- Thermoregulation
- Effects of Anaesthesia on Thermoregulatory Responses
- Physiological Consequences of Hypothermia
- Patterns of Hypothermia under General Anaesthesia
- Effects of Anaesthetic Drugs on Hypothermia
- Prevention of and Management of Hypothermia
- Temperature Monitoring
- Methods for Warming Patients
- Hyperthermic Toxidromes
- Links
{}
Thermoregulation
Afferent Sensing
- Cold Signals: Transmitted by TRPV1-4 receptors through Aδ fibers.
- Warm Signals: Transmitted by TRPM8 and A₁ receptors through C fibers.
- Signals ascend predominantly in the spinothalamic tract in the anterior spinal cord.
Central Regulation
- Pre-optic Area of Anterior Hypothalamus: Contains temperature-sensitive neurons that increase or decrease firing rate in response to warming or cooling of the hypothalamus, respectively.
- Anterior Hypothalamus: Integrates afferent responses and governs vasodilation.
- Posterior Hypothalamus: Governs vasoconstriction, integrates peripheral cold afferents, and modulates descending effector responses.
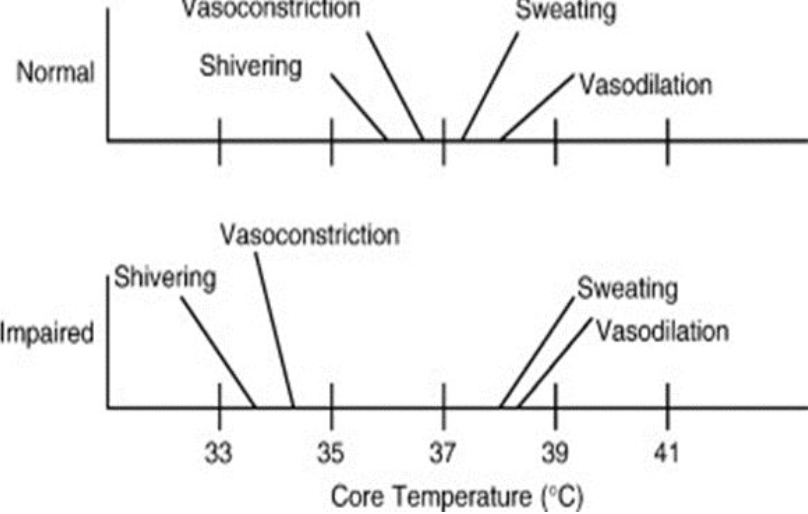
- Interthreshold Range: Core temperature range is approximately 37°C ± 0.2°C.
Efferent Responses
- Behavioral: Triggered by skin afferents.
- Autonomic: Triggered by core afferents.
- Cold Defenses:
- Vasoconstriction and piloerection (36.8°C)
- Non-shivering thermogenesis (NST) (36°C)
- Shivering (35.7°C)
- Heat Defenses:
- Sweating and vasodilation (both at 37°C)
- Cold Defenses:
Non-Shivering Thermogenesis
- Infants: Occurs in brown fat.
- Mechanism:
- Cold exposure → Noradrenaline release → Activation of β₃ receptors on brown fat → Adenylate cyclase (AC) activation → cAMP production → Protein kinase A (PKA) activation → Hormone-sensitive lipase activation → Lipolysis and beta-oxidation of fatty acids → Increased oxygen consumption and metabolic heat production without mechanical work.
- Thermogenin: Pumps H⁺ into mitochondria, uncoupling oxidative phosphorylation → Increased electron transport chain (ETC) activity → Large quantities of ATP generated and broken down.
Physics of Temperature Regulation
Routes of Heat Loss
- Radiation: 40%
- Convection: 30%
- Evaporation: 20%
- Respiration: 10%
Conduction
- Transfer of heat by direct collision between particles of high and low thermal energy.
Convection
- Passive Convection: Heated molecules rise due to decreased density, replaced by cooler molecules due to gravity (warm air rises).
- Active Convection: Warmed molecules moved away by air currents (e.g., fan).
Evaporation
- Utilizes latent energy to break intermolecular bonds, cooling the body as high-energy molecules evaporate, leaving lower-energy molecules behind.
Radiation
- Continuous emission of electromagnetic energy by hot bodies as thermal radiation.
Definitions
- Temperature: Average kinetic energy of all particles (K or °C).
- Thermal Energy: Total energy a body contains due to its temperature (J).
