- Upper and Lower Limb Vascular Surgery
- Conduct of Anaesthesia for Peripheral Revascularization
- Anaesthetic Techniques
- Supplemental Measures
{}
Upper and Lower Limb Vascular Surgery
Critical Limb Ischaemia
- Up to 15% of patients with asymptomatic peripheral arterial disease (PAD) will develop symptoms of intermittent claudication (IC) or critical limb ischaemia (CLI). A further 1-3% of these patients will require major limb amputation within a 5-year period.
- IC is characterized by aching muscle pain brought on by exercise and relieved by rest. The underlying cause is a reduction in tissue oxygen delivery due to decreased blood flow and increased tissue oxygen demand during exercise. PAD most commonly affects the superficial femoral artery, leading to calf claudication pain.
- Ischaemic rest pain and tissue loss (ulcers or gangrene) are key signs of CLI. Intervention should be considered when conservative measures have failed and symptoms become debilitating and lifestyle-restricting.
- The surgical goals are to relieve ischaemic rest pain, heal ischaemic ulcers, prevent limb loss, improve quality of life, and prolong survival.
Natural History of Atherosclerotic Lower Extremity PAD Syndromes
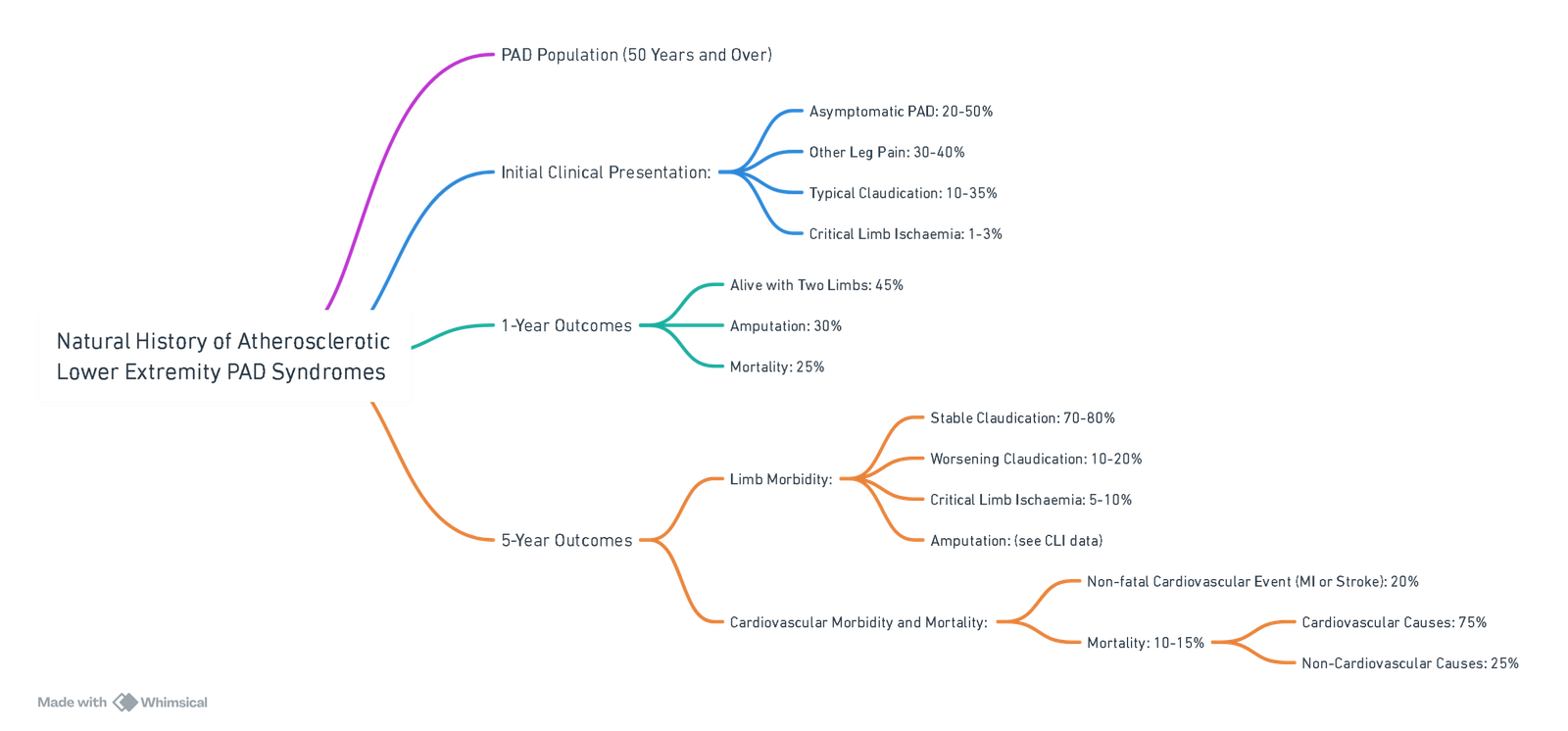
View or edit this diagram in Whimsical.
