- Summary of Approach to Cardiac Patient for Non Cardiac Surgery
- Risk Assessment
- Conduct of Anaesthesia
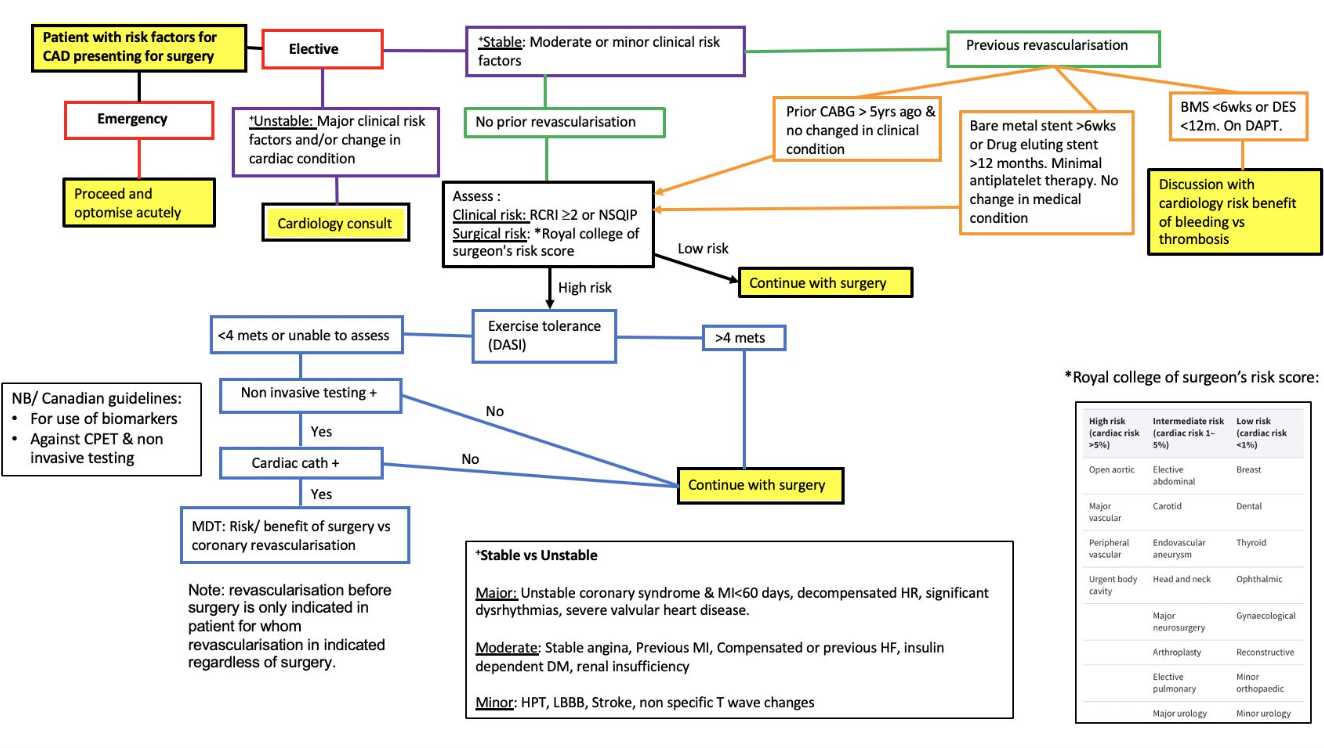
- SA Perioperative Guideline Summary
- Recommendations
- Role of Non-Invasive Testing
- Self-Reported Functional Capacity
- Resting Echocardiography, Coronary Computed Tomographic Angiography, Pharmacological Stress Echocardiography, and Radionuclide Imaging
- Exercise Stress Testing and Cardiopulmonary Exercise Testing
- The Role of Natriuretic Peptide Testing in Risk Stratification
- Preoperative NP Thresholds for Predicting 30-Day Mortality and Non-Fatal Myocardial Infarction
- Troponin
- Medication Management
- SA Flow for Cardiac Risk and ProBNP
- Major Changes in Perioperative Cardiovascular Management for Noncardiac Surgery (2024)
- Definitions of Surgical Timing and Surgical Risk
- Stepwise Approach to Perioperative Cardiac Assessment for Patients with Cardiovascular Risk Factors Scheduled for Non-Cardiac Surgery (NCS)
- 1. Initial Assessment
- 2. Management of Acute Cardiac Conditions
- 3. Estimation of Perioperative Risk
- 4. Risk Modification and Testing for Elevated Risk Patients
- 5. Functional Capacity Evaluation
- 6. Preoperative Biomarker Risk Assessment
- 7. Preoperative Testing for Abnormal Biomarkers
- 8. Postoperative Surveillance
- Summary of Recommendations for Specific Conditions from 2024 Guidelines
- Coronary Revascularization
- Hypertension and Perioperative Blood Pressure Management
- Heart Failure
- Pulmonary Hypertension (PH)
- Congenital Heart Disease (CHD) Management
- Left Ventricular Assist Devices (LVAD)
- Aortic Stenosis (AS)
- Mitral Stenosis (MS)
- Chronic Aortic and Mitral Regurgitation
- Previous Transcatheter Valve Repair
- Atrial Fibrillation (AF)
- Preoperative Management of Cardiovascular Implantable Electronic Devices (CIED)
- Stroke or Transient Ischemic Attack (TIA)
- Obstructive Sleep Apnea (OSA)
- Perioperative Medication Recommendations
- Beta Blockers
- Statins
- Renin-Angiotensin-Aldosterone System Inhibitors (RAASi)
- Alpha-2 Receptor Agonists
- Antiplatelet Therapy and Timing of Noncardiac Surgery (NCS) in Patients with Coronary Artery Disease (CAD)
- Oral Anticoagulants (OAC) Management
- Optimal Timing of Elective or Time-Sensitive NCS for Prior PCI Requiring Management of DAPT
- Systematic Work-up and Treatment of Peri-Operative Myocardial Injury/Infarction
- Peri-Operative Approach to Patients with Ventricular Assist Devices Undergoing Non-Cardiac Surgery
- Management of Oral Anticoagulation Therapy in Patients Undergoing Non-Cardiac Surgery (NCS)
- Bridging with Intravenous Antiplatelet Agents for Non-Cardiac Surgery (NCS)
- Perioperative Risk Assessment and Postoperative Monitoring for Patients Undergoing Non-Cardiac Surgery
- Management of Interventions Targeting the Prevention of Perioperative Cardiac Events
- CAD for Non-Cardiac Surgery Recommendations
- Paediatric Considerations
{}
Summary of Approach to Cardiac Patient for Non Cardiac Surgery
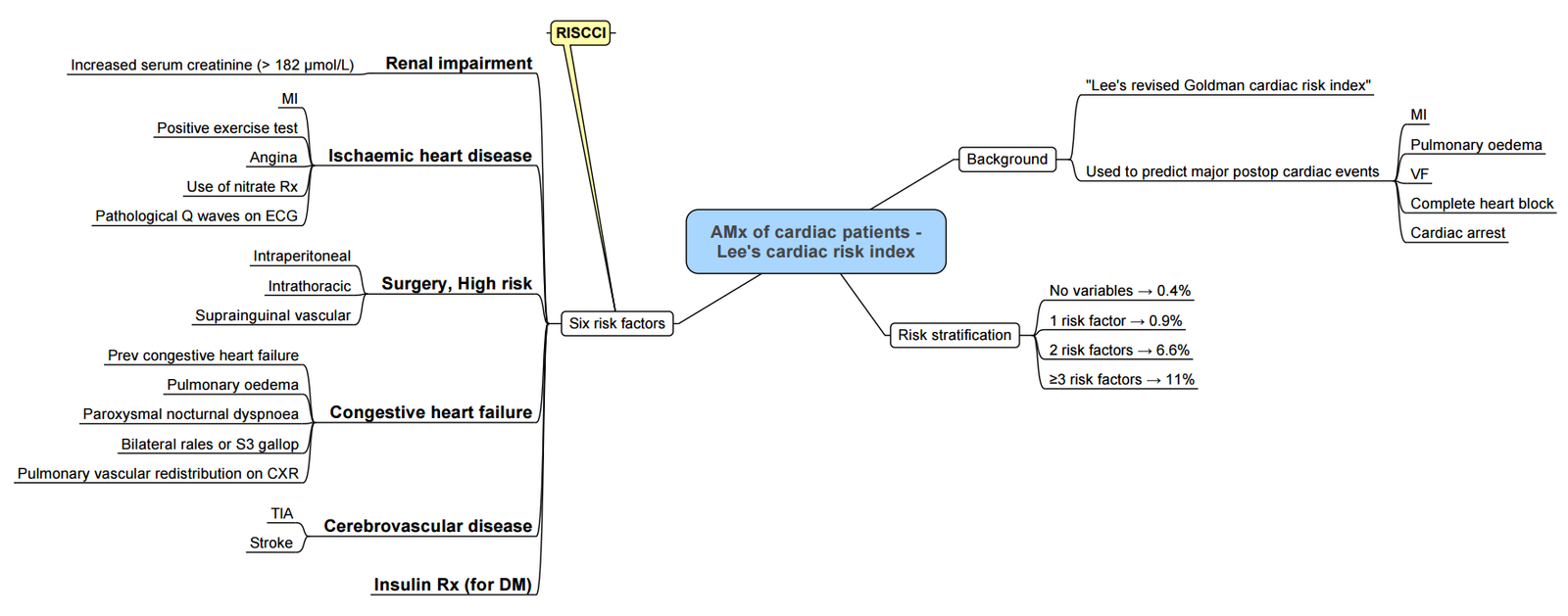
Risk Assessment
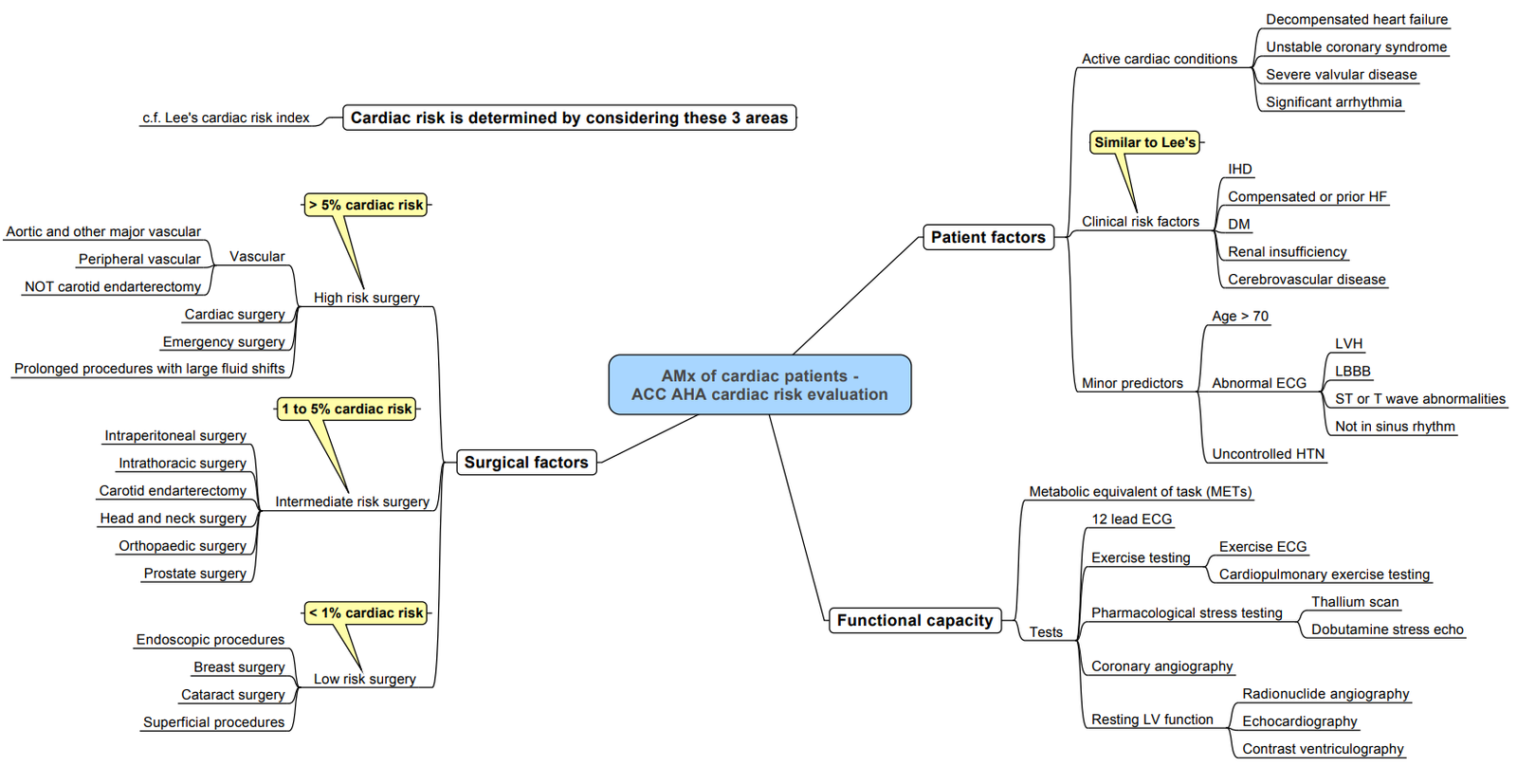
Risk Scoring Systems
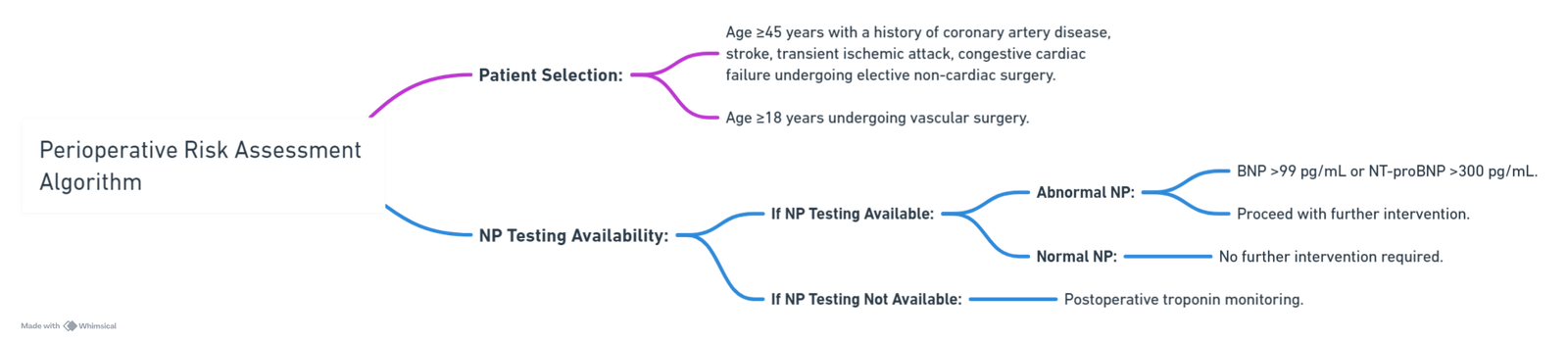
Perioperative Risk Assessment and Monitoring Algorithm (SA 2021)
- Perioperative Risk Assessment
- Target Population:
- Patients aged ≥45 years with a history of:
- Coronary artery disease.
- Stroke or transient ischaemic attack (TIA).
- Congestive cardiac failure.
- Patients aged ≥18 years undergoing vascular surgery.
- Patients aged ≥45 years with a history of:
- Procedure: Elective non-cardiac surgery.
- Decision Point: Is NP (Natriuretic Peptide) Testing Available?
- If NP Testing is Not Available:
- Proceed to Postoperative Troponin Monitoring.
- If NP Testing is Available:
- Perform NP testing to measure:
- BNP (B-type natriuretic peptide) levels. NT-proBNP (N-terminal prohormone B-type natriuretic peptide) levels.
- Perform NP testing to measure:
- NP Test Results Interpretation
- NP Abnormal:
- BNP > 99 pg/mL or NT-proBNP > 300 pg/mL.
- Action: Proceed to Postoperative Troponin Monitoring.
- NP Normal:
- Action: No further intervention is required.
Lee’s Revised Cardiac Risk Index (RCRI)
- Pro: Most validated, moderate discrimination
- Con: Some risks missing (AS, PH)
Modalities for risk Assessment
Functional Capacity
- METS (self-reported) do not predict perioperative cardiac risk (shown in multiple studies)
- DASI <34 = predicts increased 30-day mortality, MINS, and MI
- 1 MET
- Watching television
- Eating, dressing
- Walking on level ground at <6 km/h
- Walking 1-2 blocks on level ground
- Doing light housework (e.g., dusting)
- 4 METs
- Climbing a flight of stairs/Hill
- Walking on level ground > 6 km/h
- Dancing, playing golf
- Doing heavy chores (e.g., scrubbing floors)
-
10 METs
- Playing strenuous sports (e.g., tennis)
