{}
Vasculitis
Chapel Hill Consensus Conference Nomenclature for Vasculitis
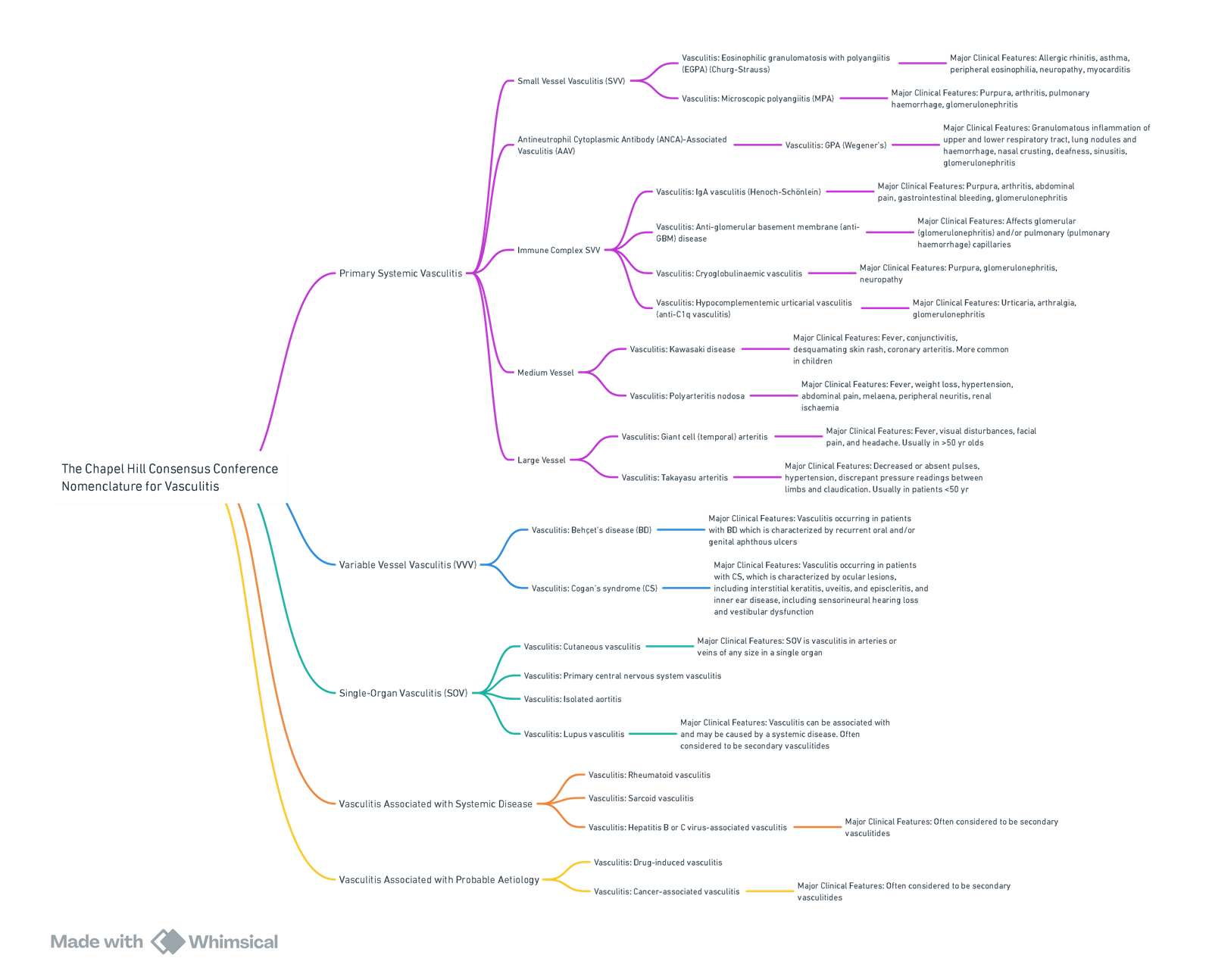
View or edit this diagram in Whimsical.