Conduct of Anaesthesia for Peripheral Revascularization
Procedure
- Grafts:
- Long saphenous vein or Gore-Tex® graft.
- Duration:
- 1–6 hours.
- Pain:
- Severe (+++).
- Position:
- Supine.
- Blood Loss:
- Typically 500–1000 mL; cross-match 2 units.
- Types of Bypass:
- Femoro-popliteal bypass: Femoral to above-knee popliteal artery.
- Femoro-distal bypass: Femoral to anterior or posterior tibial artery.
- Femoro-femoral crossover graft: From one femoral artery to another.
Preoperative Management
- Treatment Goals for Modifiable Risk Factors (ADA/EASD Guidelines):
- Glycaemic Control:
- HbA1C < 7% (ADA) or < 6.5% (EASD) in patients without cardiovascular disease.
- HbA1C 7–7.5% in patients with cardiovascular disease or life expectancy < 10 years.
- LDL-Cholesterol:
- < 1.8 mmol/L.
- Smoking:
- Complete nicotine cessation.
- Arterial Pressure:
- < 130/80 mm Hg.
- Anti-platelets:
- Aspirin or clopidogrel.
- Glycaemic Control:
Intraoperative Management
IV Access
- Ensure at least one large-bore IV cannula (14G or 16G).
- Insert an arterial line for long cases (>2 hours), if haemodynamic instability is expected or in sicker patients.
Monitoring
- Standard monitoring with:
- 5-lead ECG.
- Central venous pressure monitoring (rarely required)
Goals
- Oxygenation: Maintain optimum oxygenation.
- Haemodynamic Stability:
- Avoid tachycardia.
- Maintain mean arterial pressure (MAP) within 20% of baseline.
- Anticipate reperfusion hypotension.
- Normothermia: Maintain normal body temperature.
- Normovolaemia and Oxygen-Carrying Capacity: Prepare for significant blood loss.
- Pain Management:
- Use regional anaesthesia or patient-controlled analgesia (PCA).
Anaesthetic Techniques
- General Anaesthesia (GA):
- Techniques:
- Endotracheal tube (ETT) with intermittent positive-pressure ventilation (IPPV).
- Laryngeal mask airway (LMA) with spontaneous ventilation (SV).
- Femoral nerve block can be performed perioperatively.
- Adjuncts:
- Volatile and opioid preconditioning.
- Single-shot spinal anaesthesia may offer good operating conditions and post-operative pain relief, but may lack sufficient duration. Adding intrathecal clonidine or diamorphine may help.
- Techniques:
- Regional Anaesthesia:
- Combined spinal/epidural anaesthesia is preferred.
- Benefits:
- Decreases respiratory morbidity and postoperative cognitive dysfunction (POCD).
- Provides good postoperative analgesia and reduces stress response.
- Considerations:
- Contraindicated in coagulopathy.
- Use caution with dual antiplatelet therapy (DAPT).
- May be difficult for long procedures.
- Consider epidural diamorphine (2–3 mg) and start an infusion of 0.25% bupivacaine at 5–10 mL/hr.
Supplemental Measures
- Oxygen: Always provide supplemental oxygen. Use propofol TCI for sedation if required.
- Heparin:
- Administer 3000–5000 U before clamping.
- Reverse with protamine (0.5–1 mg/100 U of heparin) after surgery.
