{}
Management of an Intra-operative or Procedure-Related Death–South-African Requirements
Immediate (“Golden Hour”) Actions
| Step | Detail | Purpose |
|---|---|---|
| Regain composure & lead | Pause; allocate a team leader (usually the most senior anaesthetist). | Ensures coordinated response and clear delegation. |
| Secure the scene | Leave all lines, tubes and monitoring attached; stop infusions; note clock time. | Preserves forensic evidence. |
| Confirm death | Two practitioners certify as per DHA-1663 Section C. | Legal prerequisite before further steps. |
| Notify immediately | • Senior anaesthetist & surgeon • Theatre nursing manager • Hospital risk manager / Patient Safety Incident (PSI) officer |
Triggers mandatory reporting workflow. |
| Document contemporaneously | Complete full anaesthetic chart + narrative note without alteration; add print-outs (vitals, ABGs). | Protects integrity of record; meets SASA guidance. |
| Family briefing (first contact) | Joint surgeon-anaesthetist disclosure in quiet room; empathic, factual; offer spiritual support. | Ethical duty of candour and early transparency. |
| Contact indemnity insurer | Phone your Medical Protection Society helpline before detailed written statements. | Medico-legal protection. |
Mandatory Documentation & Forms (South Africa)
| Form | Who completes | When / Where filed | Notes |
|---|---|---|---|
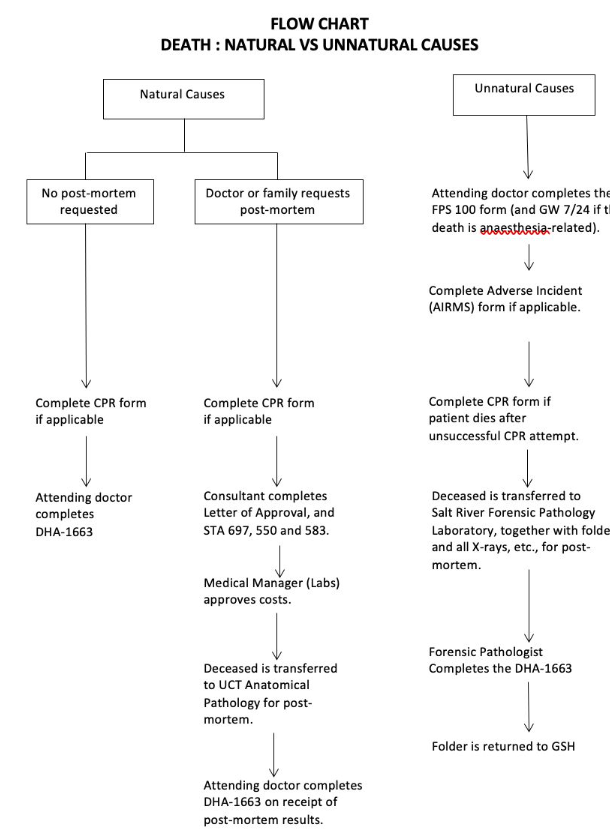
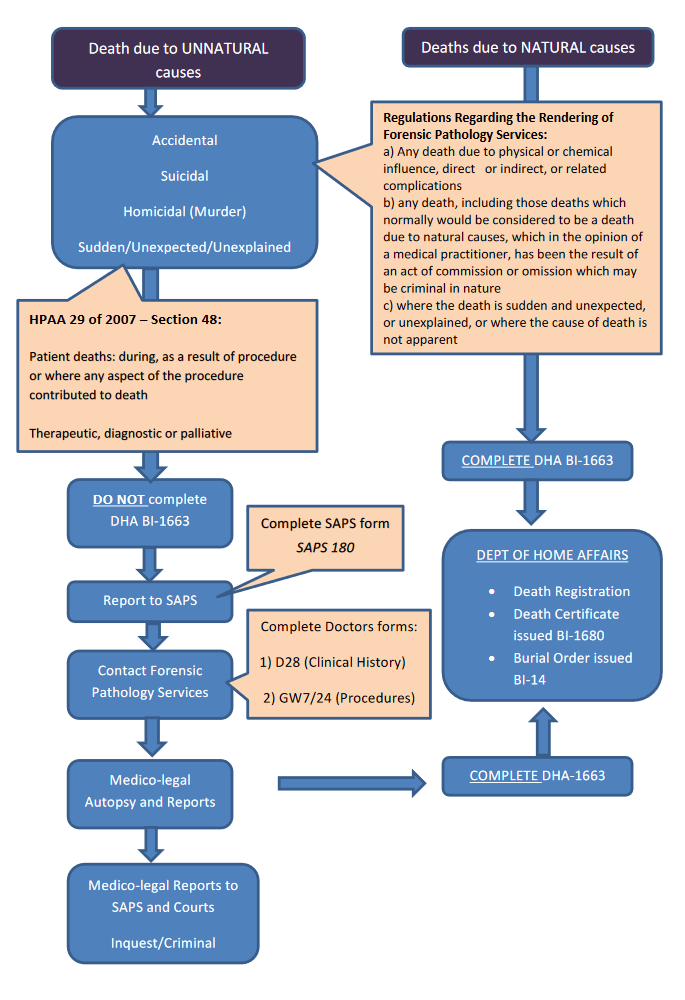
| GW 7/24–Report of a Death Associated with Anaesthesia / Procedure | Attending anaesthetist (Part A); surgeon (Part B); Head of Dept (Part C). | Within 24 h; copies to Provincial Forensic Pathology Services (FPS) & Department of Health incident office. | Statutory under Health Professions Amendment Act 29/2007 §48. |
| DHA-1663–Notification/Certificate of Death | Certifying doctor. | Originals to Department of Home Affairs via undertaker; duplicate for hospital file. | |
| FPS 100–Body referral | Theatre nurse / mortuary porter. | Travels with body to forensic mortuary. | |
| Adverse Event / PSI form | Unit manager or PSI officer. | Upload to National Patient Safety Incident Reporting & Learning System within 48 h. | |