Anaesthesia for Vasculitis
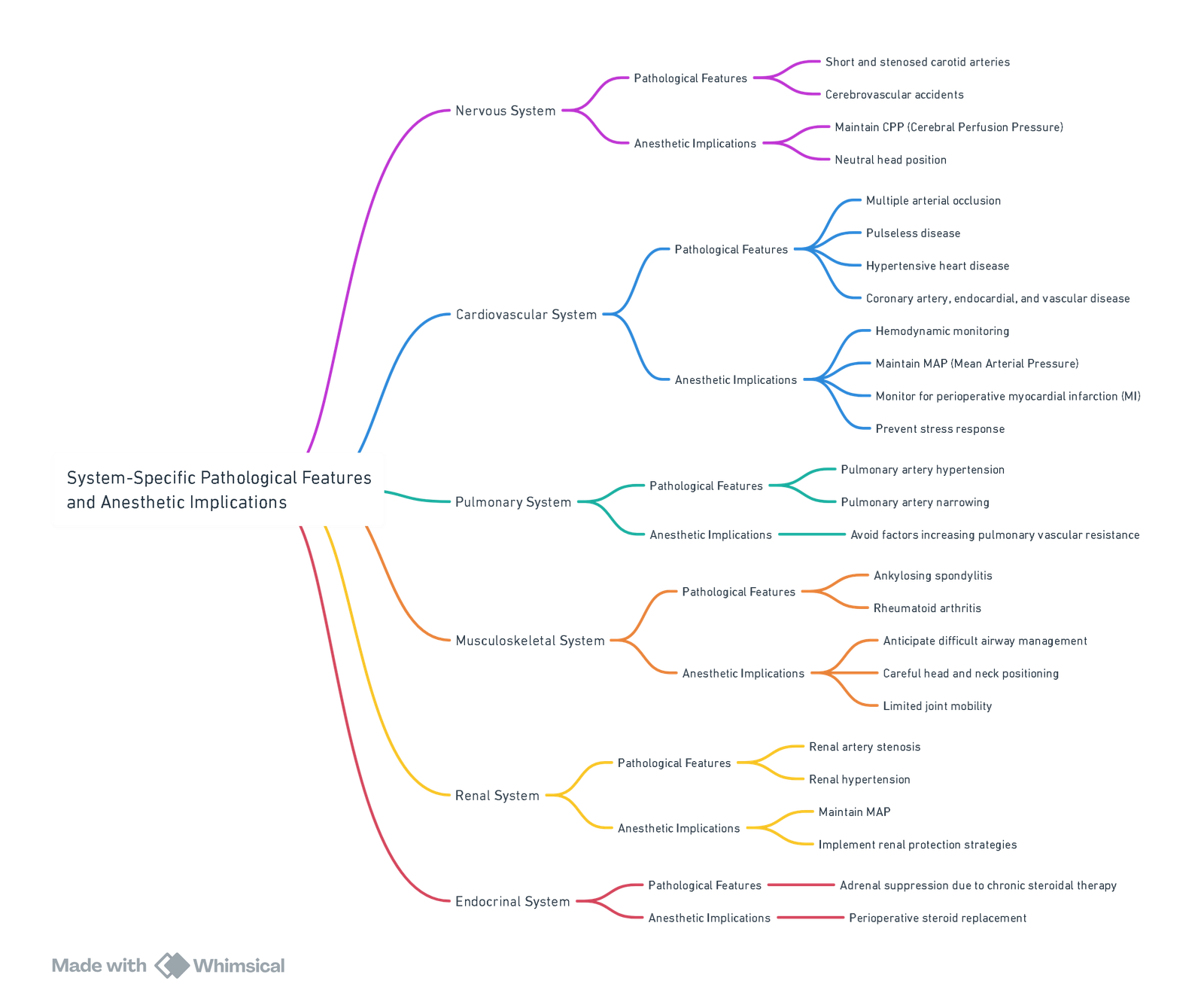
View or edit this diagram in Whimsical.
Conduct of Anaesthesia for Vasculitis
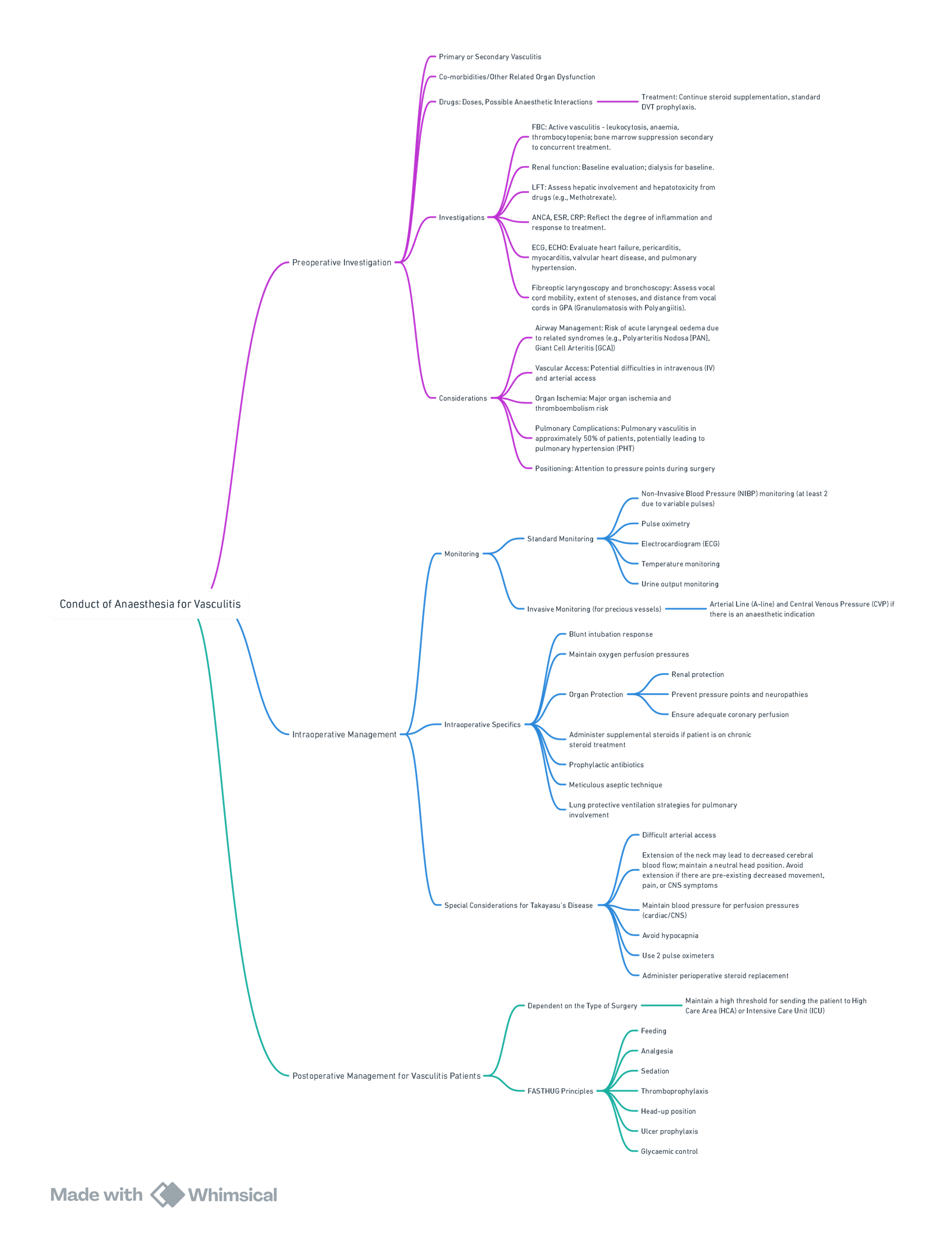
View or edit this diagram in Whimsical.
Wegener’s Granulomatosis
Considerations
- Potential difficult airway: laryngeal stenosis, subglottic stenosis, tracheal stenosis, friable bleeding tissue
- Multisystem granulomatous disease:
- CNS: cerebral aneurysms, peripheral neuropathy
- Cardiovascular: cardiac valve destruction, conduction defects, myocardial ischemia
- Pulmonary: sinusitis, pulmonary fibrosis, pulmonary hypertension, pneumonia, hemoptysis, and bronchial destruction
- Renal: hematuria, renal failure
- Possible contraindication to arterial line due to peripheral arteritis
- Medications including immunosuppressants
Goals & Conflicts
- Careful airway management
- Document neurologic deficits prior to regional techniques
- May present with massive hemoptysis and require emergency lung isolation
Takayasu’s Arteritis
Overview
- Takayasu’s arteritis (TAK) is a rare large vessel vasculitis most commonly seen in young Asian women, resulting in granulomatous inflammation of the aorta and its large branches.
- Patients can present with decreased or absent pulses, hypertension, discrepant pressure readings between arms and/or lower limbs, and claudication.
- Complications include aortic regurgitation (AR), pulmonary thrombosis and hypertension, cerebral infarction, blindness, and limb ischaemia.
- Imaging of arteries is important to aid diagnosis and monitor disease activity. Angiography remains the gold standard; however, CT modalities (CT angiography, CT PET) and MRI are more commonly used.
- Echocardiography is used as a non-invasive assessment of aortic root dilatation, pulmonary hypertension, and central hypertension.
