- Summary
- Informed Consent & Shared Decision-Making
- Groote Schuur Hospital (GSH) Consent Protocol
{}
Summary
Informed Consent & Shared Decision-Making
Core Concepts
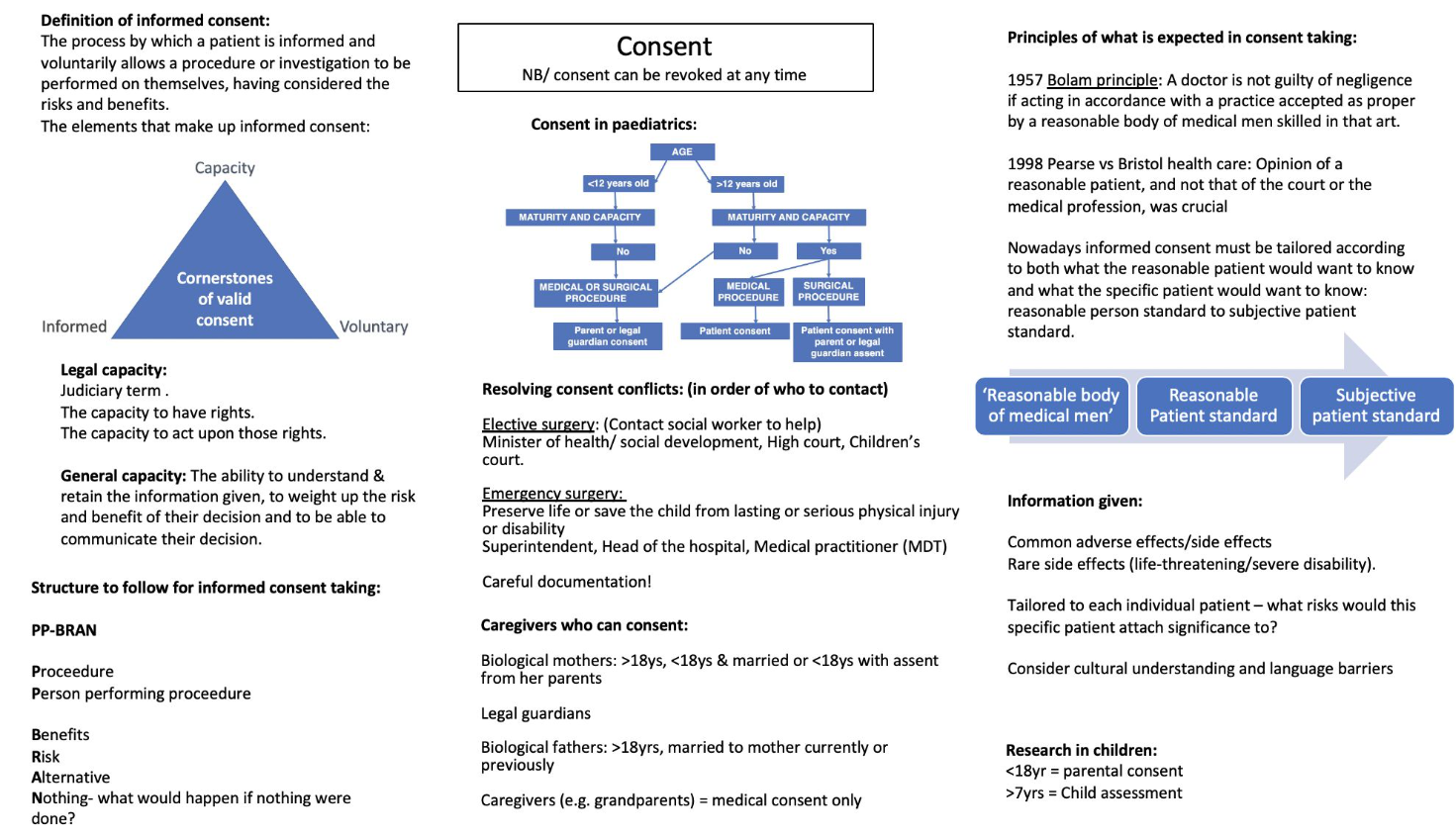
| Term | Concise definition | Practical point for anaesthetists |
|---|---|---|
| Consent | Ongoing, voluntary authorisation for a specific intervention. | Re-confirm immediately before induction |
| Informed | Based on adequate disclosure of material facts in understandable language. | Use teach-back to confirm comprehension. |
| Capacity | Ability to understand, weigh, retain and communicate a choice for the decision at hand. | Pregabalin, hypoxia, sepsis may transiently impair capacity. |
| Shared Decision-Making (SDM) | Collaborative process integrating medical evidence with the patient’s values and preferences to reach a mutually agreed plan. | Improves adherence and reduces litigation. |
Elements of a Valid Consent (FIVE-IC mnemonic)
- Free from coercion (voluntariness)
- Information–PPC iBRANE: person performing procedure, procedure purpose, cost, individualize benefits, risks, alternatives, nothing is done. Expectations after procedure
- Veracity–honest answers, no misleading omissions, shared decision making (PAIR model)
- Evidence of capacity (age + mental competence): 4 step capacity testing
- Indication in writing (documentation)–signature or digital record where required
- Continuous: Ongoing Review–consent is a process, not a form; update if clinical situation changes.
- Confirmation–re-check willingness on day of surgery or after significant delay.
