{}
Procedures
| Operation | Description | Time (min) | Pain | Position | Blood loss/X-match | Notes |
|---|---|---|---|---|---|---|
| Colposuspension | Abdominal procedure for stress incontinence | 40 | +++ | Supine | G&S | ETT, IPPV |
| Cone biopsy/LLETZ | Removal of the terminal part of the cervix through the vagina | 30 | ++ | Supine | G&S | May bleed post-operatively. LMA, SV |
| Laparotomy, investigative | Abdominal assessment of pelvic mass | 120 | ++++ | Supine | 2U | Ovarian tumours may be adherent to adjacent structures. Potentially large blood loss |
| Myomectomy | Abdominal excision of fibroids from uterus | 60 | +++ | Supine | G&S | Blood loss may be greater than expected. ETT, IPPV |
| Oophorectomy | Removal of ovaries | 40 | +++ | Supine | G&S | ETT, IPPV |
| Repair, anterior | Repair of anterior vaginal wall | 20 | ++ | Lithotomy | Nil | Often combined with vaginal hysterectomy. LMA ± caudal |
| Repair, posterior | Repair of posterior vaginal wall | 20 | ++ | Lithotomy | Nil | Often combined with vaginal hysterectomy. LMA ± caudal |
| Sacrocolpopexy | Abdominal repair of vault prolapse | 60 | +++ | Supine | G&S | ETT, IPPV |
| Sacrospinous fixation | Vaginal operation for vault prolapse | 40 | +++ | Lithotomy | Nil | |
| Shirodkar suture | Insertion of suture around cervix to prevent recurrent miscarriage | 20 | ++ | Lithotomy | Nil | May need antacid prophylaxis |
| Thermoablation | Thermal obliteration of endometrium | 20 | ++ | Lithotomy | Nil | May require opioids |
| TCRE | Endoscopic resection of endometrium | 30 | ++ | Lithotomy | Nil | Systemic absorption of water may occur from the glycine solution. Treat as for TURP syndrome |
| Vulvectomy, simple | Excision of vulva | 90 | +++ | Lithotomy | G&S | |
| Vulvectomy, radical | Excision of vulva and lymph nodes | 150 | ++++ | Lithotomy | 2U | Epidural analgesia recommended |
Molar Pregnancy
Overview
- Molar pregnancy (hydatidiform mole) represents placentas with abnormally developed chorionic villi. It is one of the four groups of Gestational Trophoblastic Disease, ranging from molar pregnancy to choriocarcinoma.
- The defect occurs during fertilization, where the ovum is fertilized by more than one sperm.
- Classification:
- Partial mole: Contains placenta and some fetal parts.
- Complete mole: Contains only grape-like placental tissue.
- Incidence: Varies geographically, ranging from 1:2500 in the USA to 1:200 in some Asian countries.
- Risk Factors:
- Age: Less than 20 and more than 35 years.
- History of miscarriage.
- Previous history of molar pregnancy (1-2%).
- Race: More common in South Asians and Africans.
- Diet: Low in vitamin A, folic acid, and protein.
Clinical Presentation
- Vaginal bleeding
- Uterus size greater than gestational age
- Hyperemesis gravidarum
- Symptoms of pre-eclampsia
- Hyperthyroidism
- Respiratory compromise or ARDS
- Theca lutein cysts
Symptom Variability
- Presenting symptoms can range from vaginal bleeding to clinical hyperthyroidism complicated by high output cardiac failure.
- Thorough pre-operative assessment of thyroid function and cardiopulmonary reserve is essential.
- Key concerns for the anesthetist include thyrotoxicosis, acute cardiopulmonary distress, and bleeding.
Management
- Surgical:
- Termination of pregnancy by suction curettage or hysterectomy for those beyond childbearing age.
- Medical:
- Methotrexate.
Hyperthyroidism in Molar Pregnancy
- Clinical hyperthyroidism complicates 7% of molar pregnancies, while biochemical hyperthyroidism can be as high as 50%.
- Presentation varies from no symptoms to thyroid storm.
- Pathophysiology:
- hCG stimulates TSH in molar pregnancy.
- Hyperthyroidism is linked to high circulating hCG levels.