Duke Activity Status Index (DASI) Questionnaire
| Questionnaire Item | Points |
|---|---|
| Can you take care of yourself, that is, eat, dress, bathe, or use the toilet? | 2.75 |
| Can you walk indoors, such as around your house? | 1.75 |
| Can you walk 200 yards on level ground? | 2.75 |
| Can you climb a flight of stairs or walk up a hill? | 5.00 |
| Can you run a short distance? | 8.00 |
| Can you do light work around the house like dusting or washing dishes? | 2.70 |
| Can you do moderate work around the house like vacuuming, sweeping floors, or carrying groceries? | 3.50 |
| Can you do heavy work around the house like scrubbing floors or lifting or moving heavy furniture? | 8.00 |
| Can you do yard work like raking leaves, weeding, or pushing a power mower? | 4.50 |
| Can you have sexual relations? | 5.25 |
| Can you participate in moderate recreational activities like golf, bowling, dancing, doubles tennis, or throwing a ball? | 6.00 |
| Can you participate in strenuous sports like swimming, singles tennis, football, basketball, or skiing? | 7.50 |
Cardiac Biomarker
- NT-proBNP: Able to predict patients at low risk of MACE
| Test Result | Risk Estimate (%) | 95% CI for the Risk Estimate |
|---|---|---|
| NT-proBNP < 300 ng/L or BNP < 92 mg/L | 4.9 | 3.9%-6.1% |
| NT-proBNP ≥ 300 ng/L or BNP ≥ 92 mg/L | 21.8 | 19.0%-24.8% |
- CCS guidelines: Perform Pro BNP on high-risk patients (>5% risk of MACE post-op):
- Older than 65 years
- RCRI>1
- Age 45-65 with CVS disease
Resting Echo
- CCS guidelines: Not for routine use (no benefit in addition to BNP & RCRI)
- Use if patient may have:
- AS/MS
- HOCM
- Severe PH
Coronary Computed Tomographic Angiography (CCTA)
- Overestimates
- CCS guidelines suggest against use
Cardiopulmonary Exercise Testing (CPET)
- Weak predictor for long-term post-op mortality
- Cost ineffective and inconvenient for patients
- CCS guidelines evaluated against CPET for risk stratification, whereas AHA/ACC use it if METS<4 and it will influence care or decision making (can be used in risk prediction scores)
Pharmacological Stress Testing
- Poor quality evidence
- Not currently advised by CCS, AHA/ACC suggest use if unable to conduct CPET
Surgical risk and Timing
| Category | Surgical Procedures |
|---|---|
| Low Surgical Risk (<1%) | – Breast – Dental – Endocrine: thyroid – Eye – Gynaecological: minor – Orthopaedic minor (meniscectomy) – Reconstructive – Superficial surgery – Urological minor (transurethral resection of the prostate) – VATS minor lung resection |
| Intermediate Surgical Risk (1-5%) | – Carotid asymptomatic (CEA or CAS) – Carotid symptomatic (CEA) – Endovascular aortic aneurysm repair – Head or neck surgery – Intraperitoneal: splenectomy, hiatal hernia repair, cholecystectomy – Intrathoracic: non-major – Neurological or orthopaedic: major (hip and spine surgery) – Peripheral arterial angioplasty – Renal transplants – Urological or gynaecological: major |
| High Surgical Risk (>5%) | – Adrenal resection – Aortic and major vascular surgery – Carotid symptomatic (CAS) – Duodenal-pancreatic surgery – Liver resection, bile duct surgery – Oesophagectomy – Open lower limb revascularization for acute limb ischaemia or amputation – Pneumonectomy (VATS or open surgery) – Pulmonary or liver transplant – Repair of perforated bowel – Total cystectomy |
Timing Categories
- Immediate: Surgery/intervention should be performed without any delay to save life or organ function.
- Urgent: Surgery/intervention should be performed without unnecessary delay to save life, limb, or organ function.
- Time-sensitive: Surgery/intervention should be performed as soon as possible as there is a time-dependent risk of losing limb or organ function, or increased risk of complications. Cancer surgery is typically time-sensitive, as is carotid surgery to prevent stroke in a symptomatic case. The time window for time-sensitive surgery will vary depending on the underlying disease.
- Elective: Surgery/intervention can be performed electively (not further defined) without significant risk of losing limb, organ function, or increased risks of complications.
Conduct of Anaesthesia
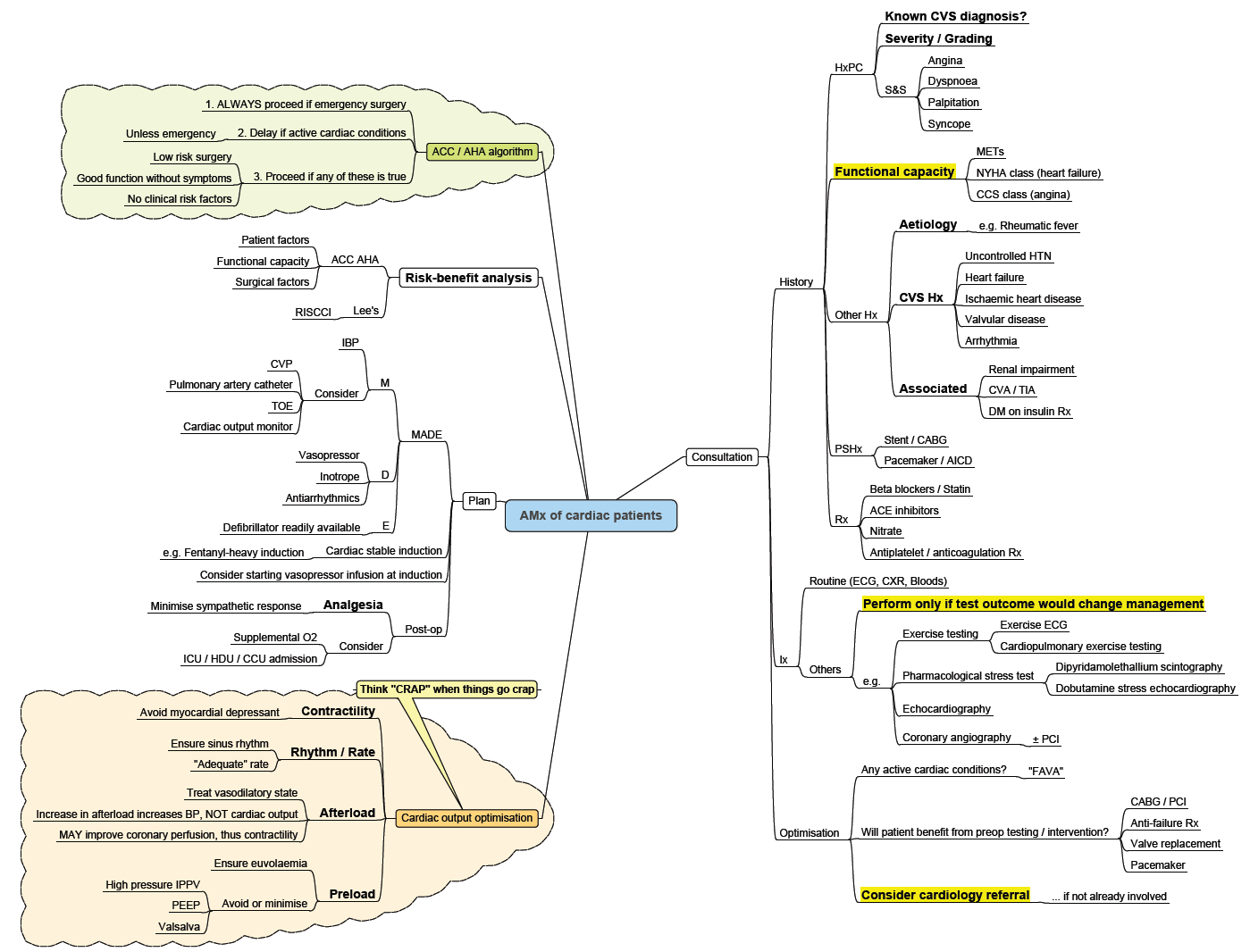
Active Cardiac Condition
Pre-op Evaluation
Major Adverse Cardiovascular Events (MACE) Risk Factors
- Estimate risk
- 6-component Revised Cardiac Risk Index (one point for each)
- 0 (0.4%); 3 or more (10%)
- Ischaemic heart disease
- Cerebrovascular disease
- Heart failure
- CKD (serum creatinine level ≥2.0 mg/dL)
- Insulin dependent diabetes mellitus
- High-risk surgery (intraperitoneal, intrathoracic, or vascular)
- 0 (0.4%); 3 or more (10%)
Factors That Increase Risk 3x Fold
- CKD
- DM
Functional Assessment
- Ask patients whether they can perform workloads of 4 or greater metabolic equivalent tasks (METs) without symptomatic limitation.
