{}
Autonomic Neuropathy
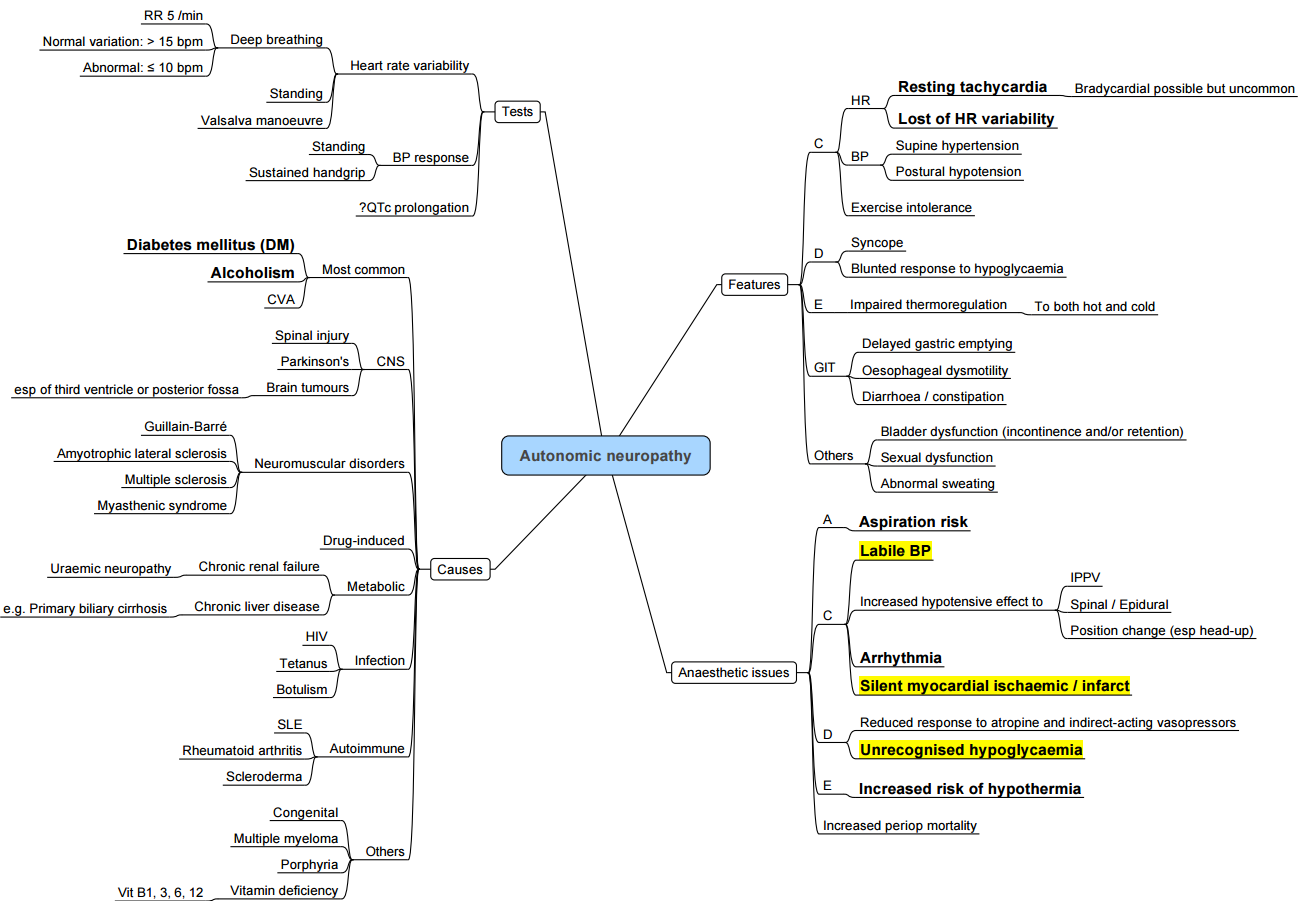
Diabetic Autonomic Neuropathy
Diagnosis of Diabetic Neuropathy
Tests Evaluating Cardiac Parasympathetic Function
- Heart rate response to Valsalva manoeuvre
- Heart rate variation during deep breathing
- Immediate heart rate response to standing
Tests Evaluating Cardiac Sympathetic Function
- Blood pressure response to standing
- Blood pressure response to sustained handgrip
Recommendations by Ewing and Clark
Ewing and Clark recommend that all five tests should be conducted to gather comprehensive information about both parasympathetic and sympathetic pathways.