| Maternal Death Notification (MDNF) | Obstetric anaesthetist / obstetrician. | Within 24 h to District Clinical Specialist Team. | |
| Clinical Record Print-outs | Anaesthetic team. | Filed with main notes; duplicate set for FPS. | Never remove originals from hospital. |
Equipment & Drug Audit
- Seal airway devices, syringes and infusion sets in labelled bags.
- Quarantine anaesthetic machine/ventilator for biomedical inspection.
- Record batch numbers of all drugs and fluids used; retain empty vials.
- Engage biomedical engineer + pharmacy manager; create written report for M&M.
Team & Department Follow-up
| Timing | Action | Rationale |
|---|---|---|
| Within 2 h | Hot debrief in empty theatre; immediate emotions & factual recap. | Psychological first-aid; captures fresh memories. |
| 24–72 h | Cold debrief / M&M chaired by HoD; structured (SBAR or ALARM). | System learning; identify latent factors. |
| ≤ 1 week | Arrange formal counselling / Employee Assistance Programme for affected staff. | Prevents burnout/PTSD. |
| Ongoing | Assess competency gaps; schedule simulation or supervised lists before clinician returns to solo work if needed. | Restores confidence and patient safety. |
Communication Outside the Team
- Media enquiries: handled only by hospital Communications Officer; clinicians should provide no comment and refer.
- Legal requests: route via hospital medico-legal office/insurer.
- Religious considerations: FPS endeavours to perform autopsy within 24 h; liaise with family faith leader.
Key Definitions
| Term | Legal Source | Meaning |
|---|---|---|
| Procedure-related death | Health Professions Act 56/1974, amended §48 | Death occurring during or as a result of any therapeutic, diagnostic or palliative procedure, or where any aspect of such procedure was a contributory cause; considered unnatural irrespective of time interval. |
| Unnatural death | Inquest Act 145/1992 | Four categories: application of force; act of commission/omission; procedure-related; sudden unexplained. |
| Adverse event (Patient Safety Incident) | DoH PSI Guideline v2/2022 | Any unintended or unexpected incident which could have or did lead to harm. |
Religious & Cultural Sensitivities
- 24-h forensic pathology service should accommodate faiths requiring early burial (Islam, Judaism).