- Walking up a hill or climbing up 2 or more flights of stairs
- If unable: 2-fold increased risk of perioperative cardiovascular complications compared with those who are able (9.6% vs 5.2%)
- Self-reported exercise tolerance does not correlate with CPET outputs (peak oxygen consumption and anaerobic threshold), and self-reported METS < 4 had a sensitivity of only 19.4%)
- DASI scores were predictive of the primary outcome
- The DASI combines 12 questions and provides a score, which is then calculated as a metabolic equivalent
- A higher score indicates greater functional capacity
- DASI <34 = predicts increased 30-day mortality, MINS, and MI
- Walking up a hill or climbing up 2 or more flights of stairs
Symptoms and Signs of Concern
- Exertional chest pain, dyspnoea, orthopnoea, palpitations, recent syncope, and physical examination findings, such as murmurs (any diastolic or grade ≥3/6 systolic), gallops, jugular venous distention, or oedema, may indicate cardiovascular disease.
Type of Surgery Risk Assessment for MACE
- Low risk (<1%): Cataract surgery and many types of cosmetic or plastic surgery.
- High risk: Vascular (7.7%), thoracic (6.5%), transplant (6.2%), and general (3.9%)
- Use of minimally invasive, laparoscopic, and endovascular techniques may attenuate cardiovascular risk
Frailty
- In patients aged ≥70 years, being scheduled to undergo intermediate or high-risk NCS, frailty screening should be performed.
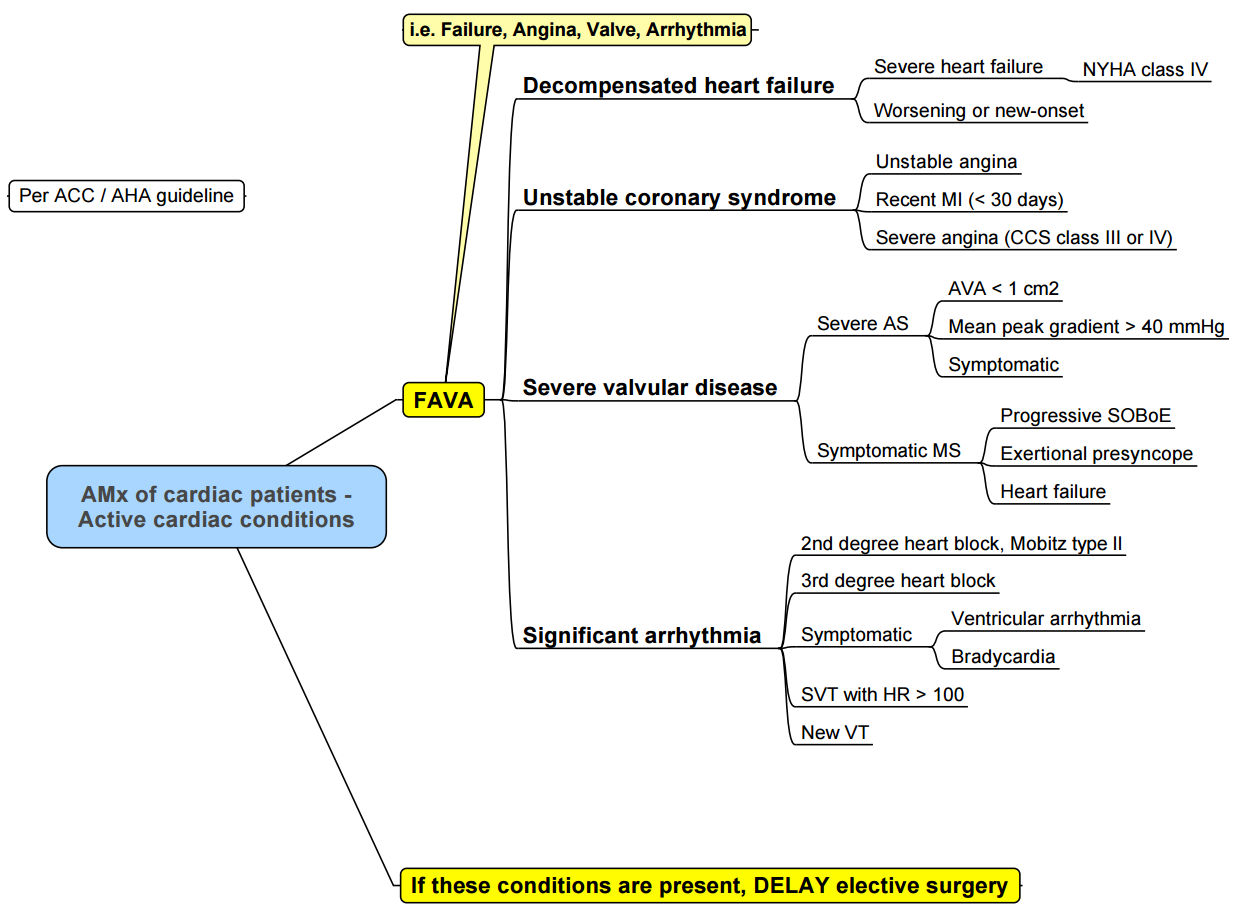
Contraindications to Elective Noncardiac Surgery (“FAVA”)
- Acute coronary syndrome
- Acute decompensated heart failure
- Tachyarrhythmias or bradyarrhythmias associated with hypotension or requiring urgent medical attention (e.g., ventricular tachycardia or high-grade atrioventricular block)
- Symptomatic, severe aortic stenosis (mean gradient >40 mm Hg or peak velocity >4 m/s)
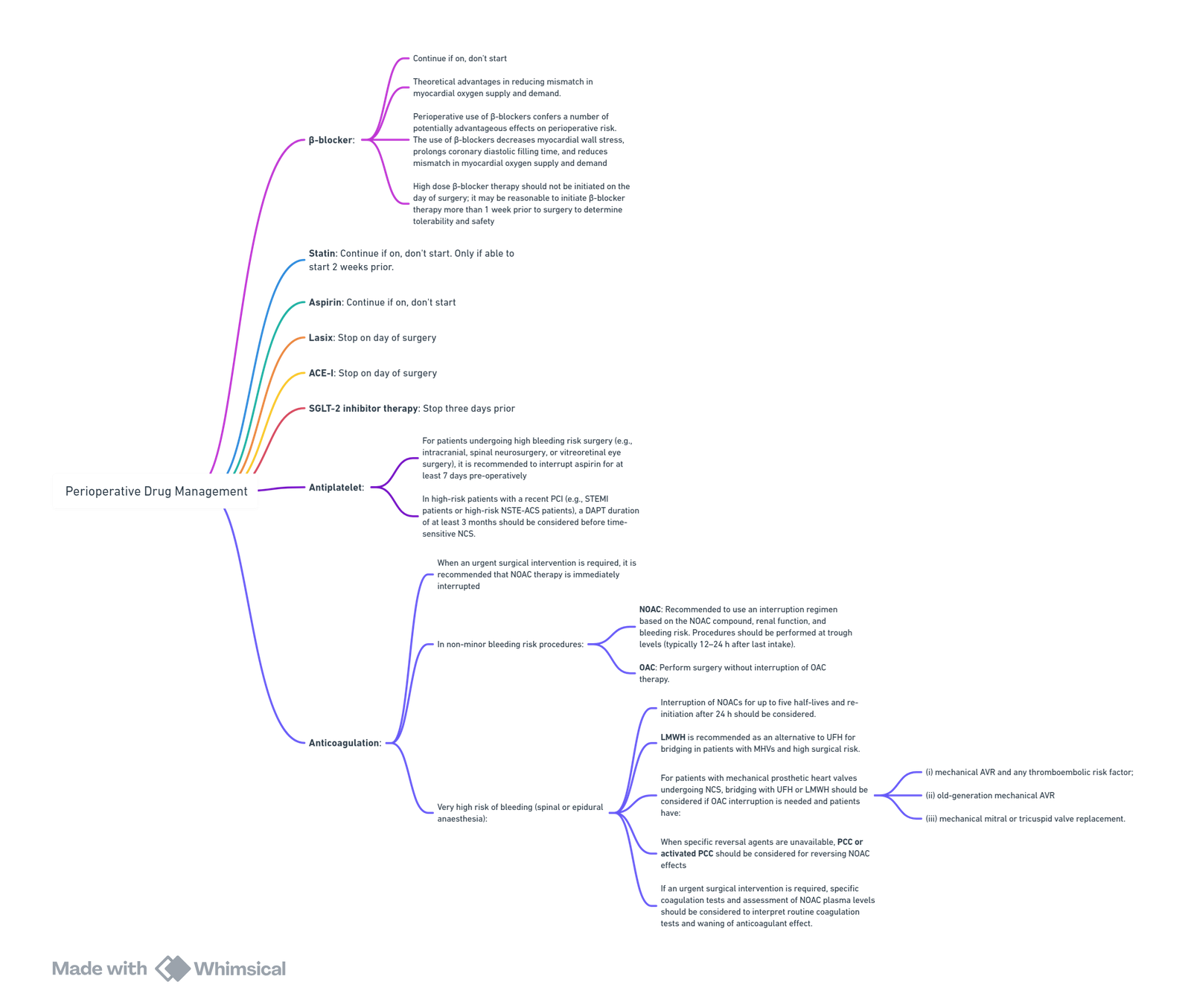
Perioperative Drug Management
Investigations
ECG
- Preoperative ST-segment depressions greater than 0.5 mm are associated with increased risk of postoperative death or myocardial infarction (11.2%)
- Little benefit prior to low-risk surgery such as cataract surgery and cosmetic or plastic surgery
- Indications:
- Risk factor(s) and are scheduled for intermediate or high-risk surgery
- Known CVD or CV risk factors (including age ≥65 years), or symptoms or signs suggestive of CVD
Echocardiography
- Any degree of systolic dysfunction, moderate to severe left ventricular hypertrophy, moderate to severe mitral regurgitation, or an aortic gradient of 20 mm Hg or greater was 80% sensitive for perioperative cardiac events and had a negative predictive value of 97%
- Left ventricular ejection fraction less than 30% was associated with a greater risk of perioperative death, myocardial infarction, and heart failure exacerbation (53.6% vs 26.0% with left ventricular ejection fraction >30%)
- Indications according to surgical risk:
- All risk surgery:
- New murmur and symptoms
- Dyspnoea and/or peripheral oedema and elevated NT-proBNP/BNP
- Family history of genetic cardiomyopathy,
- Intermediate risk:
- Poor functional capacity, abnormal ECG, high NT-proBNP/BNP, or ≥1 clinical risk factor
- Suspected new CVD or unexplained signs or symptoms
- High risk surgery:
- Newly detected murmur suggesting clinically significant pathology
- Poor functional capacity, and/or high NT-proBNP/BNP, or if murmurs are detected
- TTE should be considered in patients with suspected new CVD or unexplained signs or symptoms
- SA guideline:
- Resting echocardiography is not recommended unless there is a clinical suspicion of intracardiac lesion (mitral or aortic stenosis or hypertrophic obstructive cardiomyopathy) or severe pulmonary hypertension.
