{}
Acute & Chronic Spinal Cord Injury (SCI)
Pathophysiology
Primary Injury
- Mechanical insult–traction, compression, shear or laceration destroys grey/white-matter tracts.
Secondary Injury (minimise intra-theatre)
- Within minutes–weeks: spinal cord ischaemia, glutamate excitotoxicity, inflammatory cytokine surge, oedema, free-radical formation and delayed apoptosis
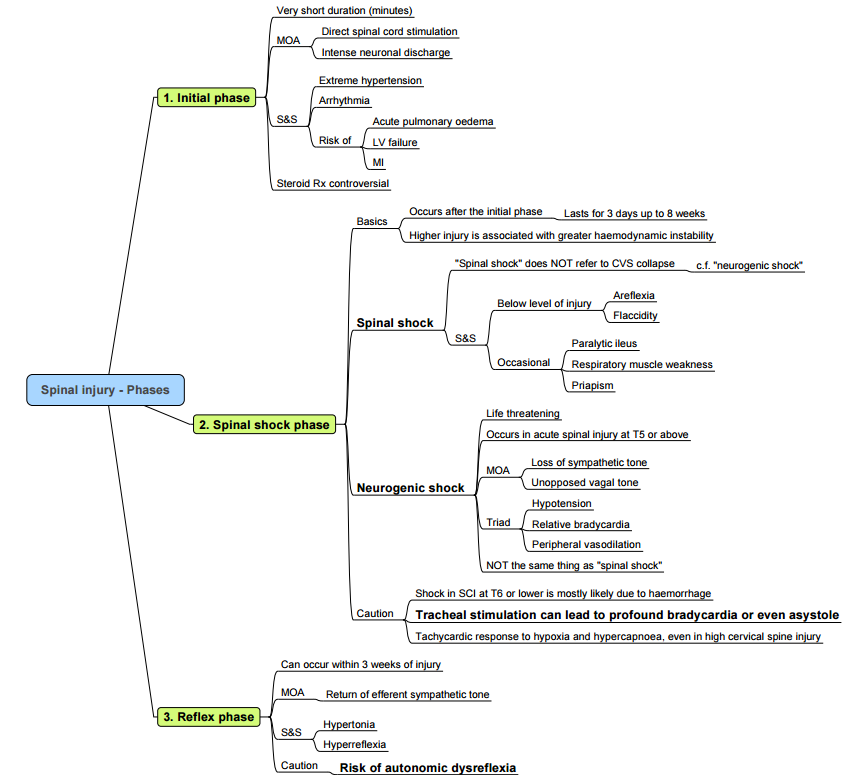
Phases after Injury
| Phase | Timing | Key features | Anaesthetic relevance |
|---|---|---|---|
| Initial | Seconds–minutes | Transient extreme sympathetic discharge → severe hypertension, arrhythmia, APO | Treat as hypertensive crisis; invasive BP if unstable |
| Spinal-shock | ~30 min–8 weeks | Areflexia, flaccidity, paralytic ileus; variable hypotension/bradycardia | Expect haemodynamic lability; avoid high PEEP which ↓ venous return |
| Neurogenic-shock | Usually cervical/high-thoracic injuries within first 24 h | Triad: hypotension, relative bradycardia, peripheral vasodilation | Maintain MAP ≥ 85 mmHg for 5–7 days with fluids + noradrenaline/phenylephrine |
| Reflex/Spastic | ≥ 3 weeks | Return of reflex arcs, spasticity; risk of autonomic dysreflexia (AD) above T6 | Anticipate severe peri-operative hypertension/tachy-/brady-arrhythmias |
Key Distinctions between Spinal Shock and Neurogenic Shock
| Aspect | Spinal shock | Neurogenic shock |
|---|---|---|
| Primary phenomenon | Neurological: transient loss of all motor, sensory and reflex activity below the level of injury | Haemodynamic: distributive shock from loss of sympathetic tone (vasodilatation ± bradycardia) |
| Typical cord level | Any; severity ↑ with high cervical injuries | Almost always lesions above T6 (loss of splanchnic sympathetic outflow) |
| Pathophysiology | Sudden interruption of descending facilitatory pathways → flaccid areflexia; gradual synaptic re-organisation leads to hyper-reflexia/spasticity | Loss of vasomotor tone + unopposed vagal cardiac influence → ↓ SVR, venous pooling, relative bradycardia |