Results are categorized into one of four categories:
- Normal: No tests abnormal.
- Early parasympathetic damage: At least one test abnormal.
- Definite parasympathetic damage: At least two tests abnormal.
- Combined parasympathetic and sympathetic damage: Positive results in both categories.
Clinical Manifestations of Diabetic Neuropathy
| System | Symptoms |
|---|---|
| Cardiovascular | Postural hypotension, Labile blood pressure, Tachycardia, Supine hypertension, Paroxysmal hypertension, Bradycardia |
| Sudomotor | Hypoor anhidrosis, Gustatory sweating, Hypothermia, Hyperpyrexia, Hyperhidrosis, Heat intolerance |
| Alimentary | Xerostomia, Gastric stasis, Constipation, Dysphagia, Dumping syndromes, Diarrhoea |
| Urinary | Nocturia, Urgency; retention, Frequency, Incontinence |
| Sexual | Erectile failure, Retrograde ejaculation, Ejaculatory failure, Priapism |
| Eye | Pupillary abnormalities, Alachryma, Ptosis, Abnormal lacrimation with food ingestion |
Gastroparesis
Gastroparesis is the delay of gastric emptying without mechanical obstruction. Symptoms that patients might experience include:
- Early satiety
- Nausea
- Vomiting
- Bloating
In diabetic patients, gastroparesis usually occurs after 10 years of the disease and is concurrent with:
- Retinopathy
- Neuropathy
- Nephropathy
Gastric Emptying Process:
- Proximal Stomach: Acts as the reservoir.
- Distal Stomach: Functions as the grinder.
The rate of emptying is influenced by:
- Particle size
- Fat and caloric content
- Physical nature of the contents
Non-nutrient liquids empty rapidly, with the fastest rate occurring if there is a large volume. Solids are retained for churning in the stomach. Once broken down to 2mm diameter particles, solids empty in two phases over 3-4 hours.
Impact on Diabetic Patients:
- Glucose regulating hormones act in different regions of the gut.
- If the vagus nerve is affected, there is a reduction in motor coordination and the number of cells.
- Diabetic patients with gastroparesis are at risk for aspiration.
Anaesthesia Implications of Autonomic Neuropathy
Preop
- Orthostatic hypotension ± supine hypertension
- Gastroparesis and aspiration risk
- Blood volume status
- Slight anemia due to ↓ erythropoiesis
- Consider holding oral vasopressors to prevent drug interactions intra-op
Intra-op
- GA vs Regional: depends on procedure
- Adequate monitoring, constant vigilance
- Hypo- / hyperthermia risks due to poor thermal regulation
- RSI: Not necessary unless other risks are present
- Positioning may have significant effects on vital signs
- Supine hypertension: Nitroglycerine, prone positioning, or reverse Trendelenberg can be used
- Sudden blood volume changes may precipitate untoward BP response
- Avoid pneumoperitoneum or use with extreme caution
- Vasopressors and inotropes can have resistance or undue sensitivity
- Abnormal electrolytes affect responses to medications
Post Op
- Anticipate volume changes
- Observe with a higher level of care
- Orthostatic hypotension: good blood volume and assistance with first ambulation
- Abnormal electrolytes affect responses to medications
- Thermal regulation may be an issue
- Ileus can be worsened by opiate use
- Restart home dysautonomia medications before discharge
Autonomic Dysreflexia
Overview
- Autonomic dysreflexia (ADR) is the most critical and relevant complication of chronic spinal cord injury (CSCI) for the anaesthetist. It is a clinical emergency characterized by a massive disordered autonomic response to certain stimuli below the level of the lesion, such as bladder and bowel distension.
- The incidence of ADR is between 50% and 70% in patients with lesions above T6. Incidence increases with higher level lesions and complete lesions. ADR can occur with lesions as low as T10, though symptoms are less severe. ADR is most common in the chronic stage of SCI (a year after injury), but early episodes can occur within weeks of injury. Approximately 10% of patients with lesions above T6 experience ADR within the first year of injury.