- All risk surgery:
Pro BNP
- Preoperative BNP levels greater than 92 pg/mL or NT-ProBNP levels greater than 300 pg/mL were associated with increased risk of MACE (21%)
- Indications:
- Canadian guidelines recommend measurement of NT-proBNP or BNP levels prior to noncardiac surgery in patients with cardiovascular disease, a Revised Cardiac Risk Index of 1 or greater, or for those who are aged 65 years or older
- Dyspnoea and/or peripheral oedema, unless there is a certain non-cardiac explanation.
- Known CVD, CV risk factors (including age ≥65 years), or symptoms suggestive of CVD, it should be considered to measure BNP or NT-proBNP
Troponin
- Should be measured perioperatively when signs or symptoms suggest myocardial ischemia or myocardial infarction
- Indications:
- Canadian guidelines recommend postoperative cardiac troponin surveillance in high-risk individuals
- High-risk patients, both before and 48–72 h after major surgery, may be considered
- CVD, CV risk factors (including age ≥65 years), or symptoms suggestive of CVD, it is recommended to measure hs-cTn T or hs-cTn I
Haemoglobin and Bleeding
- In patients scheduled for intermediateto high-risk NCS.
- Treat anaemia in advance of NCS
- Expected blood loss of ≥500 mL, use washed cell salvage.
- Point-of-care diagnostics for guidance of blood component therapy
- In patients undergoing NCS and experiencing major bleeding, administration of tranexamic acid should be immediately considered
HBA1C
- If not performed in the previous 3 months.
- In case of HbA1c ≥8.5% (≥69 mmol/mol), elective NCS should be postponed, if safe and practical.
Stress Imaging
- Stress imaging should be considered before high-risk NCS in asymptomatic patients with poor functional capacity, and previous PCI or CABG.
- Routine cardiac stress testing is not indicated for low-risk patients or for high-risk patients who are able to walk up a hill or climb up 2 or more flights of stairs without difficulty
Coronary Angiography
- CCTA should be considered to rule out CAD in patients with suspected CCS or biomarker-negative NSTE-ACS in case of low-to-intermediate clinical likelihood of CAD, or in patients unsuitable for non-invasive functional testing undergoing non-urgent, intermediate-, and high-risk NCS
SA Perioperative Guideline Summary
Recommendations
-
Patient Selection for Further Preoperative Risk Stratification:
- Elective non-cardiac surgical patients who are 45 years and older with a history of coronary artery disease, congestive cardiac failure, stroke or transient ischemic attack.
- Vascular surgical patients 18 years or older with peripheral vascular disease.
- These patients require further preoperative risk stratification as their predicted 30-day major adverse cardiac event (MACE) risk exceeds 5% (conditional recommendation: moderate-quality evidence).
-
Routine Non-Invasive Testing:
- Routine non-invasive testing for cardiovascular risk stratification prior to elective non-cardiac surgery in adults is not recommended (strong recommendation: low-to-moderate-quality evidence).
-
Preoperative Natriuretic Peptide (NP) Screening:
- Elective non-cardiac surgical patients who are 45 years and older with a history of coronary artery disease, stroke, transient ischemic attack, or congestive cardiac failure.
- Vascular surgical patients 18 years or older with peripheral vascular disease should have preoperative NP screening (strong recommendation: high-quality evidence).
-
Postoperative Troponin Measurements:
- Daily postoperative troponin measurements for 48-72 hours for non-cardiac surgical patients who are 45 years and older with a history of coronary artery disease, stroke, transient ischemic attack, congestive cardiac failure, or vascular surgical patients 18 years or older with peripheral vascular disease.
- This is indicated if:
- Baseline risk >5% for MACE 30 days after elective surgery (if no preoperative NP screening).
- Elevated BNP >99 pg/mL or NT-proBNP >300 pg/mL before elective surgery (conditional recommendation: moderate-quality evidence).
Role of Non-Invasive Testing
Self-Reported Functional Capacity
- Patient-reported ability to exercise is an inaccurate and biased measure of physical fitness.
Resting Echocardiography, Coronary Computed Tomographic Angiography, Pharmacological Stress Echocardiography, and Radionuclide Imaging
- Not recommended for cardiovascular risk assessment.
- Resting echocardiography is inferior to cardiac biomarkers.
- Resting echocardiography is only recommended if there is clinical suspicion of intracardiac lesion (mitral or aortic stenosis or hypertrophic obstructive cardiomyopathy) or severe pulmonary hypertension.
- Coronary computed tomographic angiography overestimates risk and leads to unnecessary cardiac intervention (strong recommendation: moderate-quality evidence).
Exercise Stress Testing and Cardiopulmonary Exercise Testing
- Current evidence does not support their use for cardiovascular risk assessment.
The Role of Natriuretic Peptide Testing in Risk Stratification
- NP testing is a good predictor of perioperative adverse cardiac events and superior to the RCRI.
- BNP >99 pg/mL and NT-proBNP >300 pg/mL are predictive of >5% risk of MACE.
Preoperative NP Thresholds for Predicting 30-Day Mortality and Non-Fatal Myocardial Infarction
| Type of Surgery | Type of NP | NP Level (pg/mL) | MACE (%) (95% CI) |
|---|---|---|---|
| Mixed non-cardiac surgery | BNP | 0 – 99 | 5.3 (3.2 – 7.2) |
| 100 – 250 | 11.6 (4.3 – 18.8) | ||
| ≥250 | 26.9 (17.1 – 35.5) | ||
| NT-proBNP | 0 – 300 | 5.2 (4 – 6.8) | |
| 301 – 900 | 16.1 (12 – 20.2) | ||
| 901 – 3,000 | 26 (18.3 – 33.7) | ||
| >3,000 | 39.5 (26.3 – 52.6) |
Troponin
- Indicated if:
- Baseline risk >5% for MACE 30 days after elective surgery (if no preoperative NP screening).
- Elevated BNP >99 pg/mL or NT-proBNP >300 pg/mL before elective surgery (conditional recommendation: moderate-quality evidence).
- Myocardial injury after non-cardiac surgery (MINS) is defined as a postoperative troponin elevation with no evidence of a nonischemic etiology.
- Classic signs and symptoms of MI are often absent, and it commonly occurs within the first 48 hours after surgery, detectable through daily troponin screening.
- Diagnostic definition of MINS with 5th generation high-sensitivity troponin T (hsTnT): an absolute change of at least 5 ng/L if the level is between 20 to <65 ng/L, or a hsTnT level of at least 65 ng/L.
- Management involves supportive treatment: addressing tachycardia, hypotension, hypoxia, and bleeding (anemia). ECG and cardiology consultation for significant findings (e.g., ST elevation, new left-bundle branch block) are necessary. Statin and aspirin therapy should be started or continued, and beta-blockers should be continued if the patient is hemodynamically stable.
Medication Management
Beta Blockers
- Chronic beta-blocker medication should be continued throughout the perioperative period.
- Beta-blocker therapy should not be started immediately before surgery.
Alpha Agonist
- Not recommended for initiation in the immediate preoperative period.
Calcium Channel Blocker
- Chronic medication can be continued, but initiation in the immediate preoperative period is not recommended.
Aspirin
- Stop acetylsalicylic acid (ASA) at least 3 days before surgery and restart when there is minimal risk of surgical bleeding.
- Perioperative withdrawal of chronic ASA therapy does not increase cardiac or other arterial thrombotic events.
- Continuation of ASA is recommended for patients with recent coronary stents (bare-metal stents within 3 months or drug-eluting stents within 1 year) and patients undergoing carotid endarterectomy.
ACE-I/ARB
- Stop 24 hours before surgery and restart when the risk of hypotension has passed.
Statins
- Statins should be continued in the perioperative period.
SA Flow for Cardiac Risk and ProBNP
Perioperative Risk Assessment Algorithm (SA algorithm)
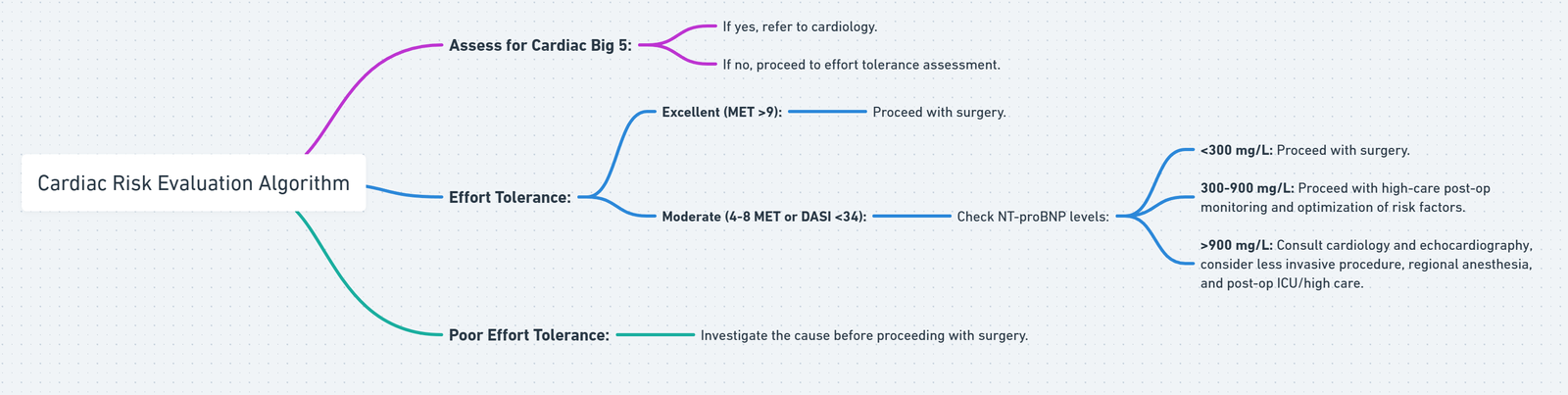
View or edit this diagram in Whimsical.
‘Cardiac Big 5’
- Acute coronary syndromes (ACS)
- Decompensated heart failure (NYHA grades 3 and 4)
- Severe valvular lesions (especially severe aortic stenosis)
- Arrhythmias (especially the tachyarrhythmias or a bradycardia requiring pacing)
- Pericarditis.
- These conditions necessitate an immediate referral to cardiology for either a definitive repair or optimization prior to elective non-cardiac surgery.
