{}
Summary
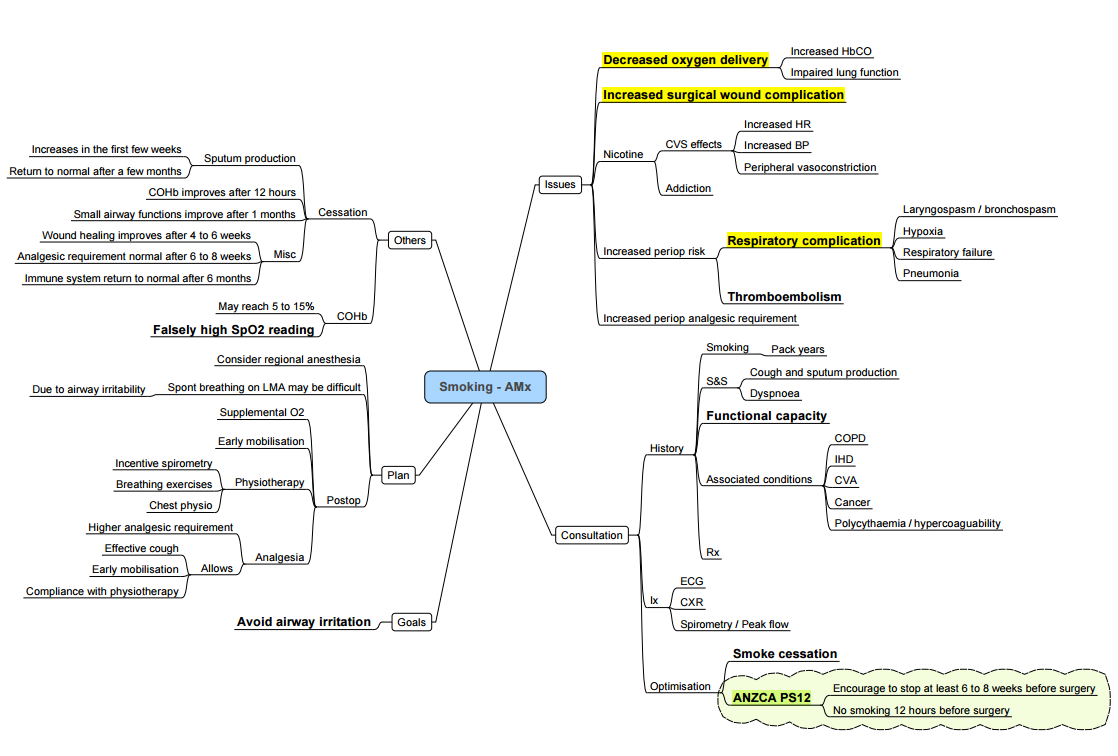
Effects of Smoking and Anaesthesia
Main Effects
Primarily: Inadequate delivery of usable oxygen to the tissues
Cardiovascular System (CVS)
- Conditions:
- Hypertension
- Ischaemic heart disease (IHD)
- Cerebrovascular accident (CVA)
- Heart failure
- Risks:
- Increased postoperative cardiovascular morbidity and mortality
- Nicotine:
- Stimulates adrenal medulla to release adrenaline
- Resets carotid body and aortic receptors, resulting in higher blood pressure
- Stimulates autonomic ganglia, increasing sympathetic nervous system tone
- Myocardial Oxygen Supply-Demand Imbalance:
- Increases myocardial contractility, heart rate (HR), systolic blood pressure (SBP), diastolic blood pressure (DBP), and peripheral vascular resistance (PVR)
- Decreases coronary blood flow due to increased coronary vascular resistance
- Increases intracellular calcium during ischemia, exacerbating myocardial damage
- Carbon Monoxide:
- Elevates carboxyhaemoglobin (COHb) levels
- Shifts the oxygen dissociation curve (ODC) to the left, reducing oxygen availability to tissues
- Inhibits cytochrome oxidase and binds with myoglobin, leading to decreased intracellular oxygen transport and usage, and a negative inotropic effect
- Leads to chronic tissue hypoxia
- Increases risk of ventricular arrhythmias under general anaesthesia if COHb > 5%
Respiratory System
- Impaired tracheobronchial clearance, resulting in lower airway reactivity (hyperviscous mucus with altered elasticity; cilia damaged by cilotoxins and become inactive)
- Increased laryngeal and bronchial reactivity, leading to breath-holding and laryngospasm at induction
- Faster decline in forced expiratory volume in one second (FEV1) compared to non-smokers
- Increased closing volume
- Small airway disease due to decreased surfactant
- Greater degree of shunt under anaesthesia
- Increased incidence of chronic obstructive pulmonary disease (COPD) and chronic bronchitis
- Increased levels of proteolytic and elastolytic enzymes, resulting in loss of elastic recoil and emphysema
- Increased lung infections
- Increased incidence of perioperative respiratory adverse events (PRAEs)
Gastrointestinal System
- Increased risk of peptic ulcer disease
- Transient gastro-oesophageal sphincter incompetence
Immune System
- Increased risk of infection and malignancy
Renal System
- Increased sympathetic nervous system activity, resulting in increased antidiuretic hormone (ADH) release and dilutional hyponatraemia
Drug Metabolism
- Induces liver enzymes, increasing metabolism of some drugs
- Higher doses required for some analgesics
- Fentanyl metabolized faster
- No effect on codeine, paracetamol, or NSAIDs
- Higher doses of benzodiazepines needed due to end-organ reduced response, not drug metabolism
- Volatile agents: No change in action but increased metabolism, leading to higher levels of toxic metabolites