- Absent any element → consent defective; treat only under statutory exceptions.
Information (PPC IBRANE)
- Person performing procedure
- Procedure purpose
- Cost
- Individualize
- Benefits
- Risks (common >1% and serious)
- Alternatives
- Nothing done
- Expectations after procedure
Shared Decision-Making–4-Step “PAIR” Model
- Prepare–quiet space, decide which decisions are preference-sensitive.
- Assess patient’s understanding, values, desired role.
- Inform–balanced evidence, decision aids, plain language.
- Reach Resolution–confirm preference, agree plan, schedule review.
- Facilitators: clinician motivation, decision aids, culture of partnership.
- Barriers: time pressure, paternalistic attitudes, health literacy gaps.
Capacity & Age Rules
Capacity: The 4-step Test for Decision-making Capacity
- Understand–Can the person comprehend the nature, purpose, and consequences of the decision (including the likely risks and benefits of the options)?
- Retain–Can they hold that information in memory long enough to make the choice?
- Use / Weigh–Are they able to reason with the information, balancing pros and cons to reach a coherent, voluntary decision?
- Communicate–Can they convey their choice by any reliable means (speech, writing, sign, assistive device, eye-blinks, etc.)?
| Group | Who consents? | Notes |
|---|---|---|
| Adults ≥ 18 yr | Patient if capacitated. | Presumed competent; burden of proof on clinician to show incapacity. |