- Treatment includes high-dose glucocorticoids with immunosuppressive therapies for remission induction and biological agents. Endovascular procedures or bypass surgery are reserved for the treatment of critical arterial stenoses, ideally performed when inflammation is controlled.
Considerations
Neurological:
- Carotid involvement (dizziness & syncope on neck extension and bruit) = Neutral head position, maintain CPP
Cardiovascular:
- Hypertension: Maintain blood pressure at pre-op level (too high = aneurysm rupture, too low = inadequate CPP)
- Cardiac dysfunction: Check echocardiography
- Pulmonary Arterial Hypertension (PAH): Avoid factors that worsen it
Renal/Electrolytes:
- Check renal function and electrolytes
Monitoring:
- NIBP: Upper and lower limb if >20mmHg discrepancy, monitor both intraoperatively
- Sats probe: Can also be used on hand and foot
- A-line: Only if really necessary (vascular injury)
- If GA, consider cerebral monitoring
General Anesthesia (GA) vs. Regional Anesthesia:
- Epidural is better than spinal to avoid precipitous drops in BP (give fluid boluses as necessary, caution with vasopressors)
- Epidurals have advantages over GA where suitable: haemodynamic stability, good post-op pain relief, avoidance of intubation response, and neck manipulation
Drugs:
- Steroid supplementation
Associated Conditions:
- Rheumatoid arthritis (RA) and Ankylosing spondylitis
IV Access:
- Potentially difficult
Links
- Vascular physiology
- Connective tissue and autoimmune disease
- Vascular surgery
- Upper and lower limb vascular surgery
References:
- Chetcuti, S., Jones, R., & Varley, J. (2016). Heritable connective tissue diseases, vasculitides, and the anaesthetist. BJA Education, 16(9), 316-322. https://doi.org/10.1093/bjaed/mkw016
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “3fcdb4dd-23d5-402b-905a-820f17f7737d”