- Muscle relaxants: Small doses of nicotine stimulate acetylcholine receptors, requiring larger doses to block receptors
Psychological Effects
- Acute withdrawal symptoms: anxiety, sleep disturbances, irritability
Pack Year Calculation
-
Pack-years = (Number of cigarettes smoked per day ÷ 20) × Number of years smoked
- 20 cigarettes = 1 pack
- So you divide by 20 to convert cigarettes into packs.
-
Example 1:
-
Smokes 10 cigarettes a day for 30 years:
→ (10 ÷ 20) × 30 = 15 pack-years -
Example 2:
-
Smokes 40 cigarettes a day (2 packs) for 10 years:
→ (40 ÷ 20) × 10 = 20 pack-years
Timing of Smoking Cessation and Effects on Physiological Recovery
Timeline of Recovery after Smoking Cessation
- 12-24 hours:
- Negates effects of nicotine and COHb.
- Increases physical work capacity by 10-20%.
- 4-6 days:
- Ciliary activity recovers, but sputum production increases.
- 5-10 days:
- Laryngeal and bronchial reactivity to settle.
- 4 weeks:
- Improvement in small-airway narrowing.
- 6 weeks:
- Sputum volume returns to normal.
- More than 8 weeks:
- Four times less pulmonary complication.
- 3 months:
- Tracheobronchial clearance improves.
- 6 months:
- Marked improvement: equal incidence of postoperative pulmonary complication as non-smokers.
Recommendations
- Optimal Timing for Smoking Cessation:
- The best result occurs when the patient stops smoking 8 weeks or more before surgery. This significantly reduces perioperative-specific respiratory events and postoperative morbidity, eliminates carbon monoxide and nicotine, improves clearance of tracheobronchial secretions, decreases small-airway narrowing, and enhances immune functioning.
- If Unable to Stop 8 Weeks Before Surgery:
- Patients should stop smoking at least 12 hours before surgery or, if the surgery is the next morning, the previous evening. This will eliminate problems in tissue oxygen uptake due to carbon monoxide and reduce the cardiac and hemodynamic effects of nicotine.
Additional Recommendations
- Duration to Stop:
- 6-8 weeks for the return of normal immune function. Short-term abstinence has not been shown to reduce the incidence of postoperative pulmonary complications. Immediate preoperative cessation may be harmful due to anxiety and increased sputum production.
- Predictors for Pulmonary Complications:
- 60 pack years, decreased diffusing capacity of the lungs for carbon monoxide (DLCO).
Links
References:
- Carrick, M., Robson, J. M., & Thomas, C. (2019). Smoking and anaesthesia. BJA Education, 19(1), 1-6. https://doi.org/10.1016/j.bjae.2018.09.005
- Rodrigo C. The effects of cigarette smoking on anesthesia. Anesth Prog. 2000 Winter;47(4):143-50. PMID: 11432181; PMCID: PMC2149030.
- The Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- ICU One Pager. (2024). Retrieved June 5, 2024, from https://onepagericu.com/
Summaries:
Smoking
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “b98ea2ec-1762-4394-bdca-f881607aa948”



