{}
Jehovah’s Witness Patients–Consent, Legal Duties & Blood-Sparing Anaesthetic Care
Documentation Checklist
- Verify official Watchtower “Patient Blood Management” card / hospital form.
- List in notes exactly which products / procedures the patient accepts or declines
- Have patient sign “Blood Refusal Statement” + witness (≥ 14 yr) + interpreter details.
- Attach to anaesthetic chart and hand-off sheet; flag in EMR and on theatre whiteboard.
- For minors: file Children’s Act Form 34 (surgery) + clinician affidavit if court order sought.
Acceptability Matrix (confirm individually)
| Category | Usually declined | Individual decision | Usually accepted |
|---|---|---|---|
| Major components | RBCs, plasma, platelets, granulocytes | — | — |
| Fractions | — | Albumin, immunoglobulins, clotting factors, haemoglobin solutions, cryoprecipitate | — |
| Procedures | — | Cell salvage (closed circuit), acute normo-/hypervolaemic haemodilution, cardiopulmonary bypass, ECMO, plasmapheresis, epidural blood patch | Crystalloids, colloids, rEPO, tranexamic acid, fibrin glue, artificial O₂ carriers |
- Record each patient’s choice–variations are common.
Legal & Ethical Landscape
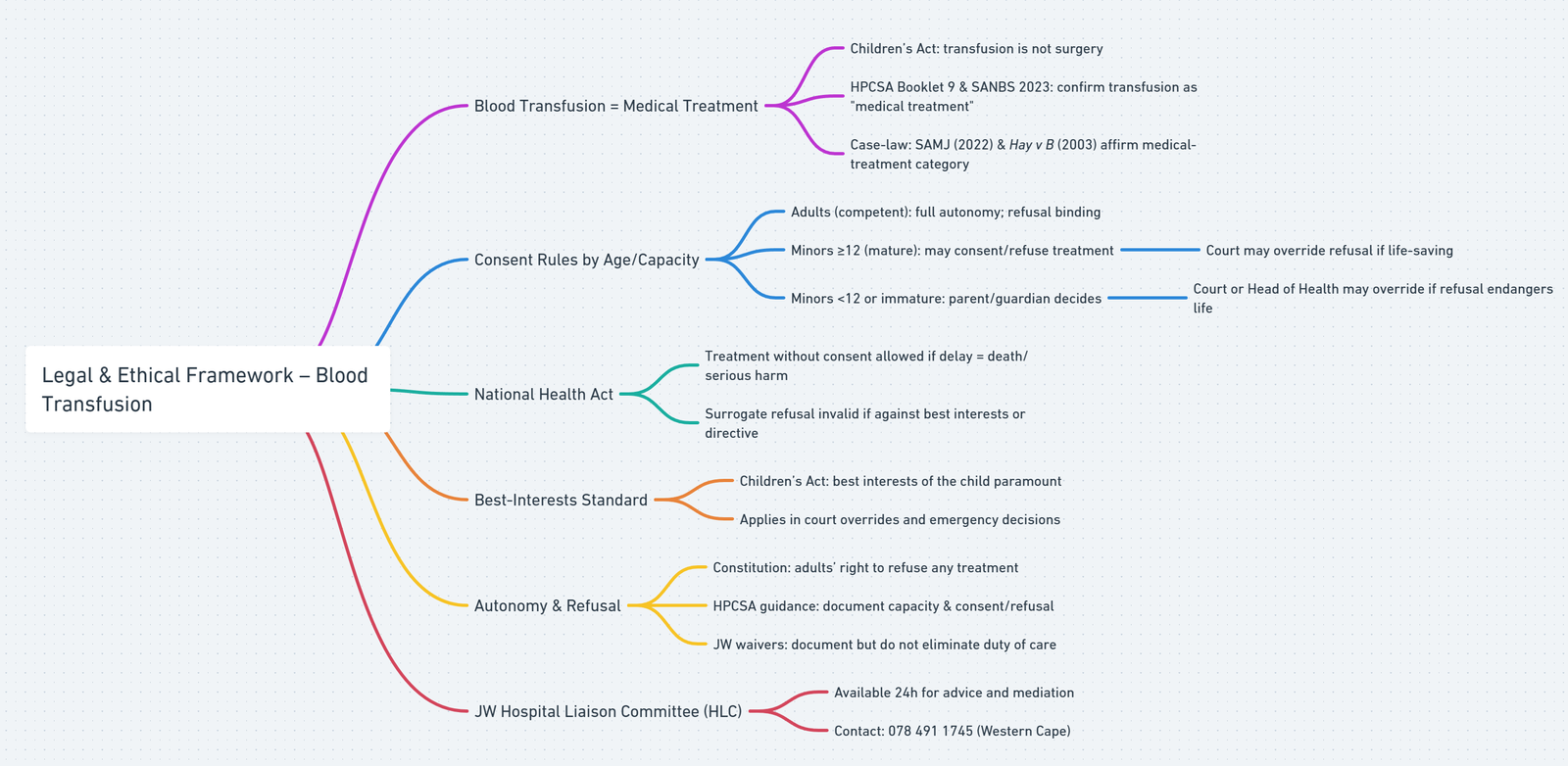
Blood Products
- Blood transfusion = medical treatment under SA law–administration of any substance (incl. blood products) is explicitly listed as “medical treatment,” not “surgical operation” (Children’s Act 38-2005 s 129(2)–(5))
- Consent threshold for minors differs from surgery–a child ≥ 12 yr who is “sufficiently mature” may self-consent or refuse a transfusion, whereas the same child still needs a parent/guardian co-signature for surgery (s 129(2) vs s 129(3))
- Professional guidance aligns–HPCSA Informed Consent Booklet 9 (2021) and the SANBS 2023 transfusion-consent guideline both list transfusion under “medical treatment” requiring specific informed consent
- Case-law commentary supports this view–SAMJ review (112:509-10, 2022) confirms transfusion disputes fall under the Act’s medical-treatment clauses (s 129(2)/(4)), not the surgical clauses (s 129(3)/(5))
- Practical take-aways
- Competent adults: their documented refusal/consent to transfusion is binding.