| Onset | Immediate (seconds–minutes) after injury | Usually within hours of injury (can be delayed) |
| Duration | Hours → weeks (resolution heralded by bulbocavernosus reflex & return of deep-tendon reflexes) | Days → up to 6 weeks; resolves with sympathetic re-adaptation or after vasopressor support |
| Cardiovascular signs | BP normal or ↓ (if coincident neurogenic shock), heart rate often normal or tachycardic initially | Hypotension with relative bradycardia (HR < 60–80 bpm), warm peripheries, wide pulse pressure |
| Neurological signs | Flaccid paralysis, areflexia, sensory loss below lesion | May have motor/sensory loss (from SCI) but reflexes unaffected by the shock state |
| Temperature regulation | Usually normal initially; later poikilothermia as reflexes return | Impaired–patient tends to assume ambient temperature owing to vasodilatation |
| Core management | Supportive; prevent secondary cord injury (MAP ≥ 85 mmHg, oxygenation) | Fluid resuscitation + vasopressor (noradrenaline/phenylephrine); atropine/isoprenaline for severe bradycardia; treat hypothermia |
| Prognosis marker | Return of reflexes → phase-2 recovery; eventual spasticity/hyper-reflexia | Responds rapidly to haemodynamic optimisation; mortality increases if unrecognised |
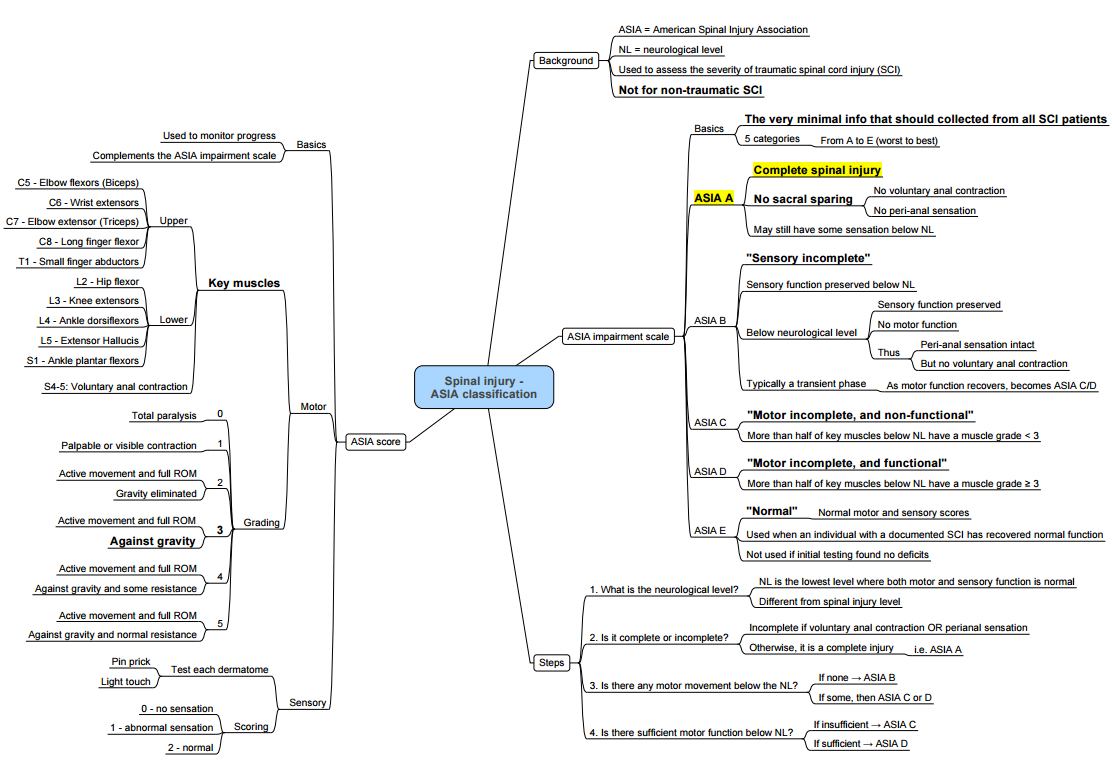
Classification
American Spinal Injury Association (ASIA) Impairment Scale (AIS)
| Grade | Description |
|---|---|
| A–Complete | No motor/sensory function in S4–S5 |
| B–Sensory incomplete | Sensory but no motor below lesion incl. S4–S5 |
| C–Motor incomplete | < 50 % key muscles below lesion grade ≥ 3 |
| D–Motor incomplete | ≥ 50 % key muscles below lesion grade ≥ 3 |
| E–Normal | Normal exam; prior deficits present |
The neurological level = lowest level with intact motor and sensory bilaterally.