- Management:
- Start anti-thyroid medications before anesthesia for stable patients with clinical hyperthyroidism.
- Emergency cases with bleeding can be managed with beta-blockers and steroids to prevent thyroid storm.
- Thyroid Storm:
- Symptoms include tachycardia, arrhythmias, cardiovascular collapse, coma, and death.
- Managed by supportive measures, administration of beta-blockers, steroids, and anti-thyroid medications.
Drugs for Thyroid Management
Antithyroid Agents
| Drug | Typical Adult Dose | Action |
|---|---|---|
| propylthiouracil (PTU) | 1,200–1,500 mg/day, given in 200–250 mg increments PO or via gastric tube | Prevents production of more T4 and T3 in the thyroid, and blocks the conversion of T4 to T3 outside the thyroid. |
| methimazole (Tapazole) | 120 mg given in 20 mg increments PO or via gastric tube | Prevents production of more thyroid hormone. |
Iodides
| Drug | Typical Adult Dose | Action |
|---|---|---|
| Lugol’s solution | 10 drops twice a day PO or via gastric tube | Blocks release of stored thyroid hormone from thyroid gland. |
| saturated solution of potassium iodide (Pima, SSKI) | 8 drops every 6 hours PO or via gastric tube | Blocks release of stored thyroid hormone from thyroid gland. |
Glucocorticoids
| Drug | Typical Adult Dose | Action |
|---|---|---|
| dexamethasone (Decadron) | 2 mg every 6 hours, PO or IV | Blocks conversion of T4 to T3. |
| hydrocortisone | 100 mg IV every 8 hours | Blocks conversion of T4 to T3. |
Beta-blockers
| Drug | Typical Adult Dose | Action |
|---|---|---|
| propranolol (Inderal) | 1 mg/min IV as required, then 60–80 mg every 4 hours PO or via gastric tube | Reduces symptoms (tachycardia, tremor, restlessness) caused by a heightened response to catecholamines; blocks conversion of T4 to T3. |
| esmolol (Brevibloc Injection) | 500 mcg/kg/min for 1 minute, then 50–100 mcg/kg/min for 4 minutes | Reduces symptoms (tachycardia, tremor, restlessness) caused by a heightened response to catecholamines; blocks conversion of T4 to T3. |
Acute Cardiopulmonary Distress
- Typically follows evacuation of the molar pregnancy in patients with very high hCG levels.
- Seen in 27% of patients with uterus size greater than 16 weeks.
- Symptoms appear 4-12 hours post-evacuation.
- Cause: Embolization of trophoblastic tissue causing high pulmonary pressures.
- Management: Support cardiac and respiratory systems, maintain oxygenation, mechanical ventilation if necessary. Condition usually resolves by 72 hours.
Bleeding and Anaemia
- Bleeding can be occult or massive.
- Patients may present fluid depleted or with high output cardiac failure due to anaemia.
- Challenges include fluid management to avoid overloading.
- During Suction Curettage:
- Potential for blood loss, uterine perforation, and massive transfusion.