2024 Perioperative Cardiovascular Management for Noncardiac Surgery
Major Changes in Perioperative Cardiovascular Management for Noncardiac Surgery (2024)
Definitions of Surgical Timing and Surgical Risk
| Timing | Definition |
|---|---|
| Emergency | Immediate threat to life or limb without surgical intervention, where there is very limited or no time for preoperative clinical evaluation, typically < 2 h. |
| Urgent | Threat to life or limb without surgical intervention, where there may be time for preoperative clinical evaluation to allow interventions that could reduce risk of MACE or other postoperative complications, typically ≥ 2 to < 24 h. |
| Time-sensitive | Surgery may be delayed up to 3 mo to allow for preoperative evaluation and management without negatively impacting outcomes. |
| Elective | The surgical procedure can be delayed to permit a complete preoperative evaluation and appropriate management. |
| Risk Category | Definition |
|---|---|
| Low risk | Combined surgical and patient characteristics predict a low risk of MACE of <1%.* |
| Elevated risk† | Combined surgical and patient characteristics predict an elevated risk of MACE of ≥1%.* |
- Determining elevated calculated risk depends on the calculator used. Traditionally a RCRI >1 or a calculated risk of MACE with any perioperative risk calculator >1% is used as a threshold to identify patients at elevated risk.
- †Encompasses patients at intermediate or high surgical risk.
Preoperative
Risk Assessment
- Systemic approach to perioperative cardiovascular risk assessment.
- Selective use of stress testing, reserved for patients with specific indications.
- In all patients ≥65 years of age and in those <64 years with perceived frailty who are undergoing elevated-risk NCS, preoperative frailty assessment using a validated tool can be useful for evaluating perioperative risk and guiding management
Frailty Assessment Tools
| Name | Items | Scoring |
|---|---|---|
| Physical Frailty Phenotype (Fried phenotype) | Slowness, low activity, weight loss, exhaustion, weakness (1 point each) | 0 = Nonfrail 1–2 = Prefrail 3–5 = Frail |
| Deficit Accumulation Index | Variable; typically 30–70 items from multiple domains | Number of deficits / number of items scored; higher scores indicate greater frailty |
| Edmonton Frail Scale | 10 items across multiple domains | Sum of scores / 17; higher scores indicate greater frailty |
| FRAIL Scale | Fatigue, stair climb, ambulation, illnesses >5, weight loss ≥5% (1 point each) | 0 = Nonfrail 1–2 = Intermediate 3–5 = Frail |
| Clinical Frailty Scale | 9 categories ranging from very fit to terminally ill as assessed by clinicians | Categories 5–8 indicate mild, moderate, severe, and very severe frailty |
| SPPB | Gait speed, chair stands, balance tests | Max 4 points per item, range 0–12 points; ≥10 = Nonfrail, 3–9 = Frail, ≤2 = Disabled |
Medications
- Discontinue Sodium-Glucose Cotransporter-2 inhibitors (SGLT2i) 3 to 4 days before surgery to reduce risk of perioperative ketoacidosis.
- Stop oral anticoagulants (OAC) as per guidelines, primarily in cases with lower thrombotic risk.
Intraoperative/Postoperative
Monitor and Follow-up
- Cardiac imaging (TEE or FoCUS) should be considered for hemodynamically unstable patients intraoperatively.
- Postoperative surveillance for myocardial injury (MINS) should be considered in high-risk patients.
- Manage new-onset atrial fibrillation (AF) postoperatively with close follow-up.
- Resume oral anticoagulants (OAC) postoperatively, if indicated, with selective bridging for patients with high thrombotic risk.
Stepwise Approach to Perioperative Cardiac Assessment for Patients with Cardiovascular Risk Factors Scheduled for Non-Cardiac Surgery (NCS)
1. Initial Assessment
- Patient with Cardiovascular Risk Factors, Disease, or Symptoms Scheduled for NCS?
- NO: Proceed to surgery.
- YES: Is it emergency surgery?
- YES: Proceed to surgery.
- NO: Manage acute cardiac condition (if present) and conduct multidisciplinary team discussion to consider deferral of surgery, noninvasive treatment, or palliative care.
2. Management of Acute Cardiac Conditions
- Does the patient have,Acute coronary syndrome, Unstable cardiac arrhythmias, Unstable Valvulopathy or Decompensated heart failure
- YES: Manage condition as per standard guidelines and re-evaluate for surgery later.
- NO: Continue to perioperative risk estimation.
3. Estimation of Perioperative Risk
- Use a risk calculator for major adverse cardiovascular events
- Does the patient have any of the following risk modifiers:
- Severe valvular heart disease
- Severe pulmonary hypertension
- Elevated risk of congenital heart disease (CHD)
- Severe or uncontrolled coronary artery disease (CAD)
- Prior stroke
- CIED
- Frailty
- NO: Proceed to surgery (If no risk modifiers and low calculated risk <1% for MACE)
- YES: Consider further perioperative risk assessment (below).
- Does the patient have any of the following risk modifiers:
4. Risk Modification and Testing for Elevated Risk Patients
- Low Calculated Risk or no risk modifiers: Proceed to surgery.
- Elevated Calculated Risk with no risk modifiers (RCRI >1 or calculated major adverse cardiac event risk >1%):
- For asymptomatic patients without established cardiovascular disease (CVD):
- Consider 12-lead ECG
- Consider initiation of guideline-directed medical therapy (GDMT) for long-term cardiovascular risk reduction and disease management.
- For asymptomatic patients without established cardiovascular disease (CVD):
- ANY Calculated Risk with risk modifiers present:
- For patients with established CVD or symptoms:
- 12-lead ECG is reasonable
- Echocardiography for patients with suspected moderate-to-severe valvular disease, suspected significant LV dysfunction, or worsening dyspnea
- Consider GDMT initiation for long-term management
- For patients with established CVD or symptoms:
5. Functional Capacity Evaluation
- Does the patient have poor or unknown functional capacity (e.g., ≤34 Duke Activity Status Index or ≤4 METs)?
- YES: Proceed to further testing if the results will impact decision making/perioperative care
- NO: Proceed to surgery.
6. Preoperative Biomarker Risk Assessment
- If elevated risk or poor functional capacity is suspected, assess preoperative biomarkers:
- BNP/NT-proBNP.
- Troponin.
- Normal biomarkers: Proceed to surgery.
- Abnormal biomarkers: Further testing and evaluation required (next section).
- Abnormal Biomarkers: Troponin >99th percentile upper reference limit (URL); BNP >92 ng/L, NT-proBNP ≥300 ng/L.
7. Preoperative Testing for Abnormal Biomarkers
- Consider the following tests based on biomarker results:
- Echocardiography for further evaluation.
- Noninvasive stress testing for patients with elevated findings.
- Coronary computed tomography angiography (CCTA) for high-risk findings.
- If low-risk findings: Proceed to surgery.
- If elevated-risk finding:
- Pursue further cardiac evaluation and management.
- Consider deferring surgery or implementing noninvasive/invasive treatment.
8. Postoperative Surveillance
- For patients with elevated preoperative troponin levels, consider postoperative troponin surveillance.
Key Definitions:
- Cardiovascular Risk Factors: Include hypertension, smoking, high cholesterol, diabetes, age (women >65 years; men >55 years), obesity, family history of premature coronary artery disease (CAD).
Summary of Recommendations for Specific Conditions from 2024 Guidelines
Coronary Revascularization
- ACS: Coronary revascularization and deferral of elective NCS is recommended to reduce perioperative cardiovascular events (Class 1, C-LD).
- Left Main CAD ≥50%: Revascularization and deferral of elective NCS is reasonable (Class 2a, C-LD).
- Non-left Main CAD: Routine revascularization before NCS is not recommended (Class 3: No benefit, B-R).
Hypertension and Perioperative Blood Pressure Management
- Preoperative:
- Continue hypertension therapy throughout the perioperative period (Class 2a, C-EO).
- Consider deferring elective surgery if SBP ≥180 mm Hg or DBP ≥110 mm Hg (Class 2b, C-LD).
- Intraoperative:
- Maintain MAP ≥60-65 mm Hg or SBP ≥90 mm Hg to reduce myocardial injury (Class 1, B-NR).
- Postoperative:
- Treat hypotension (MAP <60-65 mm Hg or SBP <90 mm Hg) to limit cardiovascular, cerebrovascular, and renal risks (Class 1, B-NR).
- Restart preoperative antihypertensive medications early postoperatively (Class 1, C-EO).
Heart Failure
- SGLT2i: Discontinue 3-4 days before elective NCS to avoid metabolic acidosis (Class 1, C-LD).
- GDMT: Continue GDMT unless contraindicated for patients with compensated HF (Class 2a, C-LD).
Pulmonary Hypertension (PH)
- Targeted Medical Therapy: Continue for PAH patients undergoing NCS to reduce perioperative major adverse cardiovascular events (MACE) (Class 1, C-LD).
- Severe PH: Referral to a specialized PH center for risk assessment and management is reasonable (Class 2a, C-LD).
- Invasive Hemodynamic Monitoring: Reasonable in severe PH cases during elevated-risk surgery (Class 2a, C-LD).
- Precapillary PH: Inhaled pulmonary vasodilators may be considered to reduce RV afterload (Class 2b, C-EO).
Congenital Heart Disease (CHD) Management
- Assess and review cardiac anatomy, prior procedures, and functional status.
- Identify risk factors (e.g., cyanosis, HF, pulmonary hypertension).
- Considerations: endocarditis prophylaxis, venous thrombosis prevention, renal and liver function monitoring, perioperative anticoagulation, and arrhythmias.
Left Ventricular Assist Devices (LVAD)
- Coordinate with the LVAD care team on perioperative considerations for elective NCS to reduce MACE risk (Class 1, C-EO).
Aortic Stenosis (AS)
- Severe AS: Evaluate for aortic valve intervention before elective NCS (Class 1, C-LD).
- Moderate or Severe AS: Preoperative echocardiography recommended for elevated-risk NCS (Class 1, C-EO).
- Asymptomatic Moderate/Severe AS with Normal LV Function: Proceed with elective low-risk NCS (Class 2a, C-LD).
Aortic Stenosis Management Summary
- Symptomatic Severe AS: AVR if candidate before elevated-risk NCS.
- Asymptomatic Severe AS:
- If LVEF <50%, consider AVR.
- If LVEF ≥50% and elevated-risk surgery, proceed after shared decision-making.
- If low-risk surgery, proceed without AVR.
Mitral Stenosis (MS)
- Severe MS: Evaluate for MV intervention before elective NCS (Class 1, B-NR).
- Non-candidates for MV Intervention: Use perioperative hemodynamic monitoring (Class 2a, C-EO).
- Heart Rate Control: Beta blockers, calcium channel blockers, ivabradine, or digoxin may be used to prolong diastolic filling (Class 2b, C-LD).
Chronic Aortic and Mitral Regurgitation
- Moderate/Severe Valvular Regurgitation: Preoperative echocardiography recommended to guide management (Class 1, C-EO).
- Valvular Heart Disease (VHD): Intervention before elevated-risk NCS should be considered (Class 1, C-EO).
- Asymptomatic MR or AR: Elective NCS is reasonable in patients with normal LV function (Class 2a, C-LD).
Previous Transcatheter Valve Repair
- TAVI Patients: NCS can be performed early if clinically indicated (Class 2a, B-NR).
- Mitral Valve TEER Patients: NCS is reasonable after successful MV intervention (Class 2a, C-EO).
Atrial Fibrillation (AF)
-
Perioperative:
- Treat underlying triggers for rapid AF during NCS (Class 2a, C-LD).
- Postoperative anticoagulation may be initiated for new-onset AF, considering thromboembolism and bleeding risks (Class 2a, C-LD).
-
Postdischarge:
- Follow-up for thromboembolic risk stratification and AF surveillance is recommended for new-onset AF after NCS (Class 1, C-LD).
Preoperative Management of Cardiovascular Implantable Electronic Devices (CIED)
- Management Plan: Develop a plan for patients with CIED undergoing NCS if EMI is anticipated (Class 1, B-NR).
