{}
Oesophagectomy
Introduction
- Epidemiology: Oesophageal cancer is the eighth most common malignancy worldwide with an increasing incidence. At initial presentation, 20-30% of patients have metastases.
- Surgical Procedure:
- Involves excision of the oesophagus and relocation of the stomach in the mediastinum to form a gastric conduit connecting the pharynx to the remaining gastrointestinal (GI) tract, with the abdominal stage performed first.
- The anastomosis is at the extreme end of the foregut’s blood supply, making it vulnerable to ischaemia without careful management of haemodynamic parameters and fluid to ensure its perfusion.
- In revision oesophagectomy, a colonic interposition is performed using a section of the colon on a pedicle.
- This is a high-risk procedure with multiple vulnerable anastomoses.
Considerations
- High Risk for Postoperative Morbidity & Mortality:
- Identify surgical approach & associated considerations.
- Possible need for lung isolation.
- Comorbid Disease Processes:
- Full stomach & high risk for aspiration.
- Malnourishment, deconditioning, anemia, coagulopathy.
- Smoker, chronic obstructive lung disease, coronary artery disease, hypertension, diabetes mellitus.
- Cancer 4M’s:
- Mass effects, medications, metastases, metabolic abnormalities.
- Prolonged Surgery with Severe Hemodynamic Insults:
- Need for invasive monitors & access.
- Lung protective ventilation.
- Maintenance of Anastomotic Integrity:
- Thoracic epidural anesthesia.
- Judicious fluid administration & vasopressor usage.
- Optimize oxygen delivery.
Risk Factors for Perioperative Morbidity & Mortality
- Poor cardiac and/or pulmonary function.
- Advanced age.
- Tumour stage.
- Diabetes mellitus.
- Impaired general health.
- Hepatic dysfunction.
- Peripheral vascular disease.
- Smoker.
- Chronic use of steroids.
Goals & Conflict
Preoperative
- Assessment of 4M’s:
- Optimization of comorbidities.
- Planning for postoperative care.
- Optimization:
- Smoking cessation.
- Correct/optimise anemia.
- Nutrition: Patients may be cachectic or obese, but even obese patients may be malnourished due to hypermetabolic state.
- Patients taking <75% of caloric goals require supplementation.
- Patients taking less than 50% of caloric goals require tube feeds.
- Rehabilitation with physiotherapy is emerging.
Intraoperative
- Aspiration Prophylaxis:
- Rapid sequence induction (RSI) due to high risk of aspiration.
- Thoracic epidural.
- Arterial & central venous access, large bore IV access.
- Lung isolation & lung protective ventilation.
- Planning for repositioning.
- Preparations for severe hemodynamic instability, especially during blunt mediastinal dissection.
- Restrictive fluid strategy with vasopressors as needed to treat epidural-related vasoplegia.
Evidence-based Strategies
- Avoiding large volumes of fluid.
- Extubation in theatre.
- Regional analgesia (Thoracic Epidural Analgesia > Paravertebral Block).
- Lung protective ventilation.
Surgical Approach
- Ivor Lewis: Laparotomy, right thoracotomy.
- Transhiatal: Laparotomy, left neck.
- Three-hole: Laparotomy, thoracotomy, and cervical incision.
- Left Thoracoabdominal: Combined thoracic and abdominal incision.
- Laparoscopic/Thoracoscopic: Minimally invasive techniques.
Surgical Considerations
- Prolonged surgery.
- Need for one lung ventilation.
- Intraoperative repositioning.
- Hemodynamic instability: Intrathoracic dissection, supraventricular arrhythmias.
- No vascular access in left neck.
Postoperative
- Greatest mortality risk of all thoracic surgery.
- Attempt postoperative extubation and plan for high care stay.
- Monitor for
- Aspiration pneumonia.
- Respiratory failure.
- Anastomotic dehiscence with empyema.
- Mediastinitis.
