{}
Summary
Clinical Governance
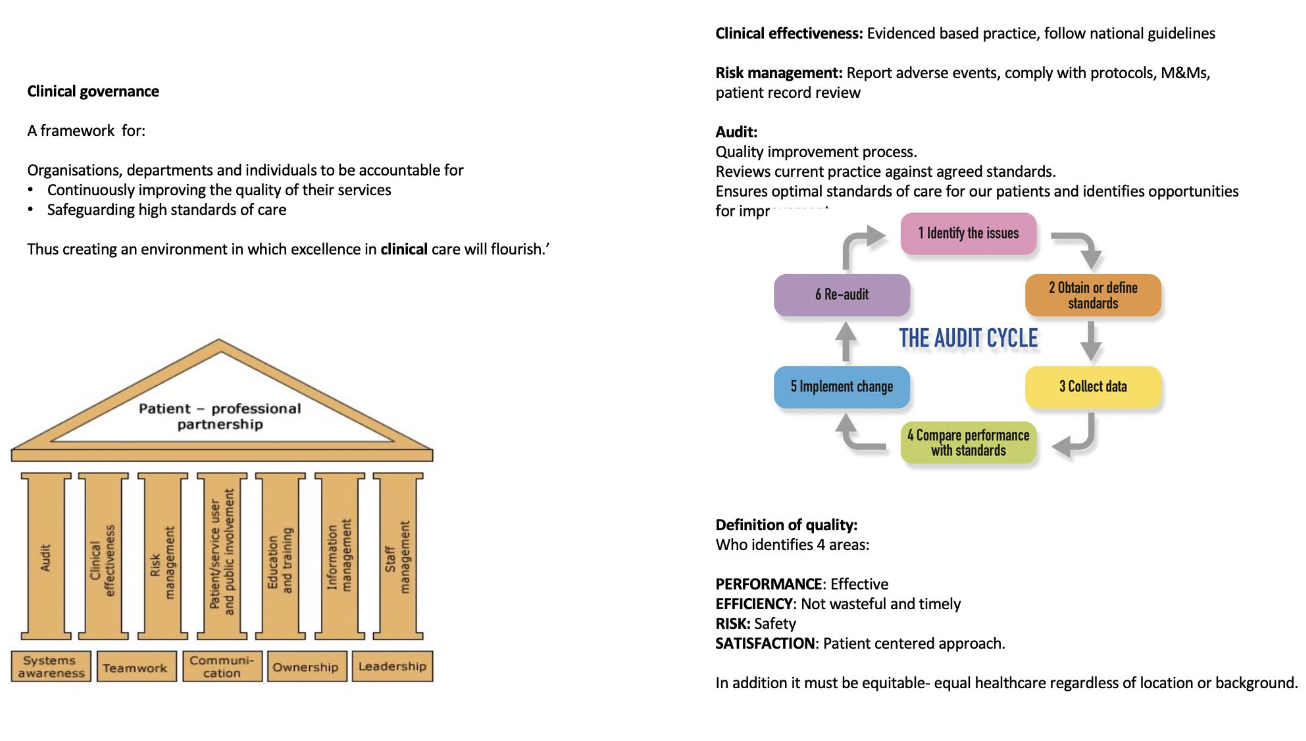
- Clinical governance is the integrated system by which healthcare organisations and individual clinicians continuously improve the quality of care, safeguard high standards and deliver the best possible outcomes. In anaesthesia it links day-to-day theatre practice with organisation-wide safety, quality-improvement (QI) and accountability mechanisms.
- Think of clinical governance as a house that keeps patients safe.