Key Syndrome Patterns
| Syndrome | Typical cause | Ipsilateral loss | Contralateral loss |
|---|---|---|---|
| Brown-Séquard | Penetrating hemi-cord injury | Motor, vibration, proprioception | Pain & temperature |
| Anterior cord | Anterior spinal artery occlusion | Motor, pain, temperature | — |
| Central cord | Hyper-extension in spondylotic neck | Upper-limb > lower-limb weakness, +/- bladder retention | Variable |
| Posterior cord | Posterior spinal artery / B12 | Proprioception & vibration | — |
| Conus medullaris | L1 fracture, tumour | Mixed UMN/LMN; early sphincter dysfunction | — |
| Cauda equina | Large central disc, fracture | LMN pattern; patchy | — |
Respiratory Consequences
| Injury level | Vital capacity (% predicted) | Cough | Ventilatory support |
|---|---|---|---|
| C1–C2 | < 10 % | Absent | Permanent invasive ventilation |
| C3–C5 (phrenic) | 10–30 % | Ineffective | 80 % need ventilation within 48 h; consider NIV wean |
| Above T8 | 30–80 % | Weak | May require short-term ventilation/assisted cough |
| Below T8 | 80–100 % | ± weak | Rarely ventilated |
Early chest physiotherapy, cough assist and physiologic PEEP reduce pneumonia and atelectasis
Anaesthetic Management
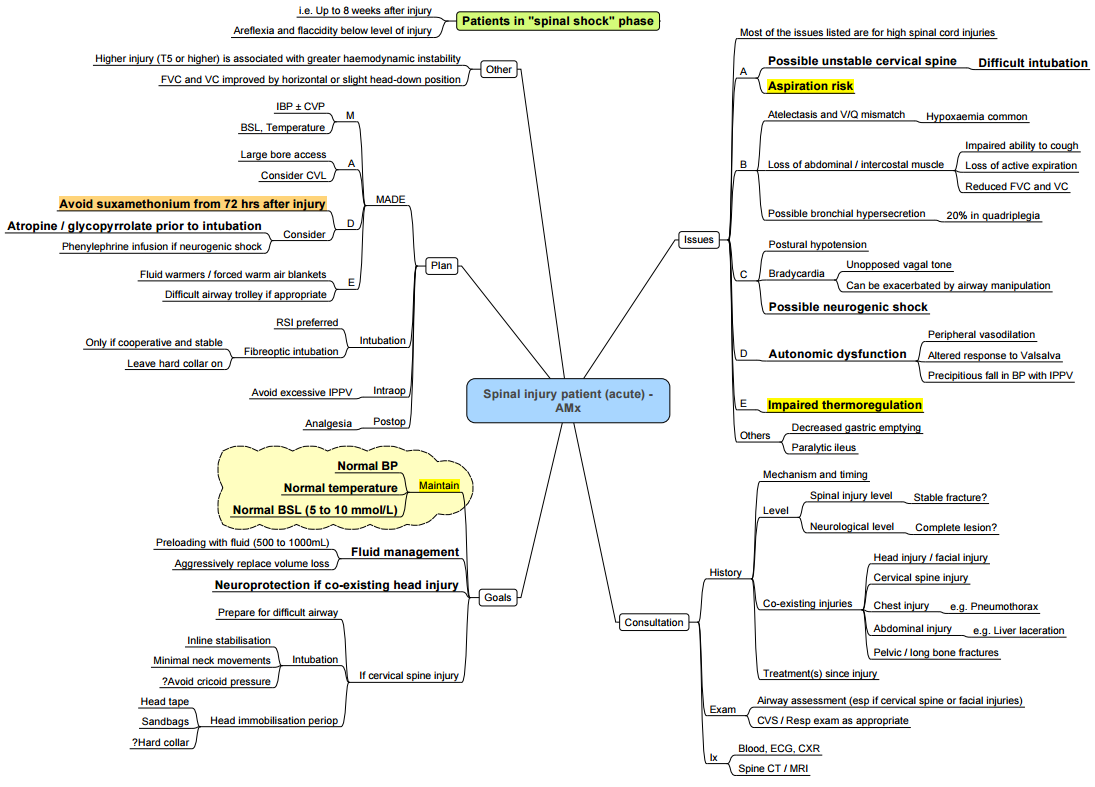
Pre-operative Assessment (ATLS framework)
- Airway–anticipate difficult intubation (rigid collar, limited jaw movement, chronic spasm).