| Adults lacking capacity | Surrogate hierarchy → spouse/partner → parent → grandparent → adult child → sibling → best-interests decision. | Document 4-step capacity test and surrogate discussion. |
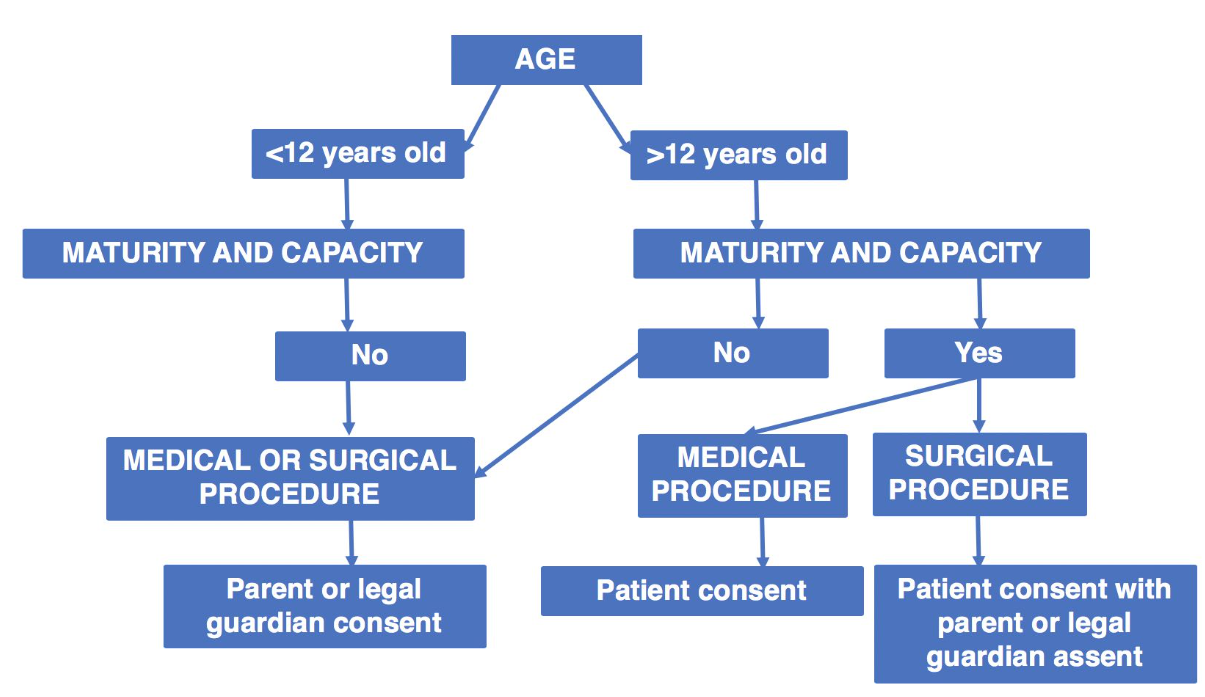
| Children ≥ 12 yr & mature | Child for medical; child + parent for surgery. | Assess maturity; record in notes. |
| Children < 12 yr or immature | Parent/guardian; Minister of Social Development if absent. | Emergency: practitioner may proceed in best interests under NHA. |
| Child-parents | May consent for their own infant if mature; their guardian co-signs for surgery (Form 35). |
Children Specifics
| Decision | Independent age threshold |
|---|---|
| Medical treatment | 12 yr + sufficient maturity |
| Surgery | 12 yr + maturity plus parental co-signature (Form 34) |
| HIV test, contraception | 12 yr |
| Male circumcision | 16 yr (unless religious/medical) |
| Research | < 18 yr = parental consent + child assent > 7 yr |
Special Topics
HIV Testing
- Illegal without consent except: occupational exposure of source patient, court order, or anonymous epidemiological surveillance. Pre- & post-test counselling mandatory.
Research Consent
- Requires NHREC-registered REC approval + participant (or surrogate) written consent; children need parental permission + age-appropriate assent.
Caesarean Section or Termination of Pregnancy (TOP)
- No Age Cut-Off: There is no age cut-off for consenting to a Caesarean section or TOP.
High-risk Cases (e.g., Awake Craniotomy, ECMO)
- Provide procedure-specific written information sheet; encourage “cool-off” period; consider audio-recording disclosure with patient consent.