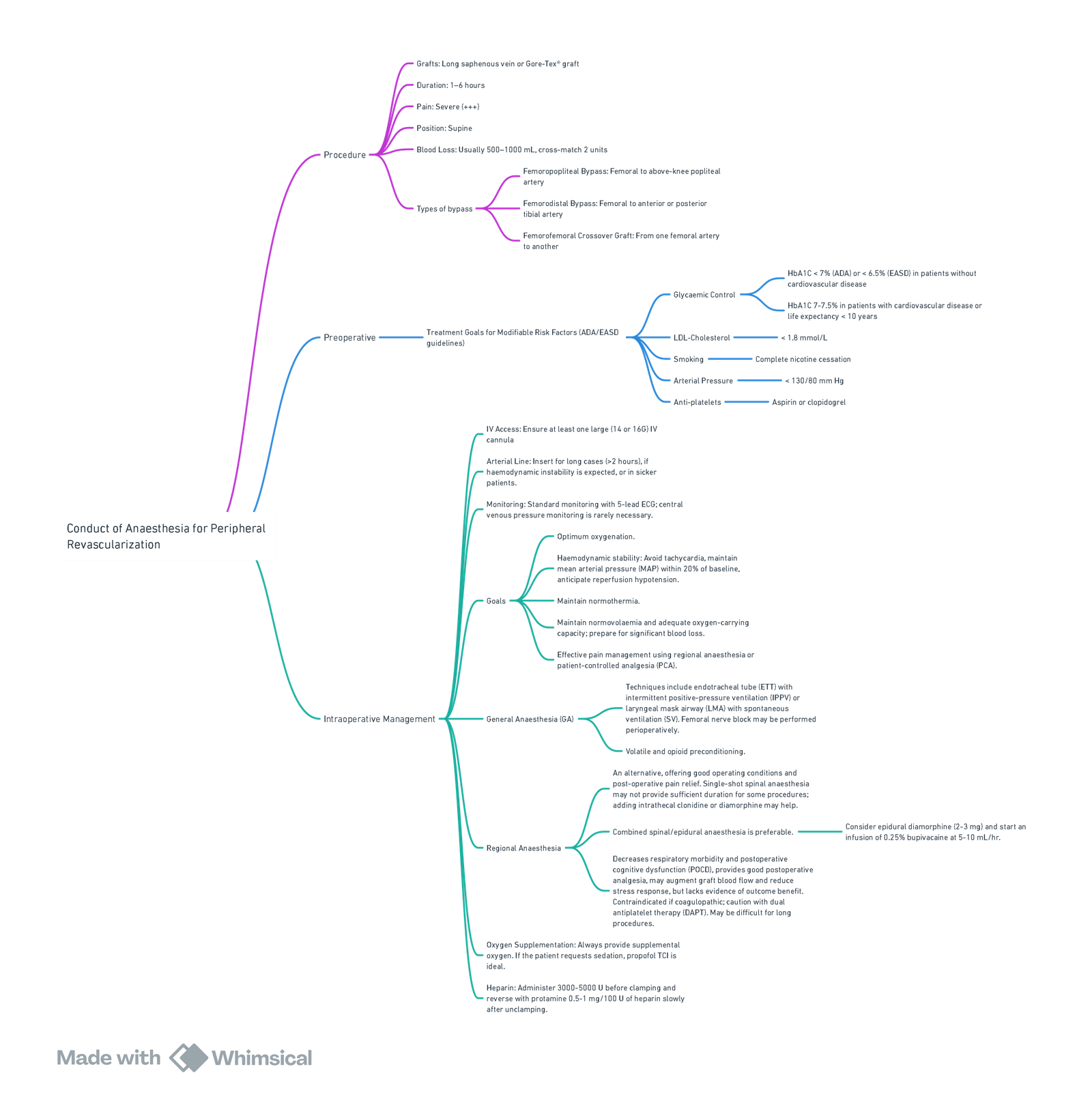
View or edit this diagram in Whimsical.
Links
- Vascular physiology
- Peripheral Vascular Disease (PVD) and Risk Stratification
- Off Pump CABG
- Cath lab anaesthesia
- Coronary artery bypass surgery (CABG)
References:
- Fraser, K. and Raju, I. (2015). Anaesthesia for lower limb revascularization surgery. BJA Education, 15(5), 225-230. https://doi.org/10.1093/bjaceaccp/mku042
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
Summaries:
Lower limb amputation
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “bb87e57b-26fe-4101-8af4-c2aebf8689b7”