- Septic shock.
- Arrhythmias.
- Congestive heart failure (CHF).
Evidence-based Strategies
- Adequate analgesia.
- Reversal of neuromuscular blocking agents (NDMR).
- Normothermia.
- Haemodynamic stability.
Conduct of Anaesthesia for Oesophagectomy
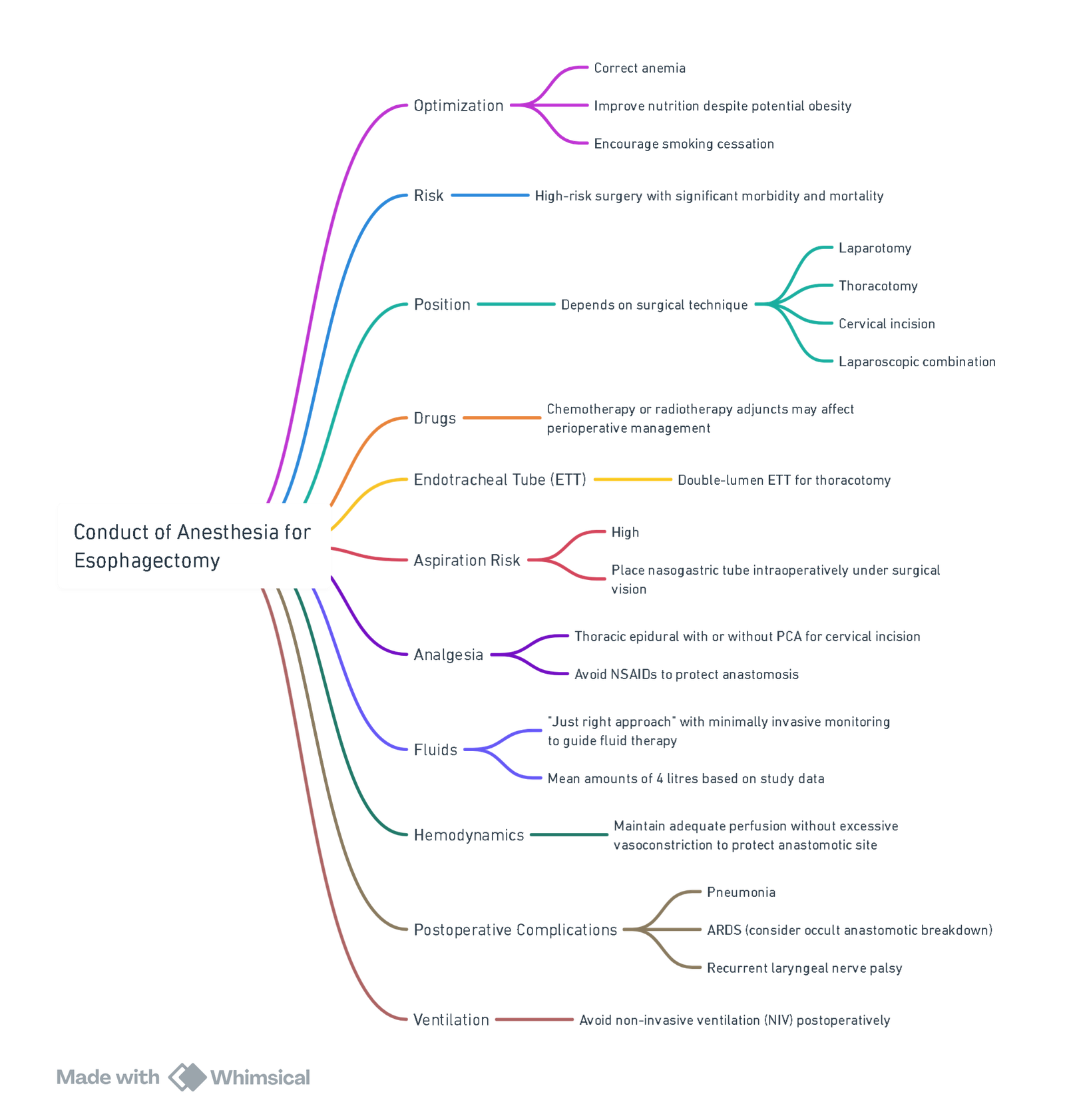
View or edit this diagram in Whimsical.