Overview
| Level of detail | Mnemonic / model |
|---|---|
| Core values | 4 Pillars (CCPP) 1. Clinical Effectiveness 2. Continuing CPD 3. Patient safety 4. Patient focus |
| Departmental checklist | 7 Pillars (“temple” graphic) The 4 pillars plus 5. Organisation & leadership 6. Communication & involvement 7. Service quality |
| Operational workstreams | 6 Domains (re-group for day-to-day delivery) What you actually do every week 1. Patient safety & risk management 2. Clinical effectiveness & research 3. QI & audit 4. Education & CPD 5. Information governance & digital health 6. Patient & public involvement |
| Bedside tools | Key safety tools (WHO list, NatSSIPs2, PSIRF, NAPs, etc.) Practical checklists, algorithms, reporting systems that put the domains into action |
Current Strategic Frameworks
| Level | 2025 framework most relevant to anaesthetists | Practical implications |
|---|---|---|
| Global | WHO Global Patient Safety Action Plan 2021-30 | ‘Zero avoidable harm’ goal; systems thinking; supports WHO Surgical Safety Checklist. |
| United Kingdom | Patient Safety Incident Response Framework (PSIRF) 2022 → replaces Serious Incident Framework. | |
| National Safety Standards for Invasive Procedures (NatSSIPs 2) 2023. | ||
| Guidelines for the Provision of Anaesthetic Services (GPAS) 2024 and ACSA accreditation. | ||
| Getting It Right First Time (GIRFT) reviews. | Moves away from blame culture to learning responses; strengthened team briefs, debriefs and human-factors checkpoints; GPAS/ACSA now benchmark departments and may appear in exam vignettes. | |
| South Africa | National Guideline for Patient Safety-Incident Reporting & Learning Version 2 (2022). | |
| National Core Standards (Domain 2: Patient safety, clinical governance & care). | ||
| SASA Anaesthesia Practice Guidelines 2022 & Sedation Guidelines 2020-25. | Mandatory incident reporting with “just-culture” algorithm; OHSC inspections use the 7-domain Core Standards; SASA guidelines define minimal monitoring, staffing and consent for all sedation/anaesthetic services. |
Clinical-governance Roles & Responsibilities during a Full-day Theatre List
| Operational domain | Registered scrub / theatre nurse | Anaesthetic registrar | Clinical head anaesthesiologist (off-site) |
|---|---|---|---|
| 1 Patient Safety & Risk Management | • Run the NatSSIPs 2/ WHO “Sign In–Time Out–Sign Out” checks and stop the list if gaps found. • Log any equipment failure or sharps injury on Datix/eQuate before leaving theatre. |
• Lead the anaesthetic‐specific Time Out (airway grade, aspiration risk). • File Datix when unexpected desaturation / drug error occurs and disclose to patient under duty-of-candour policy. |
• Review all incident reports daily and allocate investigators. • Monitor monthly Never-Event dashboard and commission drills to close gaps. |
| 2 Clinical Effectiveness & Research | • Follow sterile-scrub and count protocols exactly as per SASA guidelines. • Collect wound-infection data for the hospital’s SSI registry. |
• Apply latest national standards/ evidence based protocols • Recruit eligible patients into ongoing RCTs (e.g. airway device trial). |
• Update departmental SOPs when national guidelines change. • Sponsor and sign off ethics applications for trainee research. |
| 3 Quality Improvement & Audit | • Record tray-count timing on the theatre whiteboard for “turn-around time” QI project. • Join PDSA meetings to streamline instrument availability. |
• Audit postoperative PONV scores against anti-emetic bundle; plot run-charts and present at M&M. • Use SPC charts to monitor extubation-in-theatre rate. |
• Allocate QI leads and resources; approve new projects in line with RCoA QI Compendium. • Review GIRFT metrics and feed targets back to each list lead. |
| 4 Education & CPD | • Mentor junior scrub nurses on correct prosthesis handling. • Attend quarterly simulation |
• Run post-list debrief focusing on human factors. • Log cases and reflection to meet HPCSA ≥ 60 CEU / 24 mo (& ≥ 10 Ethics). |
• Schedule weekly multidisciplinary teaching and simulation days. • Monitor CPD compliance across the department. |
| 5 Information Governance & Digital Health | • Enter swab / instrument counts into secure EMR and verify consent • Protect printed labels and destroy them per policy. |
• Complete the anaesthetic chart in real time • Check that patient data transfer meets intuition standards |