- Heat: Transfer of thermal energy from a body with higher thermal energy to one with lower thermal energy.
- Zero Point of Kelvin: Point at which the body contains no thermal energy (theoretical, unattainable).
- Zero Point of Celsius: Point at which water freezes (273.15 K).
- Zero Point of Fahrenheit: Point at which brine freezes (255 K).
- Specific Heat Capacity: Amount of energy required to increase the temperature of 1 kg of a substance by 1°C.
- Water (liquid): 4.18 J·g⁻¹·°C⁻¹.
Latent Heat
- Amount of energy liberated (de-ionization, condensation, freezing, deposition) or absorbed (melting, evaporation, ionization, sublimation) during a phase change.
Physiology of Heat Loss
Responses to Temperature Extremes
- Too Cold:
- Piloerection: Traps warmed air around the body, reducing conduction and convection.
- Shivering: Generates heat through inefficient energy use for muscle contraction.
- Behavioral Change: Putting on clothes reduces conduction and convection.
- Too Hot:
- Behavioral Change: Taking off clothes increases heat loss.
- Vasodilation: Increases heat loss by electromagnetic radiation.
- Sweating: High-energy molecules evaporate, diminishing heat through latent heat of vaporization; reduced by high humidity and insulating clothing.
Cold Stress in Neonates
- Increased noradrenaline release
- Increased oxygen and substrate consumption
- Activation of the sympathetic nervous system
- Increased pulmonary vascular resistance
- Increased right-to-left shunting
- Decreased peripheral perfusion and oxygen delivery
- Acidosis
- Altered pharmacokinetics and dynamics of drugs, such as muscle relaxants and volatile agents
Effects of Anaesthesia on Thermoregulatory Responses
General Anesthesia
- Impairment of Thermoregulation: All general anesthetic agents impair thermoregulation in a dose-dependent manner through central mechanisms and by increasing the interthreshold range (2-4°C vs normal 0.4°C).
- Warm Response Thresholds: Slightly elevated.
- Cold Response Thresholds: Markedly reduced.
- Effector of Behavioural Change: Removed.
- Neuromuscular Blockade: Prevents shivering.
Heat Loss Under Anaesthesia
- Children: Greater heat loss through conduction and radiation than adults due to less insulating subcutaneous fat and higher surface area-to-volume ratio.
- Heat Production: Reduced by 20-30% during anesthesia due to decreased basal metabolic processes.
- Mechanically Ventilated Neonates: Lack heat generated through work of breathing.
- Central Thermoregulation: Inhibition and delayed vasoconstriction at lower core temperatures.
- Non-shivering Thermogenesis: Loss of usual heat production mechanisms.
Neuraxial Anaesthesia
- Autonomic Regulation: Central and peripheral autonomic regulation due to sympathectomy is less affected than with general anesthesia.
- Core Hypothermia: May occur without the sensation of feeling cold due to skin afferent signal obliteration by vasodilation.
- Cold Sensitivity: Decreased above the block level due to a false reduction of cold signals from the legs.
- Vasoconstriction: Obliterated below the block level, leading to no heat loss plateau.
Neuraxial Heat Loss Mechanisms
- Redistribution of heat is confined to the lower part of the body.
- No heat loss plateau due to inability to vasoconstrict.
- Increased interthreshold range to 0.9°C.
- Shivering confined to the upper body.