Oesophageal Injury
Introduction
- Causes:
- Spontaneous perforations, trauma, or iatrogenic perforations (60%).
- Most common sites: Level of the cricopharyngeus and proximal to the lower oesophageal sphincter due to angulation of the hiatus and increased pathology such as oesophageal webs, rings, and strictures.
Pathophysiology
- Oesophageal rupture allows food, gastric contents, secretions, and air to enter the mediastinum, leading to contamination, mediastinal emphysema, inflammation, and necrosis.
- Perforation of the overlying pleura allows oesophageal contents to enter the pleural space, causing pleural cavity contamination and pleural effusion, usually on the left.
Time to Treatment
- Time from injury to treatment initiation is crucial:
- Mortality with treatment delayed >24 hours: 27%.
- Mortality with treatment <24 hours: 14%.
Cause of Death
- Most common causes: Pneumothoraces, mediastinitis, and pleural effusions.
Management of Acute Oesophageal Perforation
-
Initial Assessment:
- Clinical examination.
- Fluid resuscitation.
- Diagnostic imaging: CXR, CT, oesophagography, endoscopy.
-
Leak Type Determination:
- Contained or Limited Leak:
- Non-operative Management:
- Medical management with monitoring.
- Minimally invasive interventions if deterioration occurs.
- Operative Management:
- Primary repair if suitable.
- Controlled fistula or resection if unsuitable for primary repair.
- Non-operative Management:
- Contained or Limited Leak:
Anaesthetic Considerations
- Septic Shock: Possible due to mediastinal contamination.
- Aspiration Risk: High; minimize coughing and straining to avoid worsening injury.
- Cricoid Pressure: Controversial.
- Airway Management:
- Secure airway and place nasogastric tube in proximal oesophagus above the injury.
- Surgeon will position the NG tube beyond the repaired oesophagus during surgery to keep the stomach decompressed.
- NG tube not used for enteral nutrition; use jejunostomy instead.
- Lung Isolation: Required.
- Normothermia: Maintain using a forced air device and warmed IV fluids (goal-directed).
Positioning
- Varies with pathology and surgical approach:
- Lateral position for primary repair, thoracoscopy, or open thoracotomy.
- Upper arm abducted for surgical access, avoid excessive stretch on brachial plexus.
- Avoid corneal abrasions.
- Frequent intraoperative repositioning may be needed, ensuring tube position is rechecked.
Analgesia
- Thoracic epidural analgesia.
- Multimodal analgesia (MMA).
- Paravertebral block.
Postoperative Management
- Includes broad-spectrum antibiotics and monitoring for sepsis.
- Evaluate for possible collections or leakage with ultrasound or CT.
- Gastrografin contrast study 2-3 weeks post-repair to check for ongoing leaks.
- If T-tube in place, perform contrast swallow to check for leaks before removal at 8-10 weeks post-operation.
Links
- Mediastinal masses
- Lower GIT surgery
- Tracheal surgery
- Thoracic pre-op assessment
- Head and neck surgery
References:
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- King, W. and Dickinson, M. (2015). Oesophageal injury. BJA Education, 15(5), 265-270. https://doi.org/10.1093/bjaceaccp/mku039
- Howells, P., Bieker, M., & Yeung, J. (2017). Oesophageal cancer and the anaesthetist. BJA Education, 17(2), 68-73. https://doi.org/10.1093/bjaed/mkw037
Summaries:
TOF
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “267dc8ef-06f1-4bab-a44f-158bf4e17be4”