- Pacemaker: Reprogram or use a magnet if the patient is pacemaker-dependent and surgery is above the umbilicus (Class 1, B-NR).
- ICD: Reprogram or use a magnet for pacemaker-dependent patients with ICD undergoing surgery above the umbilicus (Class 1, B-NR).
- Subcutaneous ICD: Reprogram the device or use a magnet for nonthoracic surgery with EMI (Class 2a, C-LD).
Stroke or Transient Ischemic Attack (TIA)
- Delay elective NCS for at least 3 months after a cerebrovascular event to reduce stroke and MACE (Class 2a, B-NR).
Obstructive Sleep Apnea (OSA)
- Screening for OSA using validated questionnaires is reasonable to assess perioperative complication risks (Class 2a, B-NR).
Perioperative Medication Recommendations
Beta Blockers
- Continuation: In patients already on stable doses of beta blockers undergoing NCS, continuation of therapy is recommended throughout the perioperative period (Class 1, B-NR).
- New Initiation: In patients scheduled for elective NCS with a new indication for beta blockers, initiation should occur >7 days before surgery to assess tolerability and allow for titration (Class 2b, B-NR).
- Avoidance on Day of Surgery: Beta blocker initiation on the day of surgery without a clear need should be avoided due to increased risk of postoperative mortality (Class 3: Harm, B-R).
Statins
- Continuation: In patients already on statins and scheduled for NCS, continuation of statin therapy is recommended to reduce the risk of MACE (Class 1, B-NR).
- Initiation: In statin-naïve patients who meet criteria for statin use based on ASCVD history or 10-year risk, perioperative initiation of statins is recommended, with the intention of long-term use (Class 1, B-R).
Renin-Angiotensin-Aldosterone System Inhibitors (RAASi)
- Discontinuation for Hypertension: In select hypertensive patients undergoing elevated-risk NCS, omission of RAASi 24 hours before surgery may be beneficial to reduce intraoperative hypotension (Class 2b, B-R).
- Continuation for HFrEF: In patients on RAASi for heart failure with reduced ejection fraction (HFrEF), perioperative continuation is reasonable (Class 2a, C-EO).
Alpha-2 Receptor Agonists
- Clonidine: The initiation of low-dose clonidine perioperatively is not recommended for reducing cardiovascular risk in patients undergoing NCS (Class 3: No benefit, B-R).
Antiplatelet Therapy and Timing of Noncardiac Surgery (NCS) in Patients with Coronary Artery Disease (CAD)
Timing Of NCS After PCI
- General Management: For patients with CAD undergoing elective NCS, perioperative antiplatelet therapy and timing of surgery should be determined by a multidisciplinary team (Class 1, B-NR).
- Post Balloon Angioplasty: For patients with recent coronary balloon angioplasty without stent placement, NCS should be delayed for a minimum of 14 days (Class 1, C-LD).
- Post DES-PCI for ACS: Elective NCS should be delayed for at least 12 months after DES-PCI for ACS to minimize perioperative MACE (Class 1, B-NR).
- Post DES-PCI for CCD: For chronic coronary disease (CCD) patients, it is reasonable to delay NCS for at least 6 months after DES-PCI (Class 2a, B-NR).
- Time-Sensitive NCS Post DES-PCI: NCS may be considered ≥3 months after DES-PCI if surgery cannot be delayed and the risk of MACE is outweighed by the need for surgery (Class 2b, B-NR).
- High Risk of Stent Thrombosis: Elective NCS within 30 days of bare-metal stent (BMS) or DES-PCI, requiring interruption of antiplatelet agents, is considered potentially harmful (Class 3: Harm, B-R).
Perioperative Antiplatelet Management Post PCI
- Continuation of Aspirin: For patients with prior PCI undergoing NCS, continuing aspirin (75-100 mg) is recommended if possible, to reduce the risk of cardiac events (Class 1, B-R).
- DAPT in Time-Sensitive NCS: Dual antiplatelet therapy (DAPT) should be continued for patients requiring NCS within 30 days of PCI unless bleeding risk outweighs benefits (Class 1, B-NR).
- Aspirin for PCI Patients on OAC: If oral anticoagulation (OAC) must be discontinued before NCS, continuing aspirin is recommended, with OAC resumed postoperatively (Class 1, B-NR).
- Bridging Therapy: Perioperative bridging with intravenous antiplatelet therapy may be considered in patients with high thrombotic risk ≤6 months after BMS or DES-PCI, if NCS cannot be deferred (Class 2b, B-NR).
Perioperative Antiplatelet Management in Patients Without Prior PCI
- Aspirin Continuation: In patients with CCD without prior PCI undergoing elective NCS, continuing aspirin may be reasonable if the risk of cardiac events outweighs bleeding risk (Class 2b, B-NR).
- No Benefit from Aspirin Initiation: Routine initiation of aspirin in patients with CAD but without prior PCI undergoing elective NCS is not beneficial (Class 3: No benefit, B-R).
Oral Anticoagulants (OAC) Management
OAC Management
- Multidisciplinary Approach: For patients on OAC undergoing elective NCS, a multidisciplinary team-based approach is recommended to balance the risks of thromboembolism and bleeding (Class 1, B-NR).
OAC Bridging
- Bridging with Heparin: In patients with high thrombotic risk undergoing NCS where vitamin K antagonist (VKA) interruption is required, bridging with parenteral heparin is effective in reducing thromboembolic risk (Class 2a, C-LD).
- No Routine Bridging: Routine perioperative bridging of OAC in most patients is not recommended due to increased bleeding risk (Class 3: Harm, C-LD).
OAC Resumption
- Resumption After Haemostasis: After preoperative OAC interruption, resumption of OAC is reasonable once haemostasis is achieved (Class 1, C-LD).
Optimal Timing of Elective or Time-Sensitive NCS for Prior PCI Requiring Management of DAPT
- Balloon Angioplasty (No Stent): Delay NCS for ≥14 days.
- Bare-Metal Stent (BMS): Delay NCS for ≥30 days.
- DES-PCI for ACS: Delay NCS for ≥12 months. If surgery is time-sensitive, NCS may be considered after ≥3 months if the risk of delaying surgery outweighs MACE.
- DES-PCI for CCD: Delay NCS for ≥6 months.
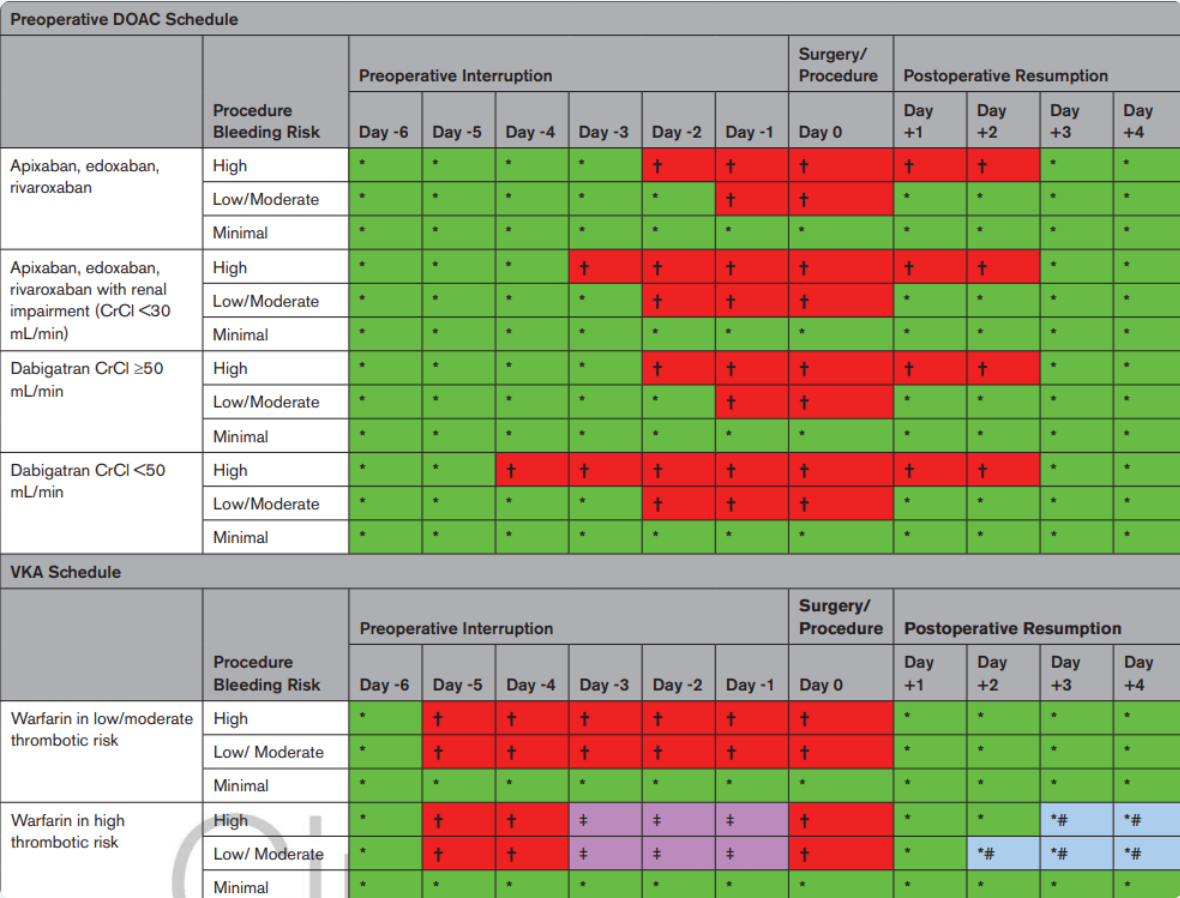
Image Ref: Thompson, A., Fleischmann, K. E., Smilowitz, N. R., de las Fuentes, L., Mukherjee, D., Aggarwal, N. R., … & Williams Sr., K. A. (2024). 2024 AHA/ACC/ACS/ASNC/HRS/SCA/SCCT/SCMR/SVM guideline for perioperative cardiovascular management for noncardiac surgery: A report of the American College of Cardiology/American Heart Association Joint Committee on Clinical Practice Guidelines. Circulation. https://doi.org/10.1161/cir.0000000000001285. Section 7.6
Key
Management for perioperative bleeding risk and DOAC or VKA schedule should incorporate team-based decision-making, especially in high thrombotic risk patients or when undergoing procedures with higher risks of adverse outcomes, should bleeding occur (e.g., neuraxial anesthesia).
- Minimal bleeding risk: 30-day risk of major bleeding 0% (e.g., cataract surgery, minor dental/dermatological procedures).
- Low/moderate bleeding risk: 30-day risk of major bleeding <2% (e.g., complex dental, gastrointestinal, breast surgery, procedures using large-bore needles).
- High bleeding risk: 30-day risk of major bleeding ≥2%.
Symbols: - *: Administer DOAC or VKA.
- †: Withhold DOAC or VKA.
- ‡: While withholding VKA in select very high thrombotic risk patients, preoperative bridging with parenteral heparin once INR is less than the desired therapeutic range.
-
: Resuming postoperative LMWH bridge at either full dose or prophylactic dose until INR is within the therapeutic range is a team-based decision that weighs risks and benefits.