- Breathing–evaluate FVC, peak cough flow; baseline ABG.
- Circulation–exclude haemorrhage; recognise neurogenic shock.
- Disability–document motor level (medico-legal).
- Exposure–pressure-area check, temperature, spasm trigger survey.
Pharmacology Pearls
| Drug/class | Evidence-based recommendation |
|---|---|
| Succinylcholine | Safe ≤ 48 h post-injury only; thereafter contra-indicated until ~9 months owing to lethal hyperkalaemia from ACh-receptor up-regulation |
| Non-depolarising NMB | Rocuronium 1 mg kg⁻¹ RSI; expect resistance in chronic phase (↑ dose/early sugammadex) |
| High-dose methyl-prednisolone | Not recommended–no neurological benefit, ↑ infection & GI bleeding risk |
| Vasopressors | Noradrenaline first-line; phenylephrine for episodic AD |
Induction & Positioning
- Manual in-line stabilisation; avoid cricoid pressure unless gastric distension.
- If awake fibre-optic needed, lignocaine 4 mg kg⁻¹ nebuliser; maintain collar.
- Warm IV fluids & forced-air blankets–impaired thermoregulation.
- Confirm BP after every position change–drastic swings common.
Maintenance Goals (“MADE”)
- M: MAP ≥ 85 mmHg.
- A: Anaemia–keep Hb > 10 g dl⁻¹ (optimises DO₂).
- D: Dysreflexia–deep anaesthesia, α-blocker (phentolamine 5 mg IV) for crises.
- E: Euthermia–36–37 °C; treat pyrexia vigorously
Autonomic Dysreflexia (chronic ≥ T6)
- Triggers: bladder/kidney stones, distended colon, labour, surgical incision.
- Presentation: SBP ↑ > 20 %, pounding headache, sweating above lesion, reflex bradycardia.
- Immediate treatment: remove stimulus, deepen anaesthesia, give GTN 2 puffs SL / nicardipine 0.5 µg kg⁻¹ min⁻¹ infusion
Ventilation
- Vₜ 6 ml kg⁻¹, permissive hypercapnia avoided (↑ ICP in concomitant TBI).
- Assisted cough (MI-E device) before extubation.
Thromboprophylaxis
- Start LMWH within 24–72 h once haemostasis secure; continue ≥ 3 months or until ambulatory. Early initiation halves VTE risk
- Add intermittent pneumatic compression.
Post-operative Priorities
- Haemodynamic monitoring for 24 h (invasive if high cervical).
- Strict temperature charting–treat poikilothermia.
- Early mobilisation/tilt-table.
- Multimodal analgesia: paracetamol, ketamine 0.1 mg kg⁻¹ h⁻¹, gabapentinoids for neuropathic pain.
- Pressure-area care checklist each nursing shift.
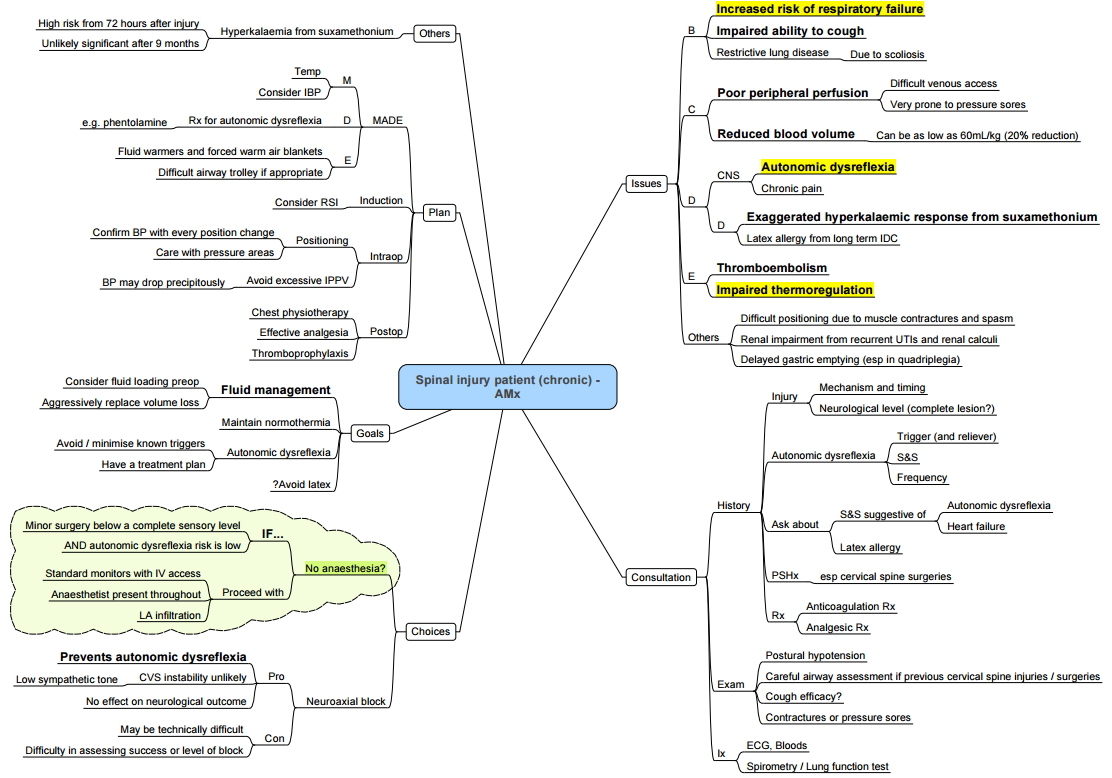
Elective / Chronic SCI Specifics
| Issue | Practical tip |
|---|---|
| Respiratory failure risk | Pre-hab with inspiratory-muscle training; plan for NIV post-op if FVC < 50 % predicted |
