{}
Acute Rheumatic Fever
Pathogenesis and Clinical Findings
Overview
- Pathogenesis:
- Untreated GAS Pharyngitis
- Environmental Factors
- Genetic Susceptibility
Pathogenesis
- Initial Event:
- Untreated Group A Streptococcus (GAS) pharyngitis
- Delayed Autoimmune Reaction:
- Triggered by molecular mimicry where GAS antigen cross-reacts with host tissues
- Activation of Immune Response:
- Activation of auto-reactive B and CD-4+ T cells
- Tissue Injury and Inflammation:
- Outcomes:
- Clinical Findings:
- Fever
- Arthralgia
- Erythema Marginatum
- Subcutaneous Nodules (Osler’s Nodes)
- Increased ESR and CRP
- Mechanisms:
- Antibodies recognize ganglioside and N-acetyl-β-D-glucosamine, targeting neuronal cell surfaces, leading to Sydenham’s Chorea via cell signaling and dopamine release.
- Antibodies attach to myosin and other cardiac proteins. Lymphocytes adhere to these proteins causing pancarditis and valvular injury, resulting in carditis and prolonged PR interval.
- Clinical Findings:
- Outcomes:
Genetic and Environmental Factors
- Genetic Susceptibility:
- Polygenic, involving HLA-DR7 and other class II MHC alleles.
- Single nucleotide polymorphisms (SNPs) for TNF-alpha and Mannan-binding lectin.
- Environmental Risk Factors:
- Overcrowding
- Poverty
- Malnutrition
- Maternal unemployment
- Low level of maternal education
Prevention
- Treatment of GAS pharyngitis with a full course of antibiotics can reduce the risk of developing rheumatic fever.
Long-term Sequelae
- Rheumatic heart disease, commonly valvulopathy.
- Jaccoud arthropathy: a benign chronic arthropathy causing joint and tendon loosening in hands/feet.
Introduction and Epidemiology

View or edit this diagram in Whimsical.
Diagnosis
- Definition of Low-Risk Population:
- Cases of acute RF ≤ 2/100,000 school-age children or rheumatic heart disease.
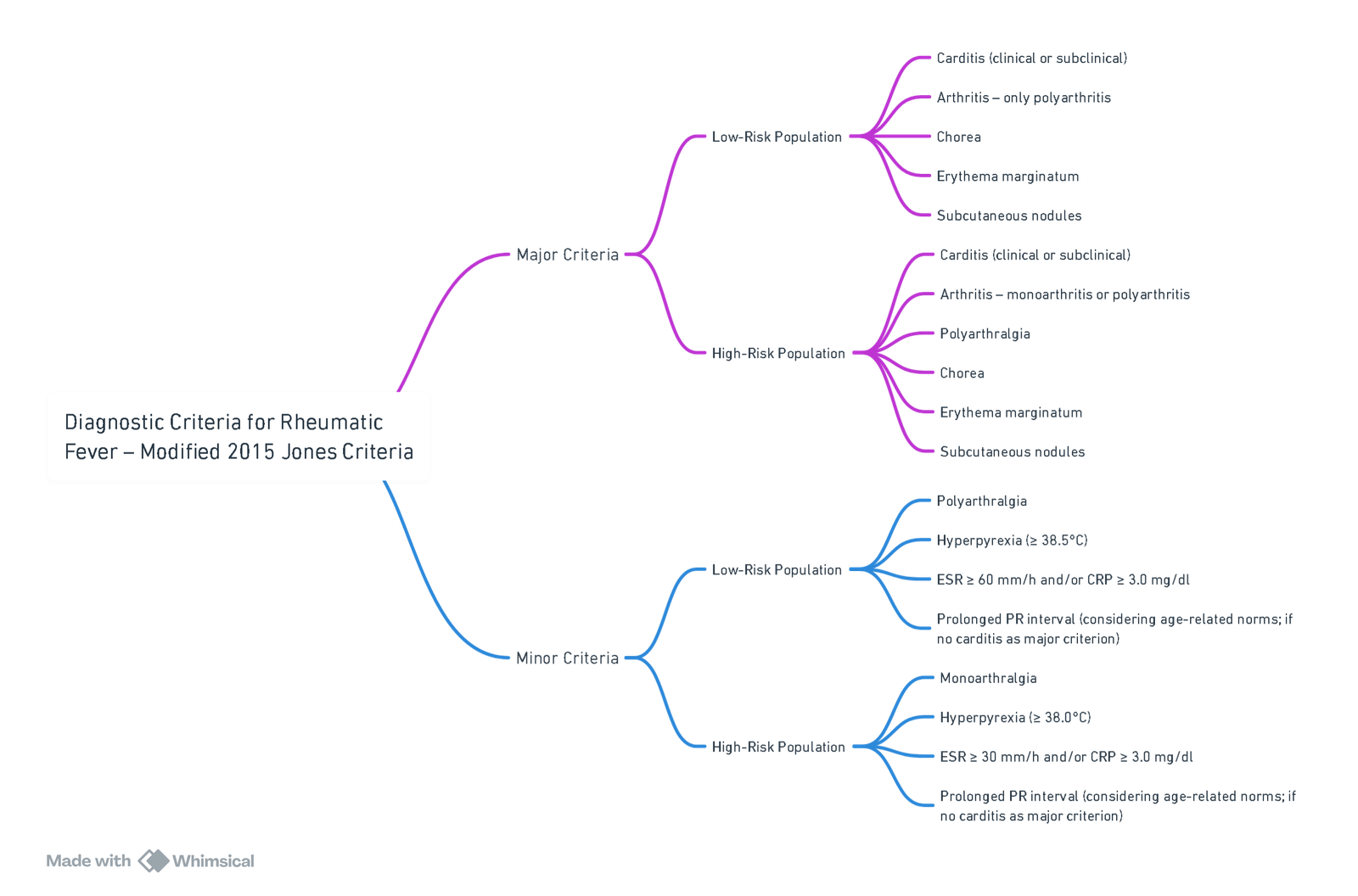
- Cases of acute RF ≤ 2/100,000 school-age children or rheumatic heart disease.