Thromboembolic Risk for Common Oral Anticoagulant Indications
| Risk Category | Venous Thromboembolism | Atrial Fibrillation | Mechanical Valve | Other Anticoagulation Indications |
|---|---|---|---|---|
| Low | VTE >12 months | CHA₂DS₂-VASc 1-4 (without prior history of stroke) | Bileaflet mechanical AVR without major risk factors for stroke* | Nonsevere coagulopathy (e.g., heterozygous factor V Leiden or prothrombin gene G20210A mutation), active cancer |
| Moderate | VTE ≤3-12 months, recurrent VTE | CHA₂DS₂-VASc 5-6 | Bileaflet mechanical AVR with major risk factors for stroke, mitral valve without major risk factors for stroke | Active cancer |
| High | Recent VTE (<1 month or <3 months) | CHA₂DS₂-VASc ≥7 (or 5-6 with recent stroke or TIA), AF with rheumatic valvular heart disease | Mechanical mitral valve, caged ball or tilting-disk valve, mechanical heart valve in any position with recent stroke or TIA (<3 months) | Recent cardioembolic stroke (<3 months)†, active cancer associated with high VTE risk, LV thrombus (within past 3 months), severe thrombophilia†, antiphospholipid antibodies |
Recommendations for Anaesthesia and Perioperative Practices from 2024 Guideline
Perioperative Management of Blood Glucose
- Preoperative Hemoglobin A1c Testing: In patients with or at risk for diabetes undergoing elective NCS, preoperative hemoglobin A1c testing is reasonable if it has not been performed within the past 3 months (Class 2a, B-NR).
- SGLT2i Discontinuation: For patients scheduled for NCS, sodium-glucose cotransporter-2 inhibitors (SGLT2i) should be discontinued 3-4 days before surgery to reduce the risk of perioperative metabolic acidosis (Class 1, C-LD).
- Metformin Continuation: In patients with diabetes or impaired glucose tolerance, continuation of metformin during the perioperative period is reasonable to maintain glycemic control (Class 2a, C-LD).
Choice Of Anesthetic Technique and Agent
- General Anesthesia: For patients undergoing NCS, the use of volatile-based anesthetic agents or total intravenous anesthesia is reasonable, with no significant difference in cardiovascular outcomes (e.g., MI, ischemia) (Class 2a, A).
- Neuraxial vs. General Anesthesia: In patients undergoing NCS where neuraxial anesthesia is feasible, both neuraxial and general anesthesia are reasonable options with no significant difference in cardiovascular events (Class 2a, B-R).
Perioperative Pain Management
- Epidural Analgesia for Abdominal Surgery: For patients undergoing major abdominal surgery, epidural analgesia for postoperative pain relief is reasonable to decrease perioperative cardiac events (Class 2a, B-R).
- Epidural Analgesia for Hip Fracture: For patients with hip fractures awaiting surgical repair, epidural analgesia may be considered to decrease the incidence of preoperative cardiac events (Class 2b, B-R).
Echocardiography
- TEE or FoCUS for Hemodynamic Instability: In patients with unexplained hemodynamic instability undergoing NCS, the emergency use of perioperative transesophageal echocardiography (TEE) or focused cardiac ultrasound (FoCUS) is reasonable to determine the cause, provided expertise is available (Class 2a, C-LD).
- No Routine Intraoperative TEE: Routine use of intraoperative TEE is not recommended in patients without risk factors or procedural risks for significant hemodynamic compromise to screen for cardiac abnormalities or monitor for myocardial ischemia (Class 3: No benefit, C-LD).
Body Temperature Management
- Normothermia Maintenance: In patients with cardiovascular disease (CVD) undergoing NCS, maintaining normothermia is reasonable to avoid perioperative complications (Class 2a, B-R).
Pulmonary Artery Catheters
- Selective Use: Pulmonary artery catheterization may be considered in patients with CVD undergoing NCS when medical conditions significantly affect hemodynamics (e.g., decompensated heart failure, severe valvular disease, pulmonary hypertension) and cannot be corrected before surgery (Class 2b, C-LD).
- No Routine Use: Routine use of pulmonary artery catheters in patients with CVD undergoing NCS is not recommended to reduce morbidity or mortality (Class 3: No benefit, A).
Perioperative Anemia Management
- Tranexamic Acid: In patients having NCS with expected blood loss, tranexamic acid is reasonable to reduce intraoperative blood loss, reduce transfusions, and avoid anemia (Class 2a, A).
- Iron Therapy: For patients with iron deficiency anemia undergoing elective NCS, preoperative iron therapy (oral or IV) is reasonable to reduce the need for blood transfusions and increase hemoglobin levels (Class 2a, B-R).
Recommendations for Postoperative Complications
Myocardial Injury After Noncardiac Surgery (MINS) Surveillance
- Cardiac Troponin Monitoring: In patients with known cardiovascular disease (CVD), symptoms of CVD, or those aged ≥65 years with cardiovascular risk factors undergoing elevated-risk NCS, it may be reasonable to measure cardiac troponin (cTn) at 24 and 48 hours postoperatively to identify myocardial injury (Class 2b, B-NR).
MINS Management
- Outpatient Follow-up: In patients who develop MINS, particularly those not previously known to have excess cardiovascular risk, outpatient follow-up is reasonable for optimization of cardiovascular risk factors (Class 2a, B-NR).
- Antithrombotic Therapy: In patients who develop MINS, antithrombotic therapy may be considered to reduce thromboembolic events (Class 2b, C-LD).
MINS Management Flowchart Summary
- Troponin >99th Percentile:
- Evaluate via history/physical examination and 12-lead ECG.
- ST-segment elevations?
- Yes (STEMI): Consider invasive coronary angiography (ICA) and guideline-directed medical therapy (GDMT).
- No:
- Criteria for Myocardial Infarction (MI) met?
- Yes (NSTEMI):
- Type 1 NSTEMI (plaque rupture): Consider GDMT and ICA, balancing bleeding and thrombotic risks.
- Type 2 NSTEMI (supply-demand mismatch): Treat the underlying cause with GDMT and optimize perioperative hemodynamic status.
- No:
- Postoperative Myocardial Injury:
- Nonischemic: Treat the underlying cause.
- MINS: Outpatient follow-up for risk factor optimization is reasonable.
- Postoperative Myocardial Injury:
- Yes (NSTEMI):
- Criteria for Myocardial Infarction (MI) met?
Recommendations for Management of Postoperative STEMI/NSTEMI
- STEMI Management: Patients who develop STEMI after NCS should be considered for GDMT, including ICA, balancing bleeding and thrombotic risks based on clinical severity (Class 1, B-NR).
- NSTEMI Management:
- Patients who develop NSTEMI after NCS should receive medical therapy as recommended for spontaneous MI, with consideration of postoperative bleeding risks and hemodynamic status (Class 1, C-EO).
- ICA Consideration: Patients who develop NSTEMI after NCS may be considered for ICA, balancing bleeding and thrombotic risks based on the severity of the clinical presentation (Class 2a, C-LD).
Perioperative Myocardial Infarction (MINS)
Systematic Work-up and Treatment of Peri-Operative Myocardial Injury/Infarction
Step 1: Initial Assessment
- 12-lead ECG, symptoms, and haemoglobin:
- ST elevation (ST↑) or ST depression (ST↓) or typical chest pain:
- Severe anaemia (Hb <80 g/L):
- Yes: Type 2 MI
- Immediate transfusion followed by reassessment for ICA.
- No: Type 1 MI
- ICA, aspirin, statin, and monitoring (Class I).
- Yes: Type 2 MI
- Severe anaemia (Hb <80 g/L):
- ST elevation (ST↑) or ST depression (ST↓) or typical chest pain:
Step 2: Echocardiography
- Transthoracic echocardiography:
- Other cardiac cause:
- Yes:
- Tachyarrhythmia (Type 2 MI)
- Acute heart failure (injury)
- Aortic valve stenosis (injury)
- Treat cause.
- No: Proceed to step 3.
- Yes:
- Other cardiac cause:
Step 3: Non-Cardiac Causes
- Non-cardiac cause:
- Yes:
- Sepsis
- Pulmonary embolism
- Stroke (injury)
- Treat cause.
- No: Proceed to step 4.
- Yes:
Step 4: Severe Anaemia or Hypotension
- Severe anaemia (Hb <80 g/L) or severe (documented) hypotension:
- Yes: Type 2 MI
- Treat cause.
- No: Proceed to step 5.
- Yes: Type 2 MI
Step 5: Hypotension or Missed MI
- Relative or undocumented hypotension:
- Yes: Type 2 MI or missed Type 1 MI
- Aspirin, statin, stress imaging/CCTA/ICA.
- Yes: Type 2 MI or missed Type 1 MI
Summary
- Transfusion and re-assessment for severe anaemia.
- Treat underlying cause for other cardiac or non-cardiac etiologies.
- Type 1 MI: Management includes ICA, aspirin, statin, and monitoring.
- Type 2 MI: Management involves treating the cause (e.g., anaemia, hypotension).
Peri-Operative Approach to Patients with Ventricular Assist Devices Undergoing Non-Cardiac Surgery
Pre-Operative
- Multidisciplinary team identified:
- Primary surgical and anaesthesia teams
- Cardiac surgery team
- HF cardiologist
- VAD personnel
- Pre-operative medical optimization when possible or necessary.
- Physical examination focused on the sequelae of HF.
- Baseline tests:
- ECG
- Echocardiogram
- Laboratory values
- Manage pacemaker/ICD settings when indicated.
- CT examination to evaluate possible driveline interference with the operative field.
- Anticoagulation management: Hold, bridge, or reverse anticoagulation when indicated, after VAD team consultation.
Intra-Operative
- Monitoring:
- Standard American Society of Anaesthesiologists monitors.
- Cerebral tissue oxygenation.
- Processed electroencephalogram.
- Arterial line with ultrasound guidance.
- Central venous catheter if fluid shifts are expected.
- PA catheter only if severe pulmonary hypertension.
- TEE available.
- Monitor VAD control console.
- External defibrillator pads in place.
- Optimize pre-load, support RV function, avoid increase in afterload.
- Gradual peritoneal insufflations and position changes.
Post-Operative
- Care Unit: Standard post-anaesthesia care unit unless ICU is otherwise indicated.
- Extubation criteria are unchanged.
- Avoid hypoventilation, optimize oxygenation.
- Resume heparin infusion when post-operative bleeding risk is acceptable.
Management of Oral Anticoagulation Therapy in Patients Undergoing Non-Cardiac Surgery (NCS)
Patient Assessment and Risk Stratification
NCS-Related Bleeding Risk
- High Bleeding Risk NCS:
- Yes: Assess thrombotic risk.
- No: Proceed with standard management.
Thrombotic Risk
-
High Thrombotic Risk:
- Yes: Evaluate specific patient conditions:
- Mechanical Heart Valve:
- Use VKA or VKA/NOAC:
- VKA: Continue with INR in lower level or short interruption (Class I).
- VKA/NOAC: Bridging is not recommended (Class III).
- Bridging: Consider (Class IIa).
- Use VKA or VKA/NOAC:
- Selected Patients with Very High Thromboembolic Risk:
- Evaluate if NCS can be deferred.
- Yes: Defer NCS (Class I).
- No: Interrupt anticoagulation (Class I).
- Bridging is not recommended (Class III).
- Evaluate if NCS can be deferred.
- Mechanical Heart Valve:
- Yes: Evaluate specific patient conditions:
-
Not High Thrombotic Risk:
- Proceed with standard anticoagulation management.
Recommendations Based on Anticoagulant Type
-
Vitamin K Antagonist (VKA):
- Continue with INR in lower level or short interruption (Class I).
- Bridging is not recommended (Class III).
-
Non-Vitamin K Antagonist Oral Anticoagulant (NOAC):
- Short interruption (Class I).
- Bridging is not recommended (Class III).
Bridging with Intravenous Antiplatelet Agents for Non-Cardiac Surgery (NCS)
Overview
This guideline provides a structured approach for bridging patients on antiplatelet therapy undergoing non-cardiac surgery (NCS), ensuring the continuation of low-dose ASA (acetylsalicylic acid) throughout the perioperative period.
Pre-Operative Management
Days -7 to -1
- Discontinue Prasugrel:
- Stop 7 days before surgery.
- Discontinue Clopidogrel/Ticagrelor:
- Stop 5 days before surgery.
Days -3 to -1
- Infusion of Tirofiban/Eptifibatide:
- Tirofiban:
- Start 0.1 μg/kg/min; adjust to 0.05 μg/kg/min if creatinine clearance <50 mL/min.