Factors Influencing ADR Development
- Level of Spinal Injury: More common above T6
- Duration of Injury
- Completeness of Injury: Complete lesions have a higher incidence
Pathogenesis and Clinical Findings
Noxious Stimuli
- Examples: Bladder/bowel distension
Pathogenesis
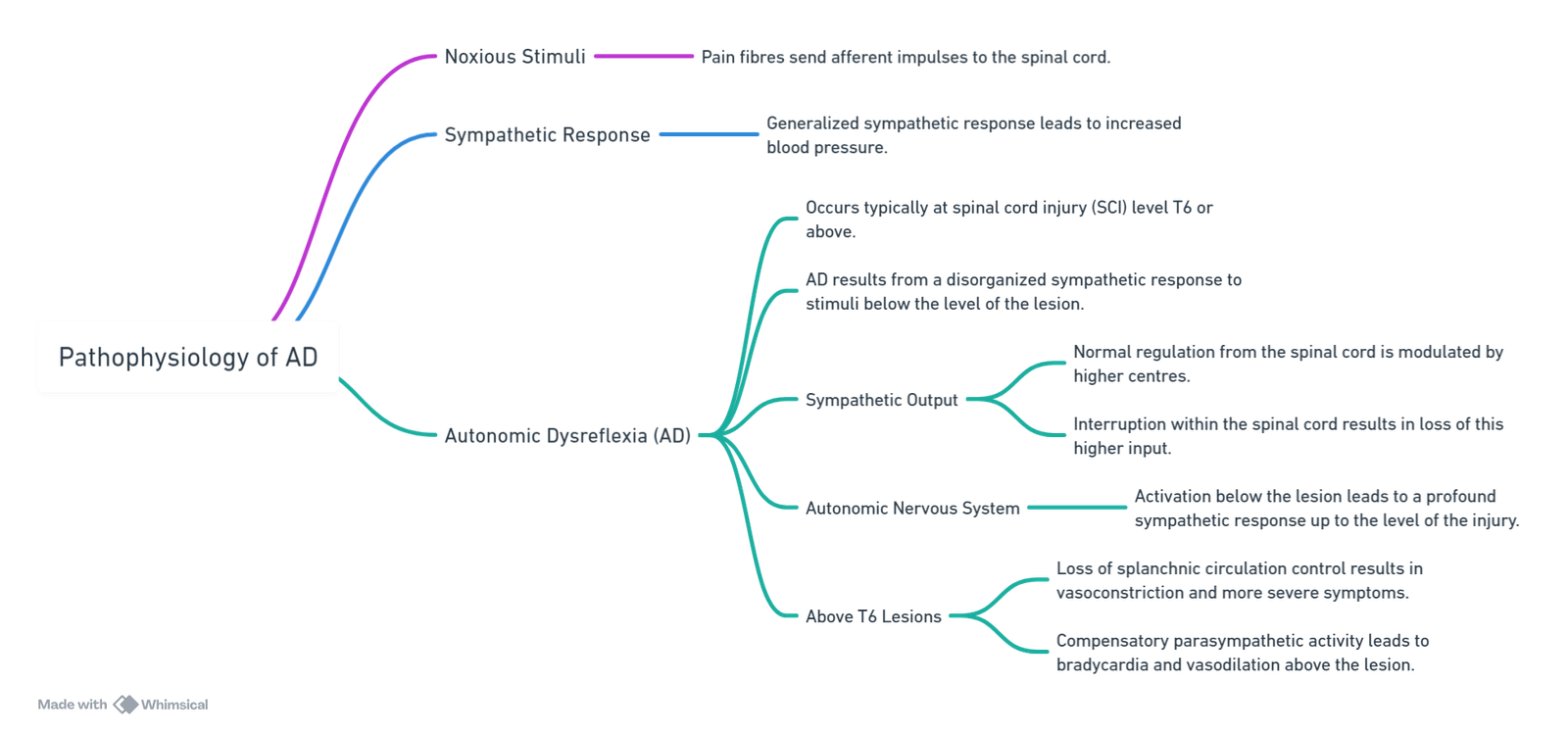
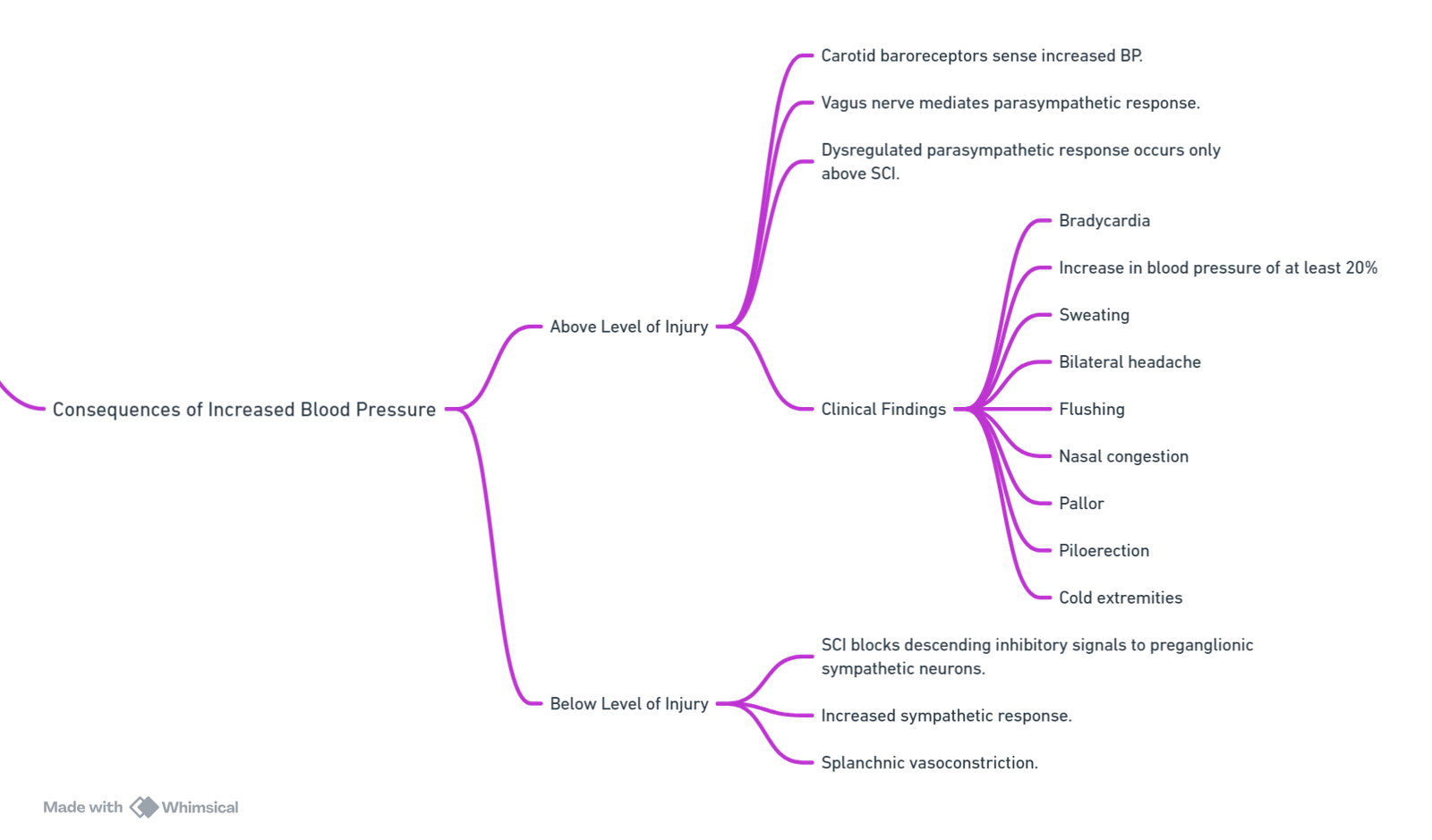
Increased Blood Pressure
- Unregulated Sympathetic Tone: Leads to sustained increasing blood pressure.
Consequences of Increased Blood Pressure
Triggers
Stimuli arise from caudal roots below the level of the lesion:
- Bladder distension (~80% of cases)
- Bowel distension
- Acute abdominal pathology
- Urinary tract infections
- Skeletal fractures
- Pressure ulcers
- Activation of pain fibers
- Sexual activity
- Uterine contractions
Severe Complications
- Raised intracranial pressure
- Seizures
- Intracranial haemorrhage
- Myocardial ischaemia
- Arrhythmias
- Pulmonary oedema
Note
- AD typically occurs with lesions at or above T6 level due to the loss of sympathetic control of splanchnic circulation, leading to a critical mass of blood vessels required to cause elevated blood pressure.
Links
References:
- Allen KJ, Leslie SW. Autonomic Dysreflexia. [Updated 2023 May 30]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2024 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482434/
- Petsas, A. and Drake, J. (2015). Perioperative management for patients with a chronic spinal cord injury. BJA Education, 15(3), 123-130. https://doi.org/10.1093/bjaceaccp/mku024
- The Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
Summaries:
Autonomic dysreflexia
Autonomic nervous system
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “b13aab2b-9e8e-46a5-bfd2-dba3f6c1969a”