Physiological Consequences of Hypothermia
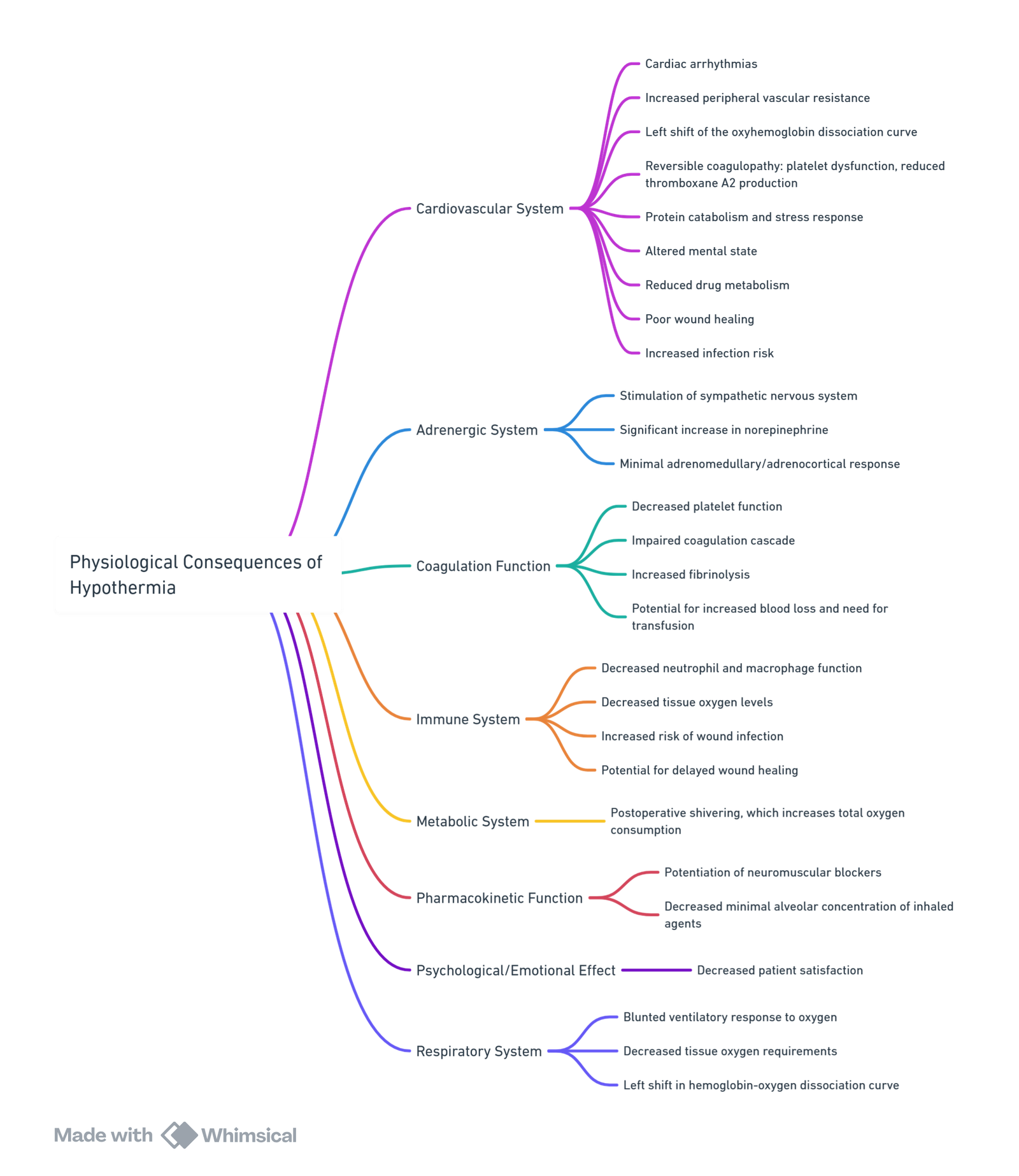
View or edit this diagram in Whimsical.
Patterns of Hypothermia under General Anaesthesia
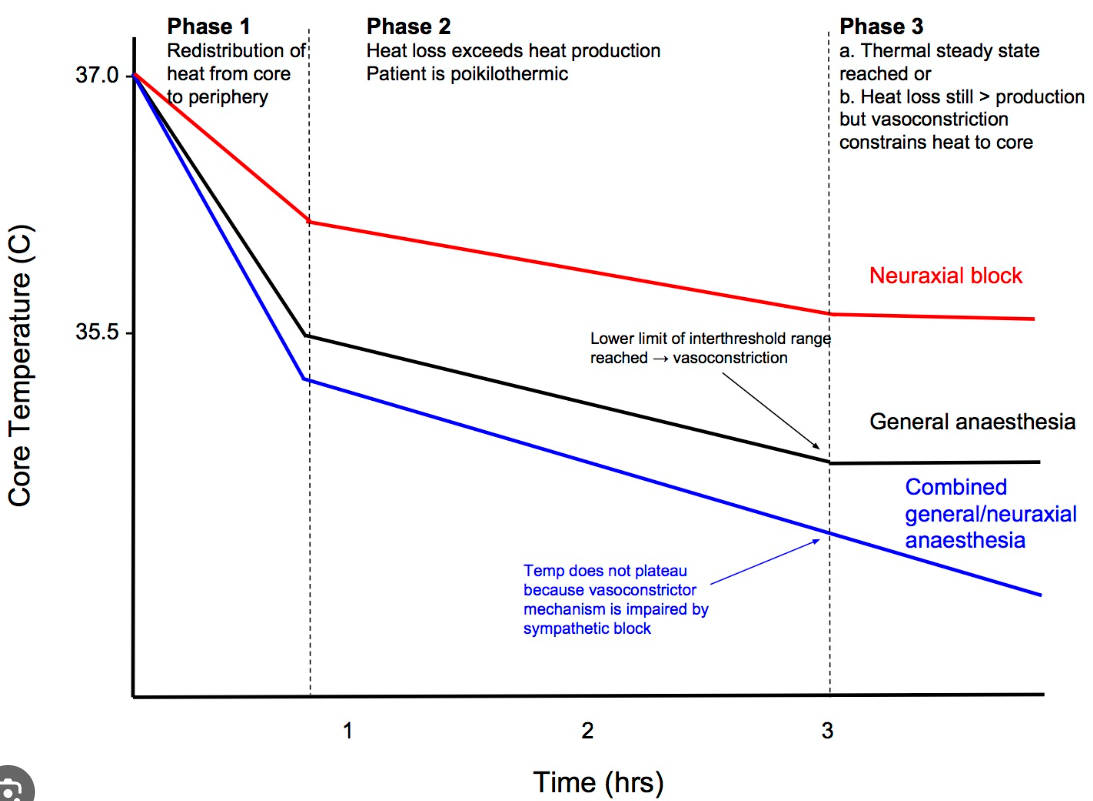
General Anaesthesia
Rapid Decline
- Temperature Drop: 0.5-1.5°C
- Time Frame: Within the first hour of anesthesia.
- Mechanism: Primarily due to thermal redistribution.
- Thermal Redistribution: The initial drop in core temperature occurs when the heat loss from the body exceeds metabolic heat production. Normally, the body maintains temperature through vasoconstriction. However, under anesthesia, the threshold for vasoconstriction is reduced, leading to peripheral vasodilation, which allows heat to escape from the core to the periphery (arms and legs). The rapid decline phase ends once the patient reaches a new steady-state where the core and periphery are closer in temperature.
Slow Linear Decline
- Time Frame: Next 1-2 hours.
- Mechanism: Due to heat loss exceeding metabolic heat production. This phase involves a steady decrease in core temperature as the body continues to lose heat to the environment.
Plateau
- Time Frame: After 3-4 hours of anesthesia.
- Mechanism: A new thermal steady state is achieved where heat loss equals metabolic heat production. At this stage, peripheral vasoconstriction is triggered when the core temperature reaches approximately 33-34°C, leading to a plateau in the temperature decline. The core temperature remains relatively stable, although the total heat content of the body continues to fall due to ongoing heat loss from the peripheries.
Neuraxial Anesthesia
