{}
Contrast-Induced Nephropathy (CIN)
Presentation
- Radiocontrast Induced Renal Failure:
- Usually mild, transient, and nonoliguric.
- Begins within 12-24 hours of contrast administration.
- Recovery typically within 3-5 days.
- Severe Cases:
- Creatinine peaks > 5 mg/dL (440 μmol/L), particularly if baseline plasma creatinine > 4 mg/dL (352 μmol/L).
- May require dialysis.
- Persistent renal failure occurs in patients with advanced underlying disease, especially diabetics.
Diagnosis
- Characteristic Rise in Plasma Creatinine:
- Begins within the first 12-24 hours post-contrast administration.
- Differential Diagnosis:
- Consider ischemic acute tubular necrosis, acute interstitial nephritis, and renal atheroemboli.
- Renal Atheroemboli Indicators:
- Presence of embolic lesions or livedo reticularis.
- Transient eosinophilia and hypocomplementaemia.
- Delayed onset renal failure (days to weeks post-procedure).
- Protracted course with minimal or no recovery of renal function.
Risk Factors
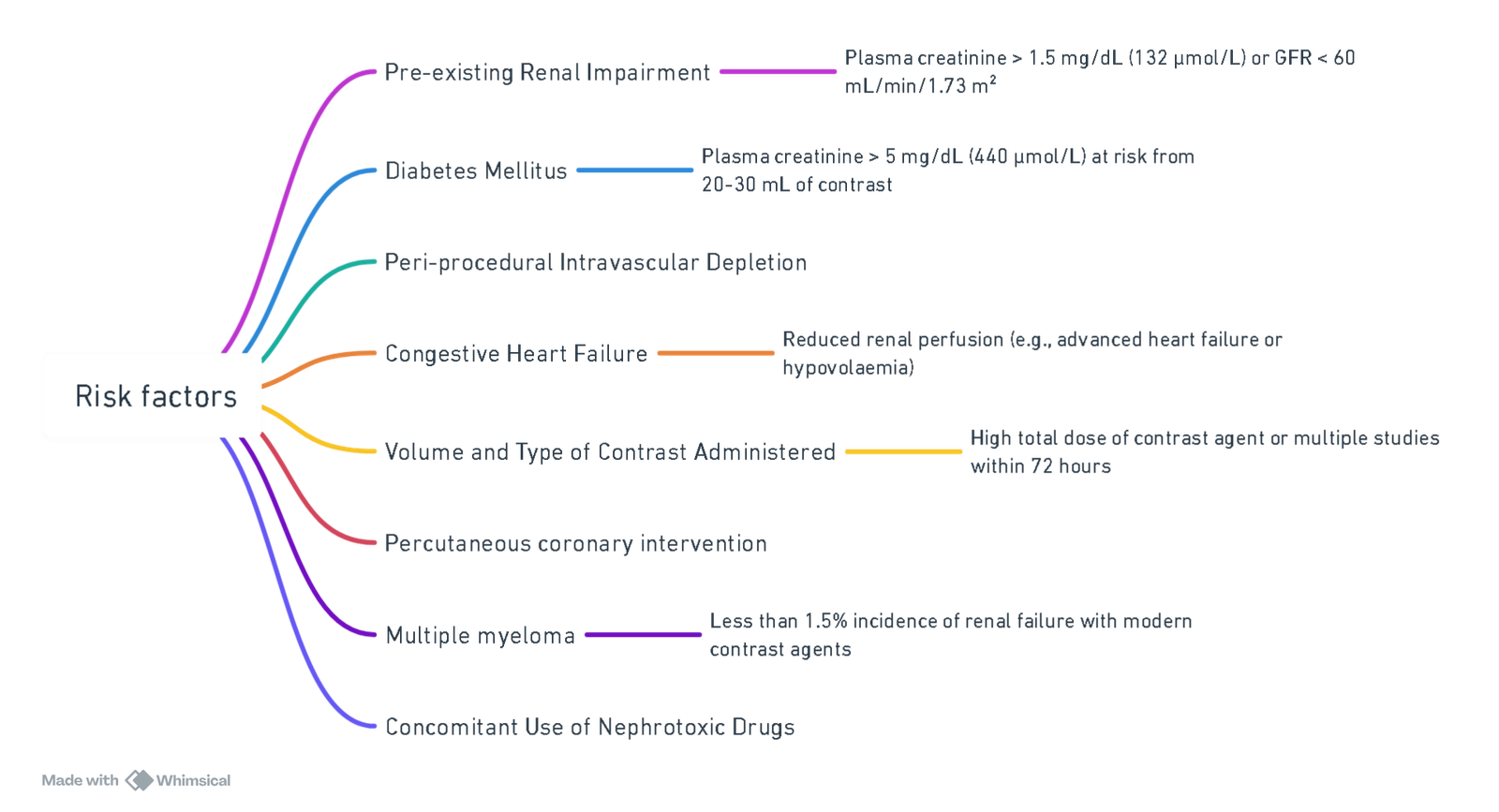
View or edit this diagram in Whimsical.