- Mature minors (≥ 12 yr): may consent to or refuse transfusion, but a court can override refusal if life-saving.
- Younger/immature minors: parent or guardian consents; if refusal jeopardises life, a High-Court order or Head-of-Health authorisation permits transfusion in the child’s best interests
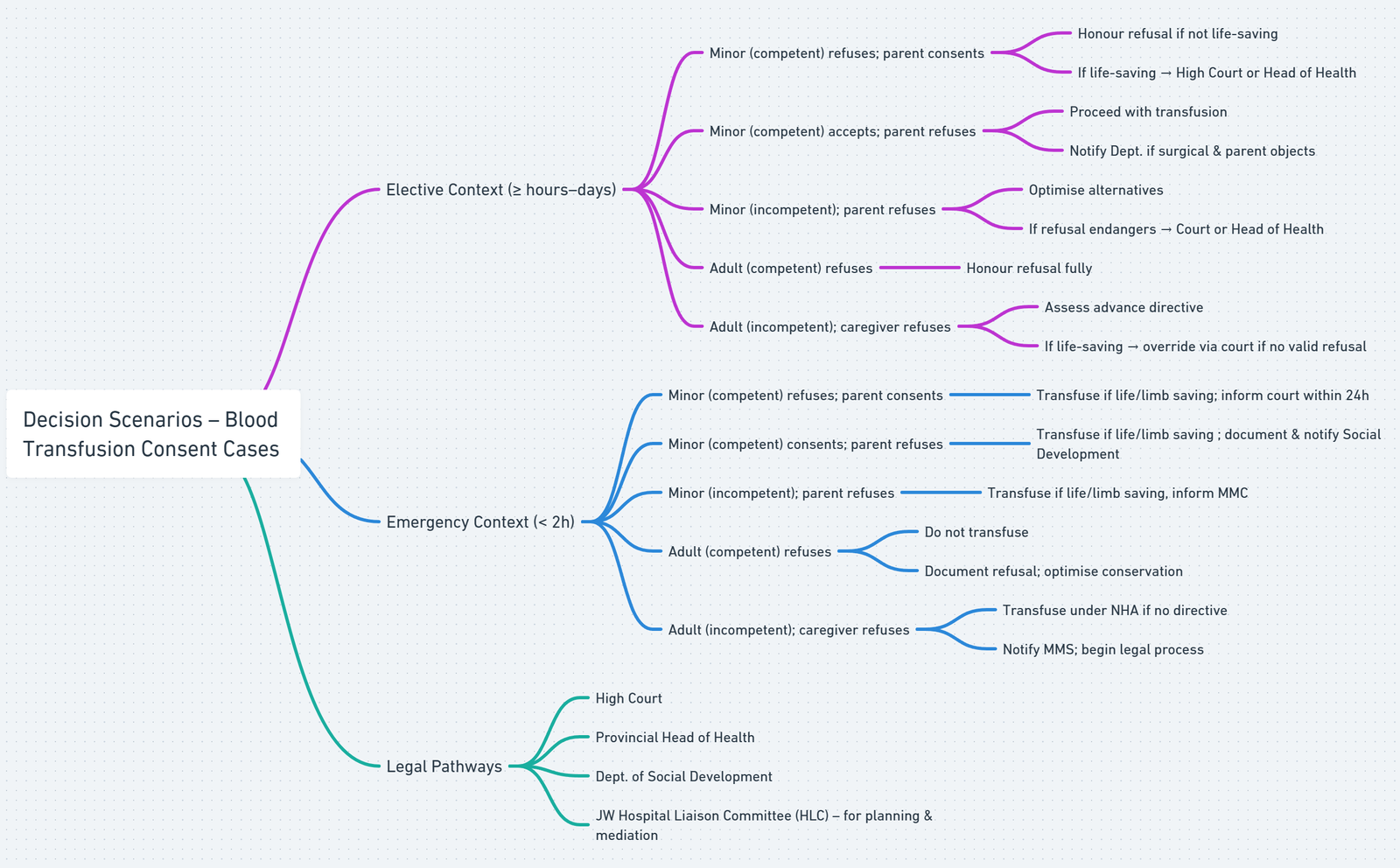
Elective (time Available ≥ hours–days)
| Scenario | Capacity in law | Immediate plan | Escalation / legal route |
|---|---|---|---|
| Minor (12–17 yr) competent, refuses blood; parent says yes | Child may consent to–or refuse–medical treatment (Children’s Act §129 (2)); refusal can be overridden if life-saving | • MDT counselling + JW HLC • Optimise blood-sparing plan • Record child’s refusal & parent consent |
If transfusion is likely life-saving → apply urgently to High Court or Provincial Head of Health for authorisation |
| Minor competent accepts blood; parent says no | Child’s informed consent for medical treatment suffices (CA §129) | Proceed with transfusion if required; document discussion | If procedure is surgical and parent still refuses → Social Development / High-Court consent in child’s best interests |
| Minor incompetent; parent refuses | Parent is default surrogate | Optimise bloodless strategy; involve JW HLC | If refusal endangers life/health → urgent High-Court order or Head-of-Dept authorisation to transfuse |
| Adult competent, refuses blood | Autonomy absolute (Constitution §12) | Honour refusal; document advance directive or blood card; full conservation measures | — |
| Adult incompetent; caregiver refuses | Surrogate decision stands unless it conflicts with best interests or written directive (NHA §7) | Search for advance directive; ethics/MDT review + JW HLC | If transfusion clearly life-saving & no directive → seek High-Court order to override surrogate |
- Children’s Act 38/2005
- §129(2) treats blood transfusion as medical treatment–a mature child (≥ 12 yr) may self-consent or refuse.
- §129(3)–(5) require parental co-signature only for surgical operations.
- §7 states that the best interests of the child are paramount; courts can override parental or child refusal when transfusion is life-saving.