- Thermal Redistribution: Differs from general anesthesia. The initial drop in core temperature is still observed, but redistribution is more confined to the lower half of the body due to the effects of the neuraxial block.
- Core Temperature Decline: Typically less than 0.5°C.
- Shivering and Vasoconstriction: Confined to regions above the block level, leading to a less pronounced plateau phase. The absence of vasoconstriction below the level of the block contributes to a continuous decline in temperature.
- Clinical Implication: Effective temperature monitoring and warming techniques are crucial to prevent hypothermia, particularly when combining general and neuraxial anaesthesia.
Effects of Anaesthetic Drugs on Hypothermia
- All anaesthetics slightly increase the sweating threshold while markedly decreasing the vasoconstriction and shivering thresholds.
- Dexmedetomidine: Does not alter the sweating threshold but linearly reduces the vasoconstriction and shivering thresholds.
- Propofol Infusion: Reduces the vasoconstriction and shivering thresholds.
- Ketamine: Reduces the magnitude of redistribution hypothermia, maintains vasoconstriction of arteriovenous shunts during the induction of anaesthesia.
- Neuromuscular Blocking Agents: Prevent motor activity, including shivering, and therefore prevent heat generation from muscle activity.
- Pethidine: Acts as an anti-shivering agent, decreasing the shivering threshold more effectively than the vasoconstrictor response.
- Anti-cholinergic Drugs: Increase the threshold for sweating and promote hyperthermia.
- Ephedrine: Increases skeletal muscle metabolism and can elevate temperatures.
- Phenylephrine: Causes precapillary vasoconstriction, reducing heat loss from redistribution.