Anaesthesia for Molar Pregnancy
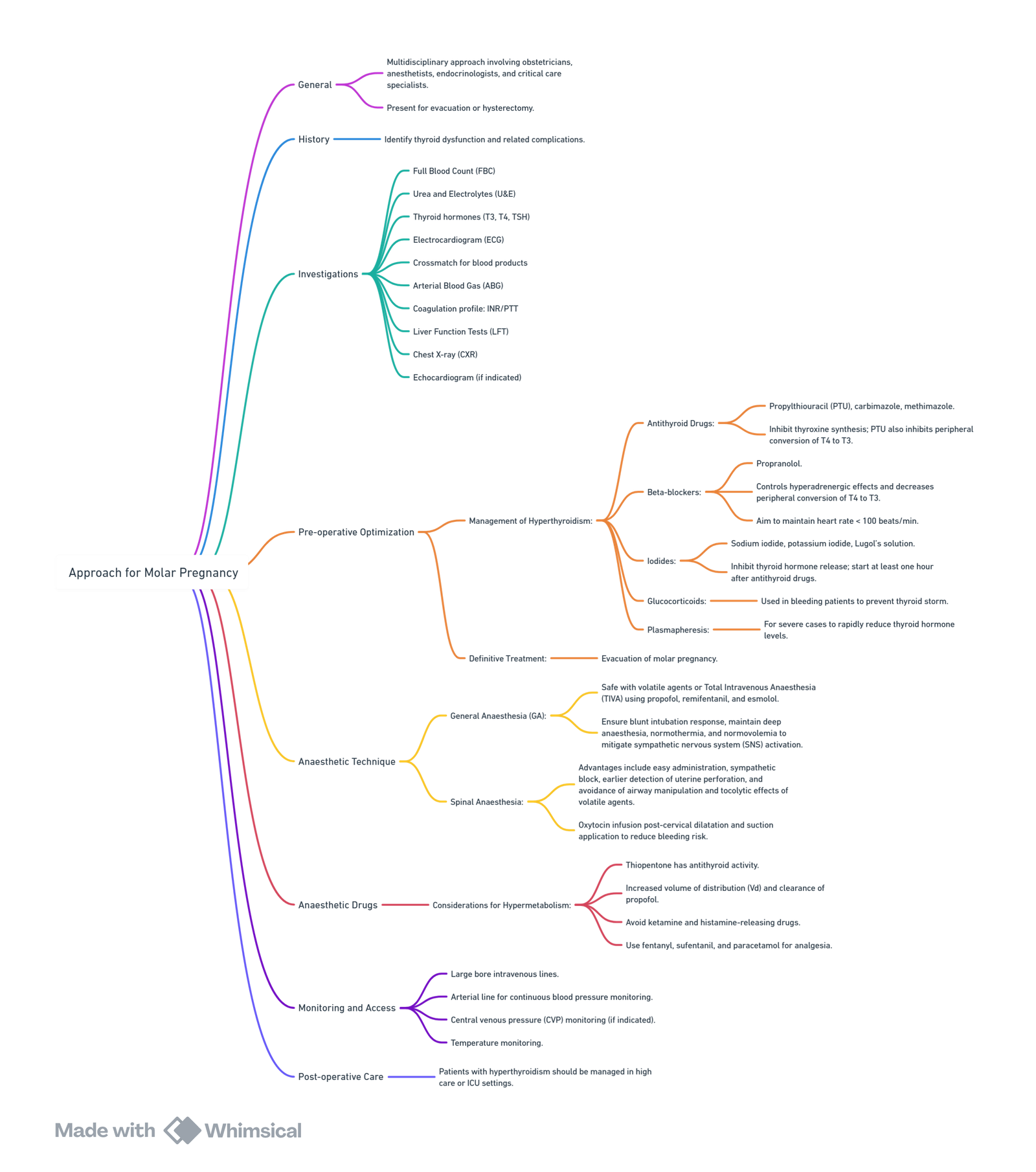
View or edit this diagram in Whimsical.
Summary of Management of Patients with Molar Pregnancy
- Communication: Essential between the obstetrician and anaesthetist for adequate patient preparation and workup.
- Anaesthetic Workup: Identify complications and avoid intraoperative and postoperative adverse outcomes.
- Baseline investigations: FBC, U&E, TFT, CXR, and baseline ABG.
- Additional investigations as needed based on patient condition.
- Blood Availability: Ensure blood is available for major bleeding.
- Postoperative Care: Patients with thyrotoxicosis or cardiopulmonary compromise need high care or ICU.
- Anaesthetic Technique: General anaesthesia is commonly preferred; regional anaesthesia may be used in stable patients with low risk of bleeding.
Ovarian Hyperstimulation Syndrome (OHSS)
Pathophysiology
- OHSS is a rare and exaggerated response to ovulation induction therapy, usually associated with exogenous gonadotropin stimulation.
- It is a self-limiting disorder that resolves spontaneously within days.
- The spectrum of presentation ranges from mild disease needing observation to severe disease requiring ICU admission.
- The hallmark is an increase in capillary permeability resulting in fluid shift from the intravascular space to the third space.
- Vascular endothelial growth factor (VEGF) is most likely involved in OHSS, but other factors such as interleukin-1, interleukin-6, angiotensin II, and platelet-derived growth factor may also play a role.