• Oversee roll-out of the theatre utilisation dashboard and data-quality audits. • Ensure cybersecurity training and policies are up-to-date. |
| 6 Patient & Public Involvement | • Explain positioning plans to the awake patient and invite questions. • Hand the patient a PREMs feedback card in recovery. |
• Conduct shared-decision discussion on regional vs GA options, documenting PROMs baseline. • Address any immediate family queries post-op. |
• Review quarterly PROMs/PREMs reports and initiate service changes. • Chair complaint-review meetings in line with SA National Guideline (2021). |
PROM Vs PREM–quick Definitions
| Term | Full name | What it captures | Typical use-case in peri-operative care |
|---|---|---|---|
| PROM | Patient-Reported Outcome Measure | The patient’s own rating of their health status, function or symptoms after an intervention | • Tracking recovery after joint-replacement (pain, mobility) • Auditing effectiveness of regional-anaesthesia protocols • Research endpoints in clinical trials |
| PREM | Patient-Reported Experience Measure | The patient’s experience of the care process itself–communication, dignity, waiting times, etc. | • Theatre-list “friends-and-family” feedback • Identifying bottlenecks in admission or discharge processes • Benchmarking service quality between hospitals |
In a Sentence
- PROMs tell you “Did the surgery/anaesthetic improve my health?”
- PREMs tell you “How did I feel about the way the care was delivered?”
What Are “GIRFT metrics”?
- GIRFT = Getting It Right First Time, an NHS-England improvement programme that deep-dives every specialty, benchmarks its hospitals against national data, then sets measurable targets to cut unwarranted variation and waste
- For peri-operative care, the 2021 GIRFT Anaesthesia & Peri-operative Medicine report and the ongoing Theatre Productivity Programme distilled a core dashboard of indicators that every theatre service is now asked to track and share.
| Domain | Sample GIRFT metric | Why it matters / typical benchmark |
|---|---|---|
| Productivity / Efficiency | • Theatre utilisation (paid session time spent operating) • Start-time punctuality (% lists knife-to-skin by < 09:10) • Turn-around time (wheels-out to wheels-in, mins) |
Targets: ≥ 85 % utilisation; ≥ 90 % on-time starts; < 20 min turns. Directly linked to backlog clearance and staff overtime. |
| Quality & Outcomes | • 30-day unplanned ICU admission rate after elective surgery • Return-to-theatre rate within 48 h • Day-case rate for high-volume low-complexity (HVLC) procedures (e.g., lap chole ≥ 85 %) |
Early detection of safety problems; HVLC day-surgery expansion is a key GIRFT pledge. |
| Safety | • “Never Event” dashboard (wrong site block, retained swab) • Compliance with NatSSIPs 2 sign-in / time-out / sign-out (%) |
Flags system gaps; aim is zero Never Events and ≥ 95 % checklist completion. |
| Patient Experience | • PROM collection rate (e.g., QoR-15 pre-op + day-3) • PREM Friends-&-Family Test response and “would recommend” % |
Ensures patient-centred outcomes drive QI cycles. |
| Workforce | • Consultant presence for high-risk (ASA ≥ III) cases (%) • Out-of-hours caseload (% surgery 20:00-08:00 that could be scheduled in-hours) |
Correlates with avoidable harm and burnout. |
| Finance / Litigation | • Anaesthetic-related claims cost per 1 000 cases • Drug-wastage spend per list |
GIRFT’s orthopaedic review cut £63 m/yr in claims; anaesthesia aims for similar. |
| Sustainability | • Volatile-agent CO₂e per case (kg) • Single-use plastic items per GA |
Supports the NHS Net-Zero plan; GIRFT highlights desflurane phase-out. |
Key Safety Tools Every Theatre Must Use
| Tool | Core components | 2025 update |
|---|---|---|
| WHO Surgical Safety Checklist | Sign-in, time-out, sign-out | Remains mandatory; integrate NatSSIPs2 ‘Team Pause’ & ‘STAR’ briefing. |
| NatSSIPs2 standards | 5 organisational & 5 procedural standards | Focus on people, not paperwork; applies to all invasive procedures including blocks & endoscopy. |
| PSIRF response protocol | Triage → learning response → action → share | Requires proactive “patient safety partner” engagement. |
| National Audit Projects (NAP 7) | Data-driven learning from peri-operative cardiac arrest | Embed NAP7 recommendations on early CPR, closed-loop communication & post-ROSC neuroprotection. |
Quality-improvement Cycle
- Identify a measurable problem (e.g. >10 % late theatre starts).