| Difficult IV access & reduced blood volume (~20 %) | Ultrasound lines, preload 2 ml kg⁻¹ h⁻¹ balanced crystalloids |
| Spasm & contractures | Positioning aids, baclofen pre-med |
| Latex allergy (chronic IDC) | Use latex-free equipment |
| Thermoregulation | Active warming & ambient 24 °C |
| Neurological monitoring for regional | Sensory testing unreliable below lesion; use US guidance for neuraxial/plexus blocks. |
- Minor procedures below the sensory level with low AD risk can occasionally proceed with local infiltration alone, provided IV access, standard monitors and an anaesthetist remain present throughout.
Disc Herniation
- Degenerative loss of proteoglycans → nucleus pulposus dehydration → annular tears.
- Lumbar L4/5 & L5/S1 90 %; Cervical C6/7 60 %.
- Lateral herniation → radiculopathy / cauda equina; central cervical → myelopathy.
- Anaesthetic relevance: optimise neurological exam pre-block; avoid excessive neck flexion.
American Spinal Injury (ASIA) Impairment Scale
Links
References:
- Dooney N, Dagal A. Anesthetic considerations in acute spinal cord trauma. Int J Crit Illn Inj Sci. 2011 Jan;1(1):36-43. doi: 10.4103/2229-5151.79280. PMID: 22096772; PMCID: PMC3210001.
- Bonner, S. and Smith, C. (2013). Initial management of acute spinal cord injury. Continuing Education in Anaesthesia Critical Care &Amp; Pain, 13(6), 224-231. https://doi.org/10.1093/bjaceaccp/mkt021
- Badhiwala JH et al. A clinical practice guideline for acute SCI: haemodynamic management. Global Spine J 2022. PMC
- Levi AD. Mean arterial pressure targets and neurologic recovery after SCI. Neurosurgery 2020. PubMed
- StatPearls. Succinylcholine Chloride (update 2025). OpenAnesthesia
- Yang J et al. Peri-operative autonomic dysreflexia review. J Anaesth Crit Care 2024. PMC
- OpenAnesthesia. Spinal cord injury–key points (2023). OpenAnesthesia
- SurgicalCriticalCare.net guideline: High-dose methylprednisolone NOT recommended (2023). Surgical Critical Care
- Medscape Reference. Corticosteroids in acute SCI (2023 update). Medscape
- PVA Consortium. Early acute management in adults with SCI (2019). Paralyzed Veterans of America
- Cardenas DD et al. Anticoagulant thromboprophylaxis after SCI. Global Spine J 2020. College of Medicine
- West CR et al. Respiratory complications in chronic SCI. BJA 2019. OpenAnesthesia
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “c8854421-a0ef-4cd7-b2cb-b51f812a729d”