Risk Factors
- Young age
- Low body weight
- Polycystic ovarian syndrome
- High doses of exogenous gonadotropins
- Previous episodes of OHSS
Clinical Features
- Symptoms: nausea, vomiting, diarrhoea, abdominal distension, ascites, pleural effusion, pericardial effusion, and hemodynamic instability.
- Hypotension results from fluid extravasation.
- Haemoconcentration with inactivity increases the risk of thromboembolism.
- Classification:
- Mild: abdominal bloating
- Moderate: nausea and moderate abdominal pain
- Severe: oliguria, ARDS, and thromboembolism
- Life-threatening complications: renal failure, adult respiratory distress syndrome, cardiovascular instability, bleeding into ovarian cysts, and thromboembolism.
- Patients with severe OHSS may present needing laparotomy for bleeding ovarian cyst or torsion, presenting an anaesthetic challenge.
Anaesthetic Concerns and Considerations
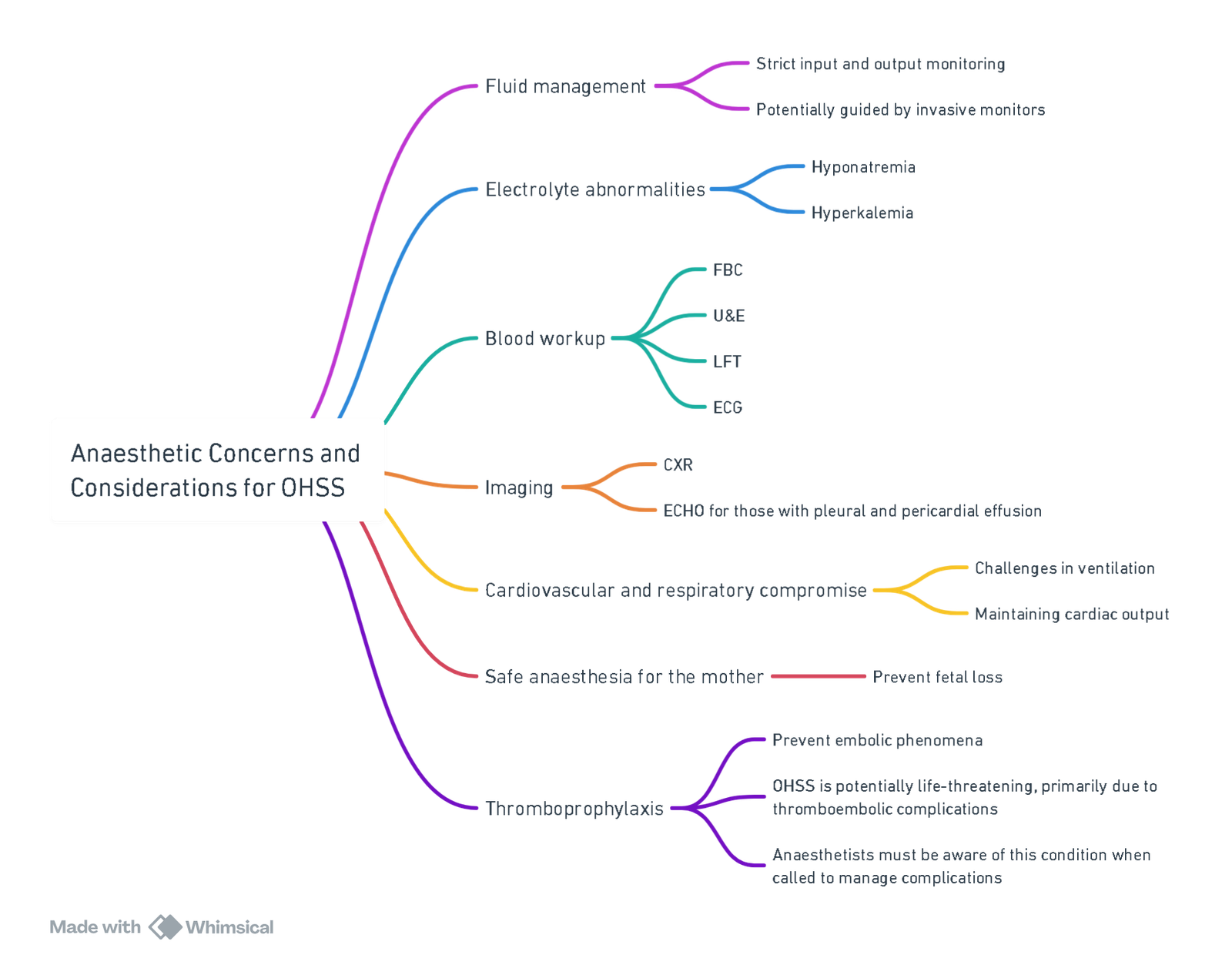
View or edit this diagram in Whimsical.