- Set standard (GPAS/ACSA or evidence-based benchmark).
- Collect data (minimum two weeks baseline).
- Analyse & plan change using human-factors principles.
- Implement small-scale PDSA test; re-measure.
- Sustain & spread; publish on departmental QI board, feed into ACSA evidence.
Incident Classification
| Severity | Definition | Immediate actions |
|---|---|---|
| SAC 1 (catastrophic) | Death or permanent severe harm | Notify senior, secure records, communicate with family, initiate PSIRF investigation within 72 h. |
| SAC 2 (major) | Temporary harm needing intervention/unplanned ICU | Complete local investigation; M&M within 30 days. |
| Near-miss | Reached patient? No | Log, share learning at safety huddle. |
- Use the SA National Guideline colour-coded form; adopt just-culture questions for staff support.
South-African Hospital Categories (National Health Act regs)
- District (Secondary)–≤ 300 beds; GP-led, level 1 surgery/obstetrics; transfers to regional.
- Regional (Secondary/Level 2)–200–800 beds; specialist services (medicine, paediatrics, O&G, general surgery, orthopaedics), short-term ventilation.
- Tertiary (Level 3)–400–800 beds; subspecialties, intensivist-led ICU; receives inter-provincial referrals.
- Central (Quaternary)–up to 1 200 beds; national referral, transplant, ECMO, major trauma.
- Specialised–≤ 600 beds; single-stream services (psychiatry, TB, rehab).
Links
Past Exam Questions
Clinical Governance in the Operating Theatre
a) Define, or explain briefly, your understanding of the term “clinical governance.” (4)
b) Using your understanding, give at least two (2) examples of the different clinical governance roles and responsibilities that each of the following categories of staff have when providing care for a full-day operating list. (6)
i) Registered scrub/theatre nurse responsible for the list.
ii) Anaesthetic registrar responsible for anaesthesia care.
iii) Clinical head anaesthesiologist for the department who is not in theatre that day.
References:
- Clinical Governance RT Erasmus Division of Chemical Pathology Department of Clinical Laboratory Sciences University of Cape Town, Cape Town South Africa
- Centre for Perioperative Care. National Safety Standards for Invasive Procedures (NatSSIPs 2). 2023. cpoc.org.uk
- NHS England. Patient Safety Incident Response Framework. 2022. england.nhs.uk
- Royal College of Anaesthetists. NAP7: Perioperative Cardiac Arrest–Main Report. 2023. rcoa.ac.uk
- Royal College of Anaesthetists. Guidelines for the Provision of Anaesthetic Services 2024–Chapter 1 “The Good Department”. 2024. rcoa.ac.uk
- Royal College of Anaesthetists. Raising the Standards: Quality Improvement Compendium (5th ed.). 2024. rcoa.ac.uk
- National Department of Health (SA). National Guideline for Patient Safety Incident Reporting & Learning–Version 2. 2022. knowledgehub.health.gov.za
- Office of Health Standards Compliance. National Core Standards for Health Establishments. 2018. knowledgehub.health.gov.za
- South African Society of Anaesthesiologists. Guidelines for Safe Procedural Sedation & Analgesia 2020-25. 2020. sajaa.co.za
- World Health Organization. Global Patient Safety Action Plan 2021-2030. 2021. who.int
- Macfarlane, A. (2019). What is clinical governance?. BJA Education, 19(6), 174-175. https://doi.org/10.1016/j.bjae.2019.02.003
Summaries:
© 2025 Francois Uys. All Rights Reserved.
id: “749dd452-7ef6-454b-bdcc-8b47c796f070”