- Midazolam: Has minimal influence on thermoregulatory control.
Prevention of and Management of Hypothermia
Guidelines And Recommendations
The UK NICE guidelines emphasize the importance of identifying at-risk patients, initiating warming in the preoperative period, and maintaining temperature regulation throughout the perioperative and recovery phases.
Preoperative Management
Patients with two or more of the following risk factors are considered at risk for perioperative hypothermia:
- ASA grade II to V (higher grades indicate greater risk).
- Preoperative temperature <36.0°C (if preoperative warming is not feasible due to clinical urgency).
- Undergoing combined general and regional anaesthesia.
- Undergoing major or intermediate surgery.
- At risk of cardiovascular complications.
Temperature monitoring and warming:
- Preoperative temperature should be measured in the ward.
- If <36.0°C, active warming must be started unless surgery is urgent.
- If ≥36.0°C, warming should begin 30 minutes before induction, provided it does not delay emergency surgery.
Timing Of Preoperative Warming
A South African review suggests:
- If surgery lasts >2 hours or combined anaesthesia and surgery exceed 30 minutes, pre-warming is advised.
- Routine warming is recommended for neonates and infants (<1 year old).
- Theatre temperature should be maintained at 21°C–24°C.
Intraoperative Management
- Temperature should be recorded before induction and every 30 minutes thereafter.
- If <36.0°C, delay induction and warm the patient unless delaying surgery is unsafe.
- The theatre suite temperature should be 21°C when the patient is exposed, and reduced to an appropriate temperature once surgery begins.
- Maintain forced-air warming or resistive heating blankets throughout surgery.
- Minimize patient exposure except during cleaning and draping.
- All IV fluids and blood products must be warmed before administration.
Postoperative (Recovery) Management
- Temperature should be documented on arrival in recovery and every 15 minutes.
- If <36.0°C, active warming should be initiated.
- Patients should only be discharged to the ward if core temperature is >36.0°C.
Prevention And Treatment of Redistribution Hypothermia
Redistribution hypothermia occurs due to vasodilation from anaesthesia. Strategies to prevent it include:
Preoperative Warming
- NICE guidelines recommend warming if the temperature is <36.0°C, maintaining 36.5°C–37.5°C perioperatively.
- Skin warming for 30 minutes pre-induction significantly reduces redistribution hypothermia.
- For children, increase the ambient temperature to 26°C for 30-40 minutes before induction.
Airway Heating and Humidification
- Heat loss from respiration accounts for 10% of total heat loss.
- Low fresh gas flows, heat-moisture exchange filters, and semi-closed circuits help minimize losses.
Warming IV Fluids
- Infusing cold IV fluids can cause significant heat loss.
- All intraoperative fluids >500 mL should be warmed.
- Rapid transfusion (>100 mL/min) of cold blood (4°C) or fluids can cause severe hypothermia.
- WHO guidelines prioritize maintaining patient temperature over warming blood, except in massive transfusions (>50 mL/kg/h in adults, >15 mL/kg/h in children).
Comparison Of Fluid Warming Devices
| Device | Advantages | Disadvantages | Remarks |
|---|---|---|---|
| Warming Cabinets | Cheap, simple | Cooling at low flow rates | Fluids must be stored overnight for uniform warming |
| Counter-current warming system | Maintains heat even at low flow rates | Risk of infection, air embolism, electrolyte disturbances | Uses non-sterile water around a sterile infusion lumen |
| Blood Warmer | Effective for blood warming | Risk of haemolysis, electrolyte disturbances | Operates at a max temperature of 43°C |
| Dry Heat Technology | Precise temperature control | None significant | Uses aluminium plates for heat transfer |
Cutaneous Warming
- Skin exposure contributes significantly to heat loss via radiation, evaporation, and convection.
- Maintaining operating room temperatures at 23°C (adults) and 26°C (infants) helps minimize heat loss.