Ovarian Torsion
Pathophysiology
- Ovarian torsion involves partial or complete rotation of the ovary around its vascular pedicle or axis.
- Complete torsion causes venous and lymphatic blockage, leading to stasis, venous congestion, hemorrhage, and necrosis.
- The cyst becomes tense and may rupture.
Presentation
- Patients present with severe abdominal pain.
- Higher incidence during pregnancy (22.7%) compared to non-pregnant patients (6.1%).
- Pregnancy increases the risk of ovarian torsion by a factor of 5.
- Ovarian torsion surgery is one of the three most common surgeries during pregnancy.
- Surgery during pregnancy should be avoided unless urgent.
- Understanding physiological and pharmacological changes across trimesters is crucial for safe anaesthesia.
Anaesthetic Goals
- Optimize and maintain normal maternal physiological function.
- Optimize and maintain utero-placental blood flow and oxygen delivery.
- Avoid drugs with teratogenic side effects.
- Prefer regional anaesthesia to avoid drug transfer to the mother and airway manipulation.
- Reduce sympathetic stimulation to prevent preterm labor.
- Prevent awareness during anaesthesia.
Anaesthetic Concerns and Considerations
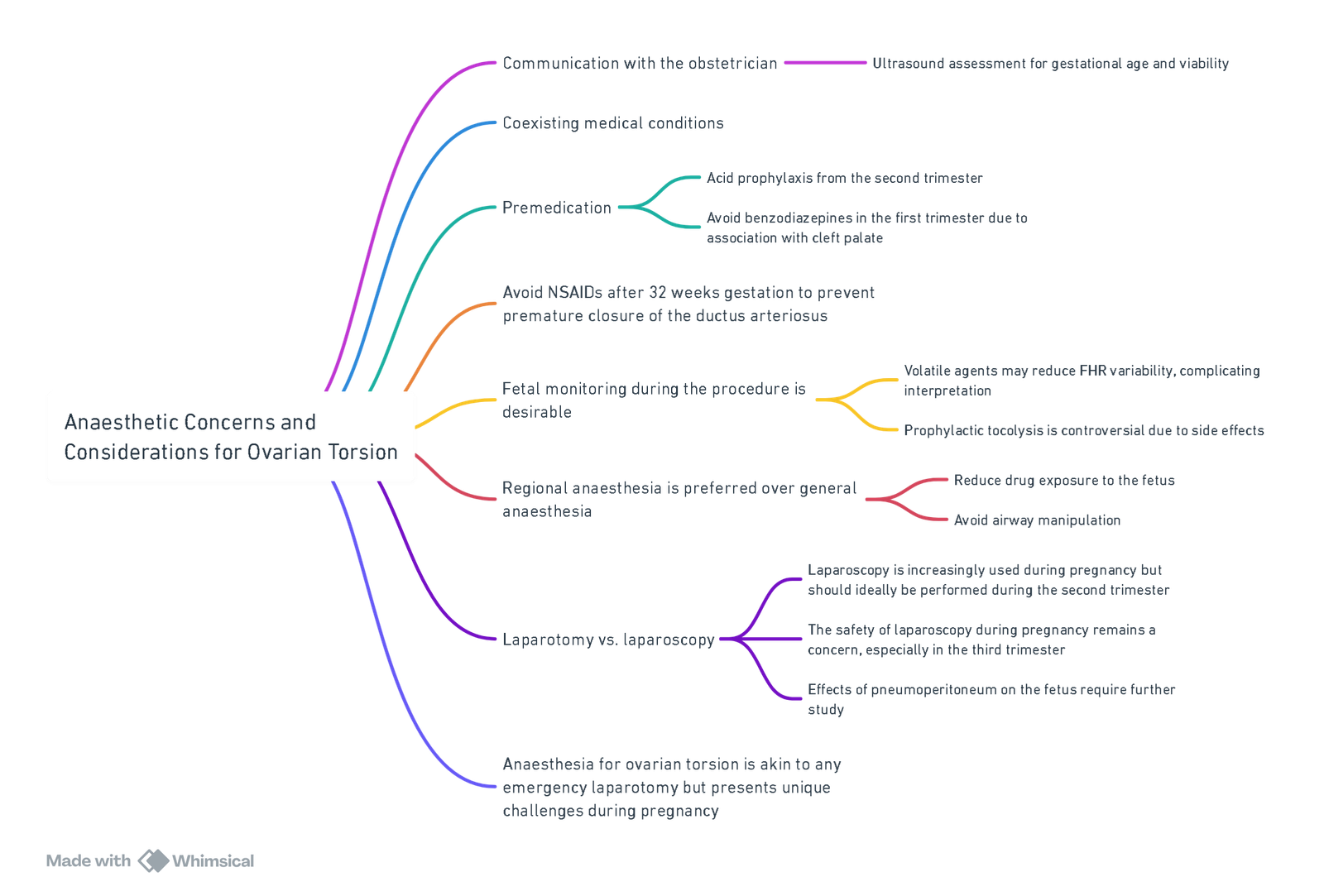
View or edit this diagram in Whimsical.
Cervical Incompetence
Presentation
- Patients present for modified Shirodkar or McDonald suture, both done transvaginally at 14-18 weeks.
- These procedures increase fetal survival from 20% to 89%.
- Patients with cervical incompetence have painless, recurrent second-trimester miscarriages.
- In cases with bulging membranes, there is a significant concern about rupturing the membranes during the procedure.
Anaesthetic Considerations