Prevention of Contrast-Induced Nephropathy
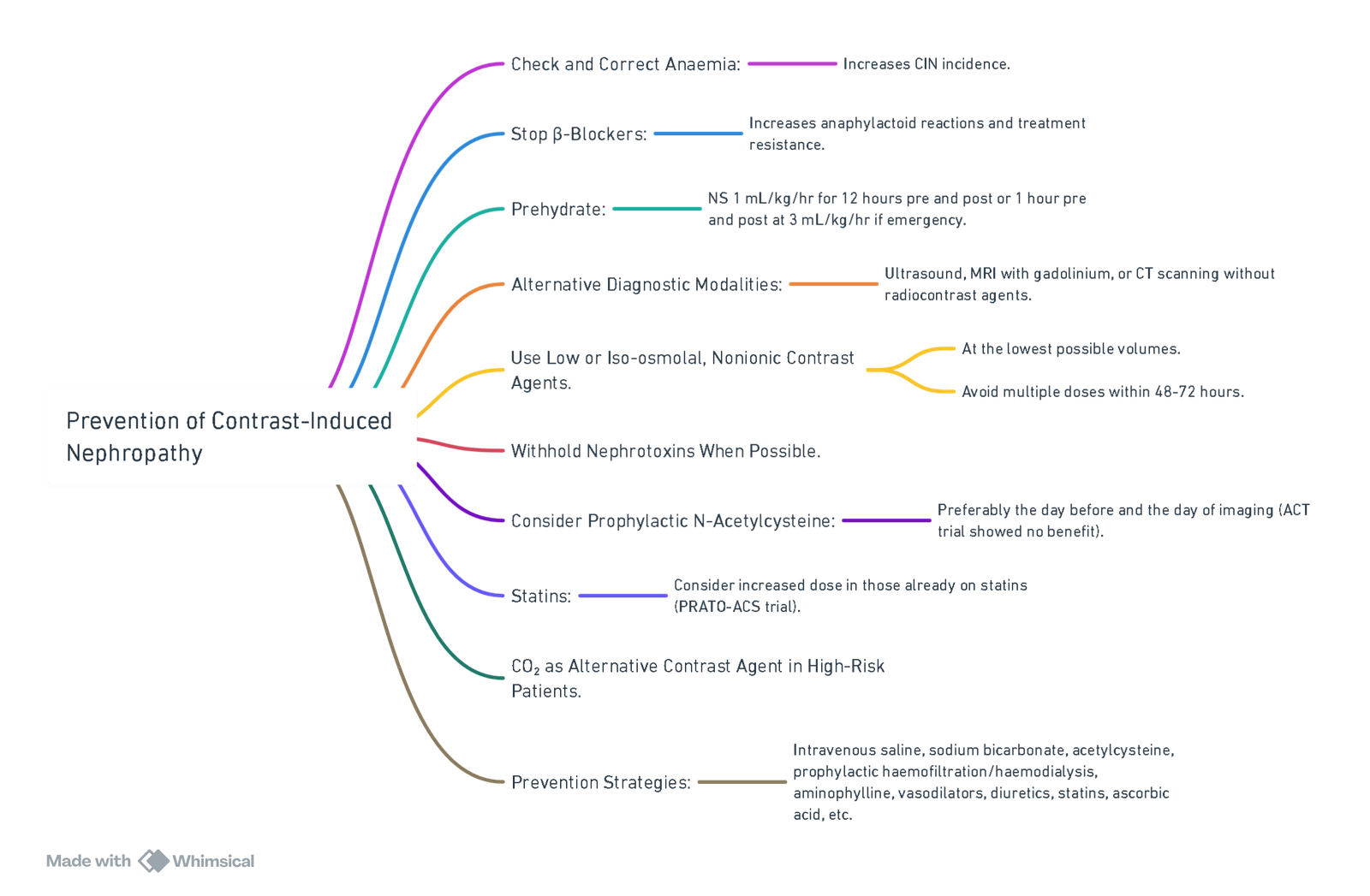
View or edit this diagram in Whimsical.
Management of Contrast-Induced Acute Renal Failure
- General Management:
- No specific treatment for contrast-induced acute renal failure.
- Manage as acute tubular necrosis, focusing on fluid maintenance and electrolyte balance.
Summary of Strategies
- Optimal Prophylaxis:
- Uncertain but includes avoidance of volume depletion and NSAIDs.
- At-Risk Patients (Defined by Rudnick et al):
- Plasma creatinine > 1.5 mg/dL (132 mmol/L) or eGFR < 60 mL/1.73 m², especially in diabetics.
- Recommendations:
- Use non-contrast diagnostic modalities where possible.
- Avoid high osmolal agents (Grade 1A).
- Prefer iso-osmolal agents to low osmolal agents (Grade 2B).
- Use lower doses of contrast and avoid repetitive studies < 48 hours apart.
- Administer isotonic IV fluids before and after contrast administration (Grade 1B).
Fluid Regimen for Prophylaxis
- Isotonic Saline:
- 1 mL/kg/hr, started at least 2 and preferably 6-12 hours prior to the procedure, and continued for 6-12 hours after contrast administration.
- Isotonic Bicarbonate:
- Bolus of 3 mL/kg over 1 hour pre-procedure, continued at 1 mL/kg/hr for 6 hours post-procedure.
- Preparation: Add 150 meq sodium bicarbonate to 850 mL of 5% dextrose in water.
Reduction of Incidence After a Previous Reaction
- Stop β-Blockers.
- Premedicate with Corticosteroids ± Antihistamines.
- Consider Alternative Contrast Mediums:
- CO₂ or CO₂ DSA.
Links
Past Exam Questions
Prevention of Contrast-Induced Nephropathy and Contrast Reactions
A 55-year-old patient with ischaemic heart disease is booked for coronary angiography. He is diabetic and hypertensive.
a) How will you minimise the risk of contrast-induced nephropathy in this patient? (7)
b) This patient has had a previous angiography study and reacted to the contrast medium used, and a repeat angiography has to be performed. How will you reduce the incidence of the reaction? (3)
References:
- Papendorf, D. (2007). Radiocontrast nephropathy: (renal protection). Southern African Journal of Anaesthesia and Analgesia, 13(6), 26–31. https://doi.org/10.1080/22201173.2007.10872509
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “24e4b28b-efb1-46ae-a872-b2ae9a506b90”