Organ & Tissue Donation (Consent Rules in South Africa)
| Consent route | Statutory basis | Key requirements | Practical theatre implications |
|---|---|---|---|
| Deceased donor–first-person consent | National Health Act 61/2003 §62 (previous Human Tissue Act repealed) | • Competent person (≥ 18 yr) may sign an organ-donor card, complete an advance directive, or give witnessed verbal instructions (≥ 2 witnesses > 14 yr). • Instruction must name intended use or allow “any therapeutic use”. |
Check wallet / Electronic Health Record for Opt-In; record presence of card in notes; notify transplant coordinator. |
| Deceased donor–surrogate consent | NHA §62(3) | In absence of a written directive and no objection recorded, consent may be obtained in order of precedence: spouse → permanent life-partner → adult child → parent → guardian → adult sibling. | Partners outrank all relatives except spouse; unresolved disputes → seek High-Court declaratory order. |
| Director-General consent | NHA §62(4) | If no relative reachable “within reasonable time”, Director-General (DG) of Health may authorise donation. | Theatre/facility must show documented attempts to contact family before DG route. |
| Retrieval time-limits | NHA Reg. R. 180 | Solid organs & vascularised composite grafts within 24 h of death; corneas up to 72 h (provided body cooled). | Ensure rapid referral to transplant team; keep body at 4 °C if retrieval delayed. |
| Living donation | NHA §63–65 | • Written informed consent; donor ≥ 18 yr. • Minors may only donate regenerative tissue (marrow, skin) with parental consent + ministerial approval. • No financial gain except reasonable expenses. |
Independent donor advocate must document voluntariness; report to SAHPRA living-donor registry. |
- Documentation checklist (donation): death certificate (DHA-1663), ICU summary, serology, brain-death certification x 2, consent form, chain of custody form
Legal & Ethical Framework (South Africa)
| Instrument | Key duties |
|---|---|
| National Health Act 61/2003 §6-7 | Unlawful to provide health service without valid consent; sets emergency and public-health exceptions. |
| HPCSA Booklet 9 (2021) | Details ethical requirements: disclosure, capacity assessment, voluntariness, documentation. |
| Children’s Act 38/2005 §129 | Children ≥ 12 yr & mature may consent to medical treatment; surgical consent needs parental co-signature. |
| Mental Health Care Act 17/2002 | Governs consent for psychiatric users; physical treatment still needs usual consent route if capacity intact. |
| Bill of Rights (Constitution §12 & §27) | Guarantees bodily integrity and access to healthcare information. |
National Act (2003) and the National Patients Health Charter (2008)
- Illegal Provision of Health Services: The National Health Act 2003 makes it an offence to provide a health service to a user without the user’s informed consent.
- Exceptions:
- An emergency where delay would result in death or serious harm to the patient.
- When mandated by law or a court order.
- Where failure to treat the patient would result in a serious risk to public health.
- Exceptions:
- Consent by Proxy: If the patient lacks capacity and a proxy or family member is consenting on their behalf, that person must be given all the necessary information to give informed consent.
- Patients Health Charter (2008): States that everyone has the right to be given full and accurate information about:
- The nature of one’s illnesses.
- Diagnostic procedures.
- The proposed treatment.
- The costs involved.
- This information is essential for making decisions that affect any of these elements.
Groote Schuur Hospital (GSH) Consent Protocol
- Designated consent-taker–only the operating consultant/registrar may obtain consent; nurses or interns explicitly barred (HPCSA Bk 9, GSH SOP).
- Timing rule–written consent must be completed before any pre-medication is given.
- Witness rule–any adult ≥ 14 yr (not involved in the case) may sign, but their role is identity verification only.
- Interpreter recording–form must note name & details of any accredited interpreter (HPCSA Interpreter Guideline 2022).
- Procedure list that always needs written consent at GSH–adds intra-operative photography and sterilisation to the usual surgery/GA/RA/blood/ research items.
- Form numbers–elective surgery uses Form I-2 for adults, Form 34 for mature minors, Form 33 via Social Development if competent child’s wish conflicts with parent.
- Emergency workflow–consultant may proceed after phoning MMS; if delay itself is lethal, may proceed without MMS and document rationale.