- Prophylactic procedures: Regional anaesthesia is preferred. A small RCT found no difference in postoperative oxytocin levels and uterine activity between spinals and general anaesthesia for prophylactic cerclage.
- After 20 weeks, aorto-caval compression decreases utero-placental perfusion.
- Emergency procedures with bulging membranes: General anaesthesia may be preferred to decrease intra-abdominal pressure and reduce the risk of rupturing membranes.
- Tocolysis should be considered if the membranes are bulging.
Links
- Non obstetric surgery
- Obstetric haemorrhage
- Molar pregnancy
- Ovarian hyperstimulation
- Maternal conditions
References:
- Lurain, J. R. (2011). “Gestational trophoblastic disease II: classification and management of gestational trophoblastic neoplasia.” American Journal of Obstetrics and Gynecology 204(1): 11-18
- Swaminathan S, James RA, Chandran R, Joshi R. Anaesthetic Implications of Severe Hyperthyroidism Secondary to Molar Pregnancy: A Case Report and Review of Literature. Anesth Essays Res. 2017 Oct-Dec;11(4):1115-1117. doi: 10.4103/aer.AER_38_17. PMID: 29284889; PMCID: PMC5735464.
- Namavar Jahromi B MD, Parsanezhad ME MD, Shomali Z MD, Bakhshai P MD, Alborzi M MD, Moin Vaziri N MD PhD, Anvar Z PhD. Ovarian Hyperstimulation Syndrome: A Narrative Review of Its Pathophysiology, Risk Factors, Prevention, Classification, and Management. Iran J Med Sci. 2018 May;43(3):248-260. PMID: 29892142; PMCID: PMC5993897.
- Chandra, A., Thakur, V. S., Duggal, R., & Pawar, S. J. (2015). Hydatiform mole and its anesthetic implications. Medical Journal of Dr. D.Y. Patil University, 8(6), 841. https://doi.org/10.4103/0975-2870.169923
- Anaesthesia for gynaecological emergencies Dr Nthatheni Madima. Wits refresher 2013
- Molar pregnancies with a focus on the thyroid. Dr F BhamWits refresher 2017
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “2d4e6058-26aa-4a85-9c9e-514a90e183ef”



