus or dextrocardia.
Bone Structure
- Skeleton Integrity: Check for humeral head ossification in premature neonates.
- Spine Visibility: The spine should be visible behind the mediastinum to reflect correct exposure.
- Rotation: Excluded if clavicles are symmetrical on either side of the midline.
- Ribs Direction: Ribs are flatter in neonates. Rib notching from coarctation visible after age 5.
- Trauma: Check shoulders and clavicles for delivery trauma and older children for non-accidental injuries (NAI).
- Skeleton Proportion: Higher proportion of the skeleton is visible in infants, including head, neck, upper limbs, pelvis, and hips. Check all these areas.
Tracheobronchial Tree and Mediastinum
- Trachea and Main Bronchi: Assess position and integrity.
- Foreign Body: Look for directly visible foreign bodies or indirect effects on ventilation.
- Thymus: Routinely visible until age 3, can obscure the heart shadow.
- Esophagus: Lines within the mediastinum should be visible; check for esophageal atresia if the nasogastric tube curls up.
- Mediastinal Tumors: Common in children include lymphomas, neurogenic tumors (ganglioneuromas), thymomas, teratomas, and lipoblastomas.
Heart Silhouette
- Cardiovascular Clues: Provides clues for cardiovascular malformations. Consider cyanotic or non-cyanotic conditions.
- Heart Assessment: Consider heart size, shape, and position.
- Lung Vasculature: Examine pulmonary vessels in the hila and overall lung vascularity. Check for hypoor hypervascularization. Correct X-ray exposure is crucial.
Contours of Thorax
- Systematic Review: Inspect all peripheral regions of the thoracic cavity.
- Apices Check: Check for pneumothoraces, especially in supine children.
- Margins and Hemidiaphragms: Inspect mediastinum and heart silhouette margins, costodiaphragmatic angles, and hemidiaphragm positions and shapes. Note visible fissures.
Lung Fields
- Symmetrical Comparison: Compare lung translucency, inflation, parenchyma, vascularization, and markings symmetrically. Diaphragmatic hernias usually occur on the left side.
- Quality X-ray: Needed to distinguish parenchymal disease or abnormal vasculature. Determine if pathology is lung or cardiovascular system-related. Unilateral pathology suggests a local process, bilateral symmetrical aspect suggests a systemic condition.
Abdomen
- Symmetrical Comparison: Same points as lung fields. Diaphragmatic hernias usually occur on the left side.
- Quality X-ray: Necessary for identifying and distinguishing parenchymal disease or abnormal vasculature. Determine if the pathology is lung or cardiovascular system-related. Unilateral pathology suggests a local process, bilateral symmetrical aspect suggests a systemic condition.
Soft Tissues
- Body Fat: Absent in premature children.
- Edema: Check for hydrops fetalis.
- Surgical Emphysema: Inspect for surgical emphysema.
Lines, Tubes, and Artifacts
- Lines: Check correct positions of umbilical artery or vein catheters, central venous catheters, PICC, nasogastric tubes, endotracheal tubes, shunts, and drains in children in PICU or NICU.
- Artifacts: Include umbilical clips, skin folds, monitoring equipment, cots, or ventilator parts.
Other
Radiopaque Foreign Body
- Distinguishing Features: Differentiate between a battery/magnet and a simple coin. A battery shows a double halo on X-ray and requires urgent removal if stuck in the esophagus.
Radiolucent Foreign Body
- Indirect Signs:
- Normal or air trapping with air bronchograms.
- Atelectasis and partial or total lung collapse.
- Hyperinflation of affected lung with/without mediastinal shift.
- Pneumothorax or air in the mediastinum.
- Consolidation.
- Hyperinflated right lung with increased translucency, flattened right hemidiaphragm, wider spaced right ribs, and mediastinal shift to the left indicating obstruction.
Links
- Heart failure
- Asthma and Chronic Obstructive Pulmonary Disease (COPD)
- Acute Respiratory Distress Syndrome (ARDS)
- Tuberculosis (TB)
References:
- Raj, T. D. (2017). Data interpretation in anesthesia.. https://doi.org/10.1007/978-3-319-55862-2
- Gambato M, Scotti N, Borsari G, Zambon Bertoja J, Gabrieli JD, De Cassai A, Cester G, Navalesi P, Quaia E, Causin F. Chest X-ray Interpretation: Detecting Devices and Device-Related Complications. Diagnostics (Basel). 2023 Feb 6;13(4):599. doi: 10.3390/diagnostics13040599. PMID: 36832087; PMCID: PMC9954842.
- Puddy, E. and Hill, C. (2007). Interpretation of the chest radiograph. Continuing Education in Anaesthesia Critical Care &Amp; Pain, 7(3), 71-75. https://doi.org/10.1093/bjaceaccp/mkm014
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “d737b755-6a34-40a1-8d57-08d3fa4015a3”