- Offer viewing of the body before transfer if culturally appropriate.
- Document all family requests and steps taken to honour them.
Checklist for On-Call Anaesthetist
- ☐ Stop, breathe, call for senior help.
- ☐ Confirm death; note time.
- ☐ Preserve lines/tubes; seal evidence bags.
- ☐ Complete anaesthetic record + narrative.
- ☐ Phone HoD, risk manager, insurer.
- ☐ GW 7/24 + DHA-1663 + FPS 100 started.
- ☐ Joint family meeting arranged.
- ☐ Equipment quarantined.
- ☐ Hot debrief scheduled.
Groote Schuur Hospital Guideline
Debriefing Mnemonic
IF SPOTS–Structured Debriefing Memory Aid
| Step | Mnemonic | Key Points to Cover | Typical Prompts / Notes |
|---|---|---|---|
| 1 | I — Introduction | • Emphasise confidentiality and voluntary participation • Clarify the session is time-limited and a learning opportunity |
“This debriefing is confidential and voluntary. It will take about ___ minutes and is meant to help us learn from the event.” |
| 2 | F — Facts-gathering | • Obtain an objective medical summary of the incident | “Let’s briefly review what happened, step-by-step, using the chart and monitors.” |
| 3 | S — Subjective | • Explore thoughts, reactions, and feelings of team members | “How did the situation feel from your perspective?” |
| 4 | P — Positives | • Identify what went well • Reinforce effective behaviours |
“What do you think went well?” “I’d like to highlight that you did ___ particularly well.” |
| 5 | O — Optimisation | • Elicit learning opportunities • Discuss how to improve hospital protocols or systems |
“What could we change next time to make this process safer or smoother?” |
| 6 | T — Teaching | • Provide concise, targeted teaching points relevant to the event | “Based on today’s case, remember that in massive haemorrhage …” |
| 7 | S — Support | • Offer emotional or logistical support as needed (peer, psychological, operational) | “Does anyone need additional support or follow-up after this incident?” |
Links
Past Exam Questions
Intraoperative Cardiac Arrest and Procedure-Related Death
A 58-year-old woman is booked for an elective cholecystectomy and suffers a cardiac arrest during the procedure. Following 30 minutes of appropriate resuscitation, the patient is declared dead on the operating table.
a) What is a procedure-related death? (3)
b) List the actions that should be taken following this patient’s death. (7)
References:
- White SM., 2003. Death on the table. Anaesthesia, (58) p.515-519
- Aitkenhead AR., 1997. Anaesthetic disasters: handling the aftermath. Anaesthesia, (52) p.477-482
- Bacon AK., 1989. Death on the Table. Anaesthesia, (44) p.245-248
- South African Society of Anaesthesiologists. Practice Guidelines 2022–Adverse Event Reporting. sasaweb.com
- Department of Health. National Guideline for Patient Safety Incident Reporting and Learning–Version 2 (2022). knowledgehub.health.gov.za
- Health Professions Amendment Act 29 of 2007–Section 48. gov.za
- Department of Home Affairs. Form DHA-1663: Notification of Death / Still-Birth (2009). suedafrika.org
- SASA. Adverse Events Toolbox (2016). sasaweb.com
- Association of Anaesthetists of Great Britain and Ireland (AAGBI), 2005. Catastrophes in Anaesthetic Practice–Dealing with the Aftermath. London: Association of Anaesthetists of Great Britain and Ireland. http://www.aagbi.org/publications/guidelines/docs/catastrophes05.pdf
- Australian Society of Anaesthetists; Catastrophes in Anaesthetic Practice.http://www.asa.org.au/static/2/V/e9578706ef595748cfb66285fe07d0 2a.pdf
- Health Professions Amendment Act 29 of 2007, Section 48
- Death on the table Sandhya Jithoo. 2012
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “696db81c-ac7c-4f04-a13d-93da3e23c133”