- Eptifibatide:
- Start 2.0 μg/kg/min; adjust to 1.0 μg/kg/min if creatinine clearance <50 mL/min.
- Continue infusion until oral P2Y12_{12}12 inhibitor therapy is possible.
- Tirofiban:
Perioperative Management
Day 0 (Day of Surgery)
- NCS:
- Continue low-dose ASA throughout.
- Infusion of Tirofiban/Eptifibatide: Continue until 4-6 hours before surgery.
- Post-Surgery (4-6 hours after NCS):
- Restart Clopidogrel (LD 300 mg), followed by 75 mg once daily (o.d.).
- Alternatively, restart Tirofiban/Eptifibatide or Cangrelor.
Post-Operative Management
Follow-Up/Discharge
- Continue low-dose ASA throughout.
- Clopidogrel: Start with a loading dose (LD) of 300 mg, followed by 75 mg o.d. or restart the infusion agent used pre-operatively (Tirofiban/Eptifibatide/Cangrelor).
Notes
- Tirofiban Dose Adjustment:
- Standard: 0.1 μg/kg/min.
- If creatinine clearance <50 mL/min: Adjust to 0.05 μg/kg/min.
- Eptifibatide Dose Adjustment:
- Standard: 2.0 μg/kg/min.
- If creatinine clearance <50 mL/min: Adjust to 1.0 μg/kg/min.
- Cangrelor Infusion:
- Initiate within 72 hours from P2Y12_{12}12 inhibitor discontinuation at a dose of 0.75 μg/kg/min for a minimum of 48 hours and a maximum of 7 days.
This bridging strategy ensures the balance between minimizing thrombotic risk and managing bleeding risk during the perioperative period for patients on antiplatelet therapy undergoing non-cardiac surgery.
C4NC Guidelines
Perioperative Risk Assessment and Postoperative Monitoring for Patients Undergoing Non-Cardiac Surgery
Patient Selection
- Age ≥45 years with known significant cardiovascular disease.
- Age 18-44 years with known significant cardiovascular disease.
- Undergoing non-cardiac surgery requiring overnight hospital admission.
Timing of Surgery
-
Emergency Surgery:
- Proceed to surgery without additional preoperative cardiac assessment.
-
Urgent/Semi-Urgent Surgery:
- Proceed to surgery.
- Undertake preoperative cardiac assessment only if there is an unstable cardiac condition or suspected undiagnosed severe pulmonary hypertension (PHTN) or obstructive cardiac disease.
-
Elective Surgery:
- Assess perioperative cardiac risk.
- Perform risk stratification with the Revised Cardiac Risk Index (RCRI).
- If RCRI ≥1, or age ≥65 years, or age 45-64 years with significant cardiovascular disease, order NT-proBNP/BNP.
Preoperative Assessment
- Age ≥65 years or 18-64 years with significant cardiovascular disease:
- Positive NT-proBNP/BNP:
- NT-proBNP ≥300 mg/L or BNP ≥92 mg/L.
- Measure troponin daily for 48-72 hours.
- Obtain ECG in PACU.
- Consider in-hospital shared-care management.
- NT-proBNP/BNP not available:
- Measure troponin daily for 48-72 hours.
- Obtain ECG in PACU.
- Consider in-hospital shared-care management.
- Negative NT-proBNP/BNP:
- NT-proBNP <300 mg/L or BNP <92 mg/L.
- No additional routine postoperative monitoring.
- Positive NT-proBNP/BNP:
Decision Algorithm
-
Emergency Surgery:
- Proceed to surgery without additional preoperative cardiac assessment.
-
Urgent/Semi-Urgent Surgery:
- Proceed to surgery.
- Undertake preoperative cardiac assessment only if there is an unstable cardiac condition or suspected undiagnosed severe PHTN or obstructive cardiac disease.
-
Elective Surgery:
- Assess perioperative cardiac risk.
- Perform risk stratification with RCRI.
- If RCRI ≥1, or patient is ≥65 years, or age 45-64 years with significant cardiovascular disease:
- Order NT-proBNP/BNP.
Postoperative Monitoring
-
Positive NT-proBNP/BNP:
- Measure troponin daily for 48-72 hours.
- Obtain ECG in PACU.
- Consider in-hospital shared-care management.
-
NT-proBNP/BNP Not Available:
- Measure troponin daily for 48-72 hours.
- Obtain ECG in PACU.
- Consider in-hospital shared-care management.
-
Negative NT-proBNP/BNP:
- No additional routine postoperative monitoring.
This flowchart and guideline offer a comprehensive approach for assessing perioperative cardiac risk and determining the need for postoperative monitoring based on individual patient risk factors and surgery type.
Management of Interventions Targeting the Prevention of Perioperative Cardiac Events
Management of Chronic Medications and Smoking Before Non-Cardiac Surgery
ASA (Acetylsalicylic Acid)
- Withhold at least 3 days before surgery.
- Restart ASA when the risk of bleeding related to surgery has passed (i.e., 8-10 days after major non-cardiac surgery).
β-Blocker
- Continue β-blocker during the perioperative period.
- If the patient’s systolic blood pressure is low before surgery, consider decreasing or holding the dose of the β-blocker.
ACEI/ARB (Angiotensin-Converting Enzyme Inhibitor/Angiotensin II Receptor Blocker)
- Withhold ACEI/ARB 24 hours before non-cardiac surgery.
- Restart ACEI/ARB on day 2 after surgery if the patient is hemodynamically stable.
Statin
- Continue statin during the perioperative period.
Smoking
- Discuss and facilitate smoking cessation, ideally starting ≥4 weeks before surgery (e.g., nicotine replacement therapy).
Initiation of New Medications and Coronary Revascularization Before Non-Cardiac Surgery
ASA
- Do not initiate ASA for the prevention of perioperative cardiac events.
β-Blocker
- Do not initiate a β-blocker within 24 hours before non-cardiac surgery.
α(_2)-Agonist
- Do not initiate an α(_2)-agonist for the prevention of perioperative cardiovascular events.
Calcium Channel Blocker
- Do not initiate a calcium channel blocker for the prevention of perioperative cardiovascular events.
Coronary Revascularization
- Do not undertake preoperative prophylactic coronary revascularization for patients with stable coronary artery disease.
Special Considerations
- Unstable CAD: Individualized risk/benefit assessment of revascularization and delay (procedure + post-revascularization and DAPT) vs. expediting the non-cardiac surgery.
Note:
- These guidelines apply to patients aged ≥45 years with significant cardiovascular disease or aged 18-44 years with severe obstructive intracardiac abnormality undergoing non-cardiac surgery requiring hospital admission.
- Individualized assessment is necessary for patients with recent coronary artery stents or those undergoing high-risk surgeries such as carotid endarterectomy.
CAD for Non-Cardiac Surgery Recommendations
- Either Volatile or TIVA.
- Neuraxial for post-op analgesia in aortic surgery, pre-op for hip fracture.
- TEE if hemodynamically unstable.
- Normothermia maintenance.
- Hemodynamic assist devices if hemodynamically unstable.
- PAC when underlying medical conditions affecting hemodynamics cannot be corrected pre-op.
- Not recommended:
- Routine TEE.
- Routine PAC.
- Prophylactic nitroglycerin.
Paediatric Considerations
Major Physiological Status Risk Factors
-
Cardiac Failure:
- Signs: Raised HR + RR, sweating, cool peripheries, hepatomegaly, failure to thrive, poor feeding.
- Risk: 10% cardiac arrest, 96% inotropic support (less if HF milder).
- Anaesthesia: Prolonged induction time, avoid prolonged use of 8% sevo, avoid propofol.
-
Pulmonary Hypertension (PHTN):
- Risk: 8 times more likely to have a major complication.
- Anaesthesia: Reduced pulmonary compliance + increased airway resistance, respiratory tract infections poorly tolerated.
-
Arrhythmia:
- Risk: Ventricular ectopics = ominous sign, 30% die suddenly.
- Single ventricle circulation: 30% risk of arrhythmia leading to death.
-
Cyanosis:
- Risk: Polycythemia = hyperviscosity, cerebral vein and sinus thrombosis (worsened by dehydration).
- Coagulopathy: Abnormal clotting in 20% (platelet dysfunction, thrombocytopenia, clotting factor reduction).
Factors Associated with Increased Risk of Complications
- Disease complexity (single ventricle, balanced, cardiomyopathy, aortic stenosis).
- Physiological status.
- Type of surgery (intraperitoneal, intrathoracic, vascular, cross-matched blood required, emergency).
- Young age (<6 months, even up to 2 years risk may be higher).
- Syndromic conditions.
Links
Past Exam Questions
Dual Anti-Platelet Therapy (DAPT) Following Percutaneous Intervention (PCI)
a) With regards to Dual Anti-Platelet Therapy (DAPT) following a Percutaneous Intervention (PCI), how long should DAPT be administered for? (2)
b) Explain how you would determine which patients can deviate from the above stipulated duration of therapy and the Grade/level of evidence supporting this decision. (8)
Preoperative Cardiac Risk Assessment for a Complex Fistula Repair
A 64-year-old man is planned for a multidisciplinary procedure to correct a complex fistula post-prostatectomy which he had a year earlier. The procedure is expected to be prolonged. He has Type 2 Diabetes and is using insulin. He is also treated with three agents for hypertension. The patient had an ST elevation myocardial infarction 5 years ago for which a stent was inserted in the left circumflex coronary artery. He was on anticoagulation treatment for 3 months. The patient defaulted on cardiology follow-up because he was asymptomatic. On examination, he is able to climb two flights of stairs unassisted, and his pre-operative ECG reveals a Mobitz Type 2 block.
a) Discuss this patient’s pre-operative cardiac risk. (5)
b) What precautions will you take before embarking on the anaesthetic for this patient? (5)
—
References:
- Smilowitz NR, Berger JS. Perioperative Cardiovascular Risk Assessment and Management for Noncardiac Surgery: A Review. JAMA. 2020;324(3):279–290. doi:10.1001/jama.2020.7840
- Sigrun Halvorsen, Julinda Mehilli, Salvatore Cassese et al. ESC Scientific Document Group, 2022 ESC Guidelines on cardiovascular assessment and management of patients undergoing non-cardiac surgery: Developed by the task force for cardiovascular assessment and management of patients undergoing non-cardiac surgery of the European Society of Cardiology (ESC) Endorsed by the European Society of Anaesthesiology and Intensive Care (ESAIC), European Heart Journal, Volume 43, Issue 39, 14 October 2022, Pages 3826–3924, https://doi.org/10.1093/eurheartj/ehac270
- Alphonsus, C S et al. South African cardiovascular risk stratification guideline for non-cardiac surgery. South African Medical Journal, [S.l.], v. 111, n. 10b, oct. 2021. ISSN 2078-5135. Available at: <http://www.samj.org.za/index.php/samj/article/view/13424/9975>.
- A practical approach to perioperative risk optimisation for non-cardiac surgery. I Cassimjee University of the Witwatersrandhttps://orcid.org/0000-0001-7074-9752
- Bhave, N. M., Cibotti-Sun, M., & Moore, M. M. (2024). 2024 perioperative cardiovascular management for noncardiac surgery guideline-at-a-glance. Journal of the American College of Cardiology. https://doi.org/10.1016/j.jacc.2024.08.018
- Thompson, A., Fleischmann, K. E., Smilowitz, N. R., de las Fuentes, L., Mukherjee, D., Aggarwal, N. R., … & Williams Sr., K. A. (2024). 2024 aha/acc/acs/asnc/hrs/sca/scct/scmr/svm guideline for perioperative cardiovascular management for noncardiac surgery: a report of the american college of cardiology/american heart association joint committee on clinical practice guidelines. Circulation. https://doi.org/10.1161/cir.0000000000001285
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “c935448f-615a-43c8-b7e6-64ad21abd549”