Comparison Of Active Cutaneous Warming Devices
| Device | Mechanism | Advantages | Disadvantages | Remarks |
|---|---|---|---|---|
| Forced-air warmers | Convection | Safe, effective, fast warm-up, high capacity | Costly, disrupts laminar flow, infection risk | Most commonly used intraoperatively |
| Radiant heaters | Radiation | Fast warm-up, good warming capacity | Bulky, burn risk | Commonly used in recovery rooms |
| Resistive heating devices | Conduction | Reusable, cost-effective, does not disrupt airflow | Burn risk, slow warm-up | Uses electric current in polymer/carbon fibres |
| Circulating water mattresses | Conduction | No ambient warming | Slow heating, limited surface area coverage | Less effective than over-body warming |
| Circulating water garments | Conduction | Transfers large heat amounts | Bulky, risk of water leakage | Covers both anterior & posterior body |
| Negative pressure warming | – | Enhances peripheral-to-core heat transfer | Burn risk, questionable intraoperative role | Uses sub-atmospheric pressure to improve perfusion |
Temperature Monitoring Guidelines (SASA 2018)
- Monitoring core temperature during general and neuraxial anaesthesia if surgery lasts >30 minutes.
- Targeting a core temperature of 36-37°C by:
- Controlling ambient temperature.
- Using active warming devices.
- Preventing and treating surgical and patient-related causes of hypothermia.
Temperature Monitoring
Core Temperature (Preferred)
- Sites: Rectum, nasopharynx, oesophagus, temporal artery, bladder, tympanic membrane, and blood measurement.
Non-core Temperature
- Sites: Axillary thermometry (accuracy depends on continuous proximity to axillary artery), skin probes.
Tympanic Thermometers
- Measure thermal radiation from the ear canal, approximating the temperature of blood bathing the hypothalamus.
- Inaccuracies in children may occur due to small ear canals, leading to under-reading.
Nasopharyngeal Probes
- Placed blind once the patient is asleep, with the tip positioned behind the soft palate.
- Cooling effect of inspired gases, especially with uncuffed ETT or LMA, may affect accuracy.
- Closely equate to pulmonary artery blood temperature in children in intensive care.
Oesophageal Probes
- May become inaccurate during surgeries like thoracotomy.
- Less prone to cooling than nasopharyngeal probes due to their advanced position beyond the pharynx.
- In adult cardiac surgery, they equate most closely with pulmonary artery temperature.
Rectal Probes
- Commonly used when nasopharyngeal probes cannot be used.
- Regional blood flow and presence of stool may affect accuracy.
- Rectal temperatures may lag behind other core temperature measurements, especially during rapid temperature changes.
Bladder Temperature
- Closely equates with pulmonary artery temperature in adults undergoing cardiac surgery and critically ill children following cardiac surgery.
- Requires reasonable urine flow; may equate more closely with rectal temperature in oliguria.
Platinum Resistance Thermometers, Thermistors, and Thermocouples
Platinum Resistance Thermometer
- Resistance of platinum wire increases linearly with temperature.
- Not very sensitive.
Thermistor
- Made of metal oxide semiconductor whose resistance decreases as temperature increases (negative thermal conductivity).
- Added to a Wheatstone bridge.
- Non-linear relationship compensated by algorithms.
- Cheap, sensitive, and convenient.
Thermocouples
- Based on the Seebeck effect: Two dissimilar metals joined at two junctions. A temperature difference between the junctions causes a current flow, varying with the temperature difference.
- Calibrated to ambient temperature (cold junction compensator).
- Can be very small, resulting in low specific heat capacity and rapid response, very sensitive and accurate.
Methods for Warming Patients
General Measures
- Warm pre-operatively.
- Walk to the theater.
- Ambient theater temperature: 20-30°C.
- Limit large areas of skin exposure, especially wet skin.
Specific Measures
- Forced air warmers.
- Fluid warmers/warm IV fluids.
Caution
- Children receiving active warming intraoperatively are at risk of overheating.
- Risk of burns from non-uniform warming devices.
Effects of Hyperthermia
- Localized increased skin and muscle blood flow, increased vascular permeability, and edema.
- Potential cell death and organ failure.