View or edit this diagram in Whimsical.
Echocardiographic Criteria (AHA 2012)
Doppler Criteria
-
Pathological Mitral Regurgitation (all must be met):
- Visible in at least 2 projections.
- Regurgitation jet length ≥ 2 cm in at least 1 projection.
- Regurgitation peak velocity > 3 m/s.
- Regurgitation pansystolic.
-
Pathological Aortic Regurgitation (all must be met):
- Visible in at least 2 projections.
- Regurgitation jet length ≥ 1 cm in at least 1 projection.
- Regurgitation peak velocity > 3 m/s.
- Regurgitation pandiastolic.
Morphological Criteria
-
Acute Mitral Valve Involvement:
- Dilatation of mitral annulus.
- Elongation of chordae tendineae.
- Rupture of chorda tendinea with acute mitral regurgitation.
- Prolapse of anterior (less often posterior) leaflet.
- Nodular lesions on leaflets.
-
Chronic Mitral Valve Involvement:
- Thickening of leaflets.
- Thickening and fusion of chordae tendineae.
- Limited leaflet mobility.
- Calcifications.
-
Acute and Chronic Aortic Valve Involvement:
- Symmetrical or focal thickening of leaflets.
- Disturbed leaflet coaptation.
- Limited leaflet mobility.
- Prolapse of leaflets.
Treatment
Primary Prevention
- Indication: Treatment of group A streptococcal (GAS) pharyngitis to prevent the first episode of acute rheumatic fever (ARF).
- Preferred Agent:
- Phenoxymethylpenicillin (Penicillin V)
- Dose: 500 mg orally twice daily for 10 days (250 mg for children <27 kg).
- Phenoxymethylpenicillin (Penicillin V)
- Penicillin Allergy (non-anaphylactic)
- First-generation cephalosporins (e.g., cephalexin).
- Penicillin Allergy (anaphylactic):
- Macrolides (e.g., azithromycin or erythromycin).
Secondary Prevention
- Goal: Prevent recurrence of ARF and progression to chronic RHD.
- Preferred Agents:
- Benzathine benzylpenicillin IM every 3–4 weeks (first-line).
- Phenoxymethylpenicillin orally twice daily.
- Macrolides if allergic to penicillin.
- Dosage:
- Phenoxymethylpenicillin: 250 mg orally twice daily.
Duration of Secondary Prophylaxis
-
Without carditis:
- Until 21 years of age or 5 years after last ARF episode, whichever is longer.
-
With carditis but no residual valvular disease:
- Until 25 years of age or 10 years after last ARF, whichever is longer.
-
With carditis and persistent valvular heart disease:
- Until 40 years of age or 10 years after last ARF, whichever is longer; some guidelines recommend lifelong prophylaxis.
Anti-inflammatory Treatment
- Prednisone:
- Dosage: 1–2 mg/kg/day for 2–3 weeks, then taper gradually.
- Total duration: 6 weeks.
Links
- Infective endocarditis
- Valvular heart disease
- Cardiac physiology
- Cardiac disease in pregnancy
- Anaesthetic management of specific cardiac conditions
References:
- Szczygielska, I., Hernik, E., Kołodziejczyk, B., Gazda, A., Maślińska, M., & Gietka, P. (2018). Rheumatic fever–new diagnostic criteria. Rheumatology, 56(1), 37-41. https://doi.org/10.5114/reum.2018.74748
- The Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “371d27a1-1648-49bd-9eed-ef1d800d9625”