Special Consent Situ
| Intervention | Key GSH requirements |
|---|---|
| Sterilisation | ≥ 18 yr competent: patient signs. < 18 yr: only for health reasons; needs patient + guardian consent, independent doctor letter, Sterilisation Panel approval. |
| Termination of pregnancy | Woman’s consent sufficient at any age; counsel minor to involve parent but cannot compel. “Minor’s statement” part 1 filed. |
| HIV / HBV / HCV testing | Verbal consent after pre-test counselling; document in notes. Children ≥ 12 yr may self-consent. |
| Needlestick source testing | If patient refuses/unconscious → follow occupational policy; treat HCW empirically or use previously drawn blood (with post-test disclosure). |
| Blood transfusion | Explicit discussion of risks, alternatives (cell-salvage, Jehovah’s Witness options) and benefits; emergency override if delay endangers life. |
| Intra-operative photography | Pre-operative written consent if planned; if unforeseen, obtain post-op verbal consent and delete images if refused. Identifiable images need separate release form. |
| Mental Health-Care user | Unless psychiatrist certifies incapacity, patient consents for non-psychiatric surgery. If incapable, curator/closest family or CEO (on surgeon’s written request) authorises. |
| Organ donation (living & deceased) | Transplant Co-ordinator obtains consent; donation cannot proceed if identity unknown or relatives unavailable. Consent must precede death certification in DCD cases. |
Links
- General Ethics
- Practice management
- Research ethics
- Impaired capacity
- Transplants and organ donation
- Practice guideline
Past Exam Questions
Informed Consent for Research Subjects and Minors
a) What are the 3 requirements for informed consent for research subjects? (3)
b) What factors may change the validity of a minor’s consent or their ability to give consent? (2)
c) What methods, principles, and adjuncts will assist you in obtaining “informed consent” from a minor? (5)
Ethical Considerations in Medical Practice
a) During a laparotomy, the medical and nursing students wish to capture the image of an excised teratoma on their cell phones. Discuss how you would advise them. (3)
b) What steps should be considered to protect patient confidentiality on multimedia educational platforms? (3)
c) You are asked by a surgeon to anaesthetise a patient for an emergency procedure. You believe that the procedure is not in the best interests of the patient. How do you proceed? (4)
References:
- Tierney, Sarah; Perlas, Anahi. Informed consent for regional anesthesia. Current Opinion in Anaesthesiology 31(5):p 614-621, October 2018. | DOI: 10.1097/ACO.0000000000000635
- Strode, A., Slack, C., & Essack, Z. (2010). Child consent in south african law: implications for researchers, service providers and policy-makers. South African Medical Journal, 100(4), 247. https://doi.org/10.7196/samj.3609
- Jackson, G. and Cox, M. (2011). Consent on labour ward. Trends in Anaesthesia and Critical Care, 1(1), 7-12. https://doi.org/10.1016/j.cacc.2010.07.016
- Ivashkov, Y. and Norman, G. A. V. (2009). Informed consent and the ethical management of the older patient. Anesthesiology Clinics, 27(3), 569-580. https://doi.org/10.1016/j.anclin.2009.07.016
- Groote Schuur Hospital. Standard Operating Procedure: Informed Consent v5.2 (April 2024).
- Western Cape Department of Health. Circular H97/2023–Consent for Surgical Procedures in Minors.
- South African National Blood & Organ Donor Foundation. Consent & Retrieval Guidelines 2024.
- Cook TM et al. NAP3: Major Complications of Central Neuraxial Anaesthesia. RCoA 2009.
- Barrington MJ, Kluger R. Ultrasound guidance reduces serious complications of peripheral nerve blocks. Reg Anesth Pain Med 2023;48:155-63.
- Association of Anaesthetists. Guidelines for the Provision of Anaesthesia Services (GPAS): Peri-operative Tissue Donation. 2022.
- RA-UK. Consent for Peripheral Nerve Block (Position Statement) 2020.
- ASRA. Practice Advisory on Neurologic Complications of Regional Anaesthesia 2018.
- Health Professions Council of South Africa. Guidelines on Informed Consent (Booklet 9). 2021.
- Republic of South Africa. National Health Act 61 of 2003, §§6-7.
- Republic of South Africa. Children’s Act 38 of 2005, §129.
- Mouton-du-Plessis v. H, Supreme Court of Appeal (212/13) [2015] ZASCA 19.
- Woolley S. Capacity, consent and adolescents. SAMJ 2022;112:240-4
- Charles C, Gafni A, Whelan T. Shared decision-making in the medical encounter. Soc Sci Med 1997;44:681-92.
Summaries
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “2ed75ec2-7cd0-46dd-884e-c84148ebaefe”