Hyperthermic Toxidromes
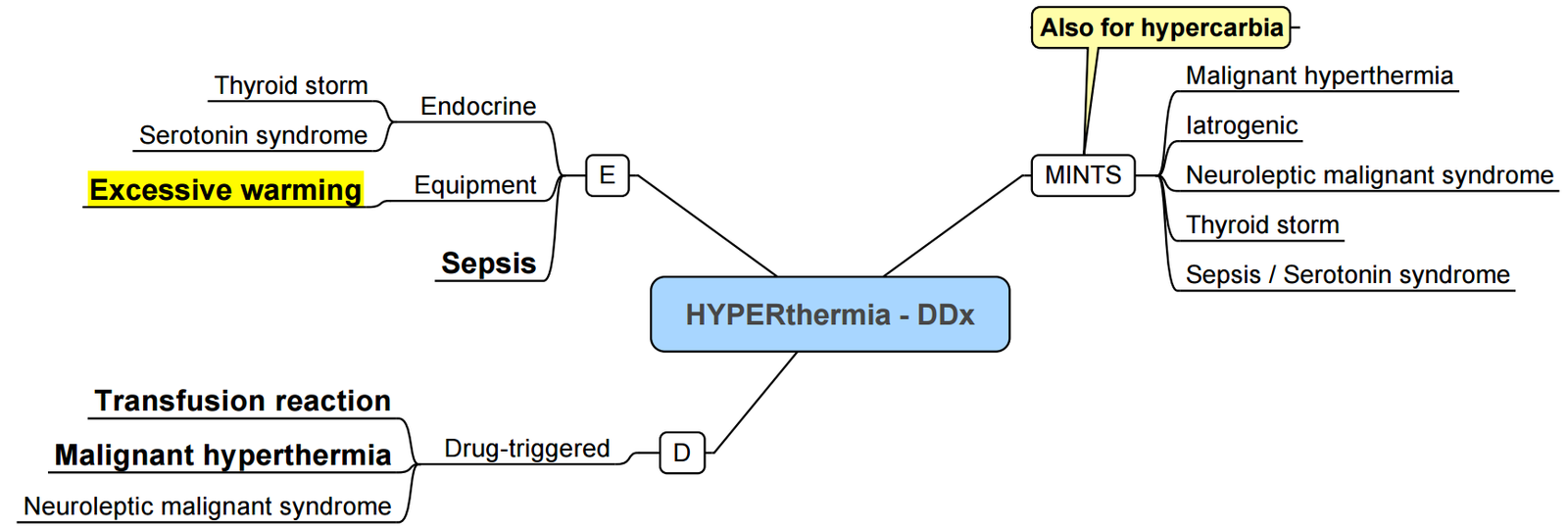
Hyperthermia Syndromes
| Feature | Serotonin Syndrome | Neuroleptic Malignant Syndrome (NMS) | Malignant Hyperthermia | Malignant Catatonia |
|---|---|---|---|---|
| Cause | Serotonin agonist | Dopamine antagonist (e.g., antipsychotics) OR abrupt cessation of dopamine agonist (e.g., Parkinson’s meds) | Autosomal dominant (AD); exposed to volatile anesthetics or succinylcholine | Unknown; occurs in patients with psychiatric/medical comorbidities |
| Onset | Sudden (within 24 hours) | Gradual (days to weeks) | Very rapid | Acute or insidious |
| Vitals | Hyperthermia, tachycardia, hypertension, tachypnea | Hyperthermia, hypertension, tachypnea | Hyperthermia, hypercarbia, sinus tachycardia | Fever, autonomic instability (e.g., ↑BP, tachycardia, tachypnea, diaphoresis) |
| Muscle Tone | Increased | “Lead pipe” rigidity | Generalized muscle rigidity | Rigidity |
| Reflexes | Hyperreflexia, clonus | Hyporeflexia | ? | ? |
| Mental Status | Agitated | Lethargic | ? | Altered |
| Treatment | Benzodiazepines, Cyproheptadine (resolves in ~24 hrs) | Bromocriptine (resolves in days to weeks) | FiO₂ 100%, increase ventilation, discontinue triggering agent, administer dantrolene | Lorazepam challenge (should respond rapidly, within minutes) |
Links
References:
- Bindu B, Bindra A, Rath G. Temperature management under general anesthesia: Compulsion or option. J Anaesthesiol Clin Pharmacol. 2017 Jul-Sep;33(3):306-316. doi: 10.4103/joacp.JOACP_334_16. PMID: 29109627; PMCID: PMC5672515.
- Sullivan, G. and Spencer, M. (2022). Heat and temperature. BJA Education, 22(9), 350-356. https://doi.org/10.1016/j.bjae.2022.06.002
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- ICU One Pager. (2024). Retrieved June 5, 2024, from https://onepagericu.com/
- Riley, C. L. and Andrzejowski, J. (2018). Inadvertent perioperative hypothermia. BJA Education, 18(8), 227-233. https://doi.org/10.1016/j.bjae.2018.05.003
Summaries:
Hyperthermic toxidromes
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “2ea0312d-88d5-4ce5-9c8f-df53b6301ec3”