- Hay v B (WLD, 2003) confirms High-Court power to authorise transfusion over a competent minor’s refusal when best-interest test is met.
- National Health Act 61/2003 §7–permits treatment without consent if delay will result in death or serious, irreversible harm and no legally valid refusal or advance directive exists.
- Constitution of South Africa §12 & HPCSA Booklet 9 (2021)–uphold an autonomous adult’s right to accept or refuse any medical intervention, including blood products.
- Surrogate decisions–valid unless they conflict with the patient’s documented wishes or the best-interests test (NHA §7; SAMA medico-legal guidance 2022)
- Release forms: A JW “no-blood” waiver does not remove liability for negligence; it simply records informed refusal. Always document the capacity assessment and alternatives discussed.
- Hospital Liaison Committee (HLC): 24 h JW support line–078 491 1745 (Western Cape). Engage early for elective planning or crisis mediation.
Emergency Framework (<2h)
| Scenario (emergency, < 2 h) | Legal trigger / authority | Immediate action |
|---|---|---|
| Minor (competent) refuses blood; parent consents | Child’s refusal is not decisive if transfusion is life-saving (Children’s Act §7 & §129; High-Court precedent Hay v B, 2003) | Transfuse; record parent’s consent, note child’s objection; inform High Court within 24 h |
| Minor (competent) consents; parent refuses | Child ≥ 12 yr may self-consent to medical treatment (CA §129(2)); parent cannot veto in an emergency | Transfuse immediately; document parental refusal; notify Dept. Social Development |
| Minor incompetent; parent refuses | National Health Act §7(1)(e)–clinician may act without consent to avert death or irreversible harm | Transfuse at once; phone Manager: Medical Services/consultant; write best-interests note; alert Child-Protection team |
| Adult competent refuses | Constitutional autonomy (Bill of Rights §12) & HPCSA Booklet 9–refusal binding even in extremis | Do not transfuse; maximise blood-conservation; counter-sign capacity assessment; contact JW Hospital Liaison Committee |
| Adult incompetent; caregiver refuses | NHA §7(1)(e) allows treatment if delay fatal and no valid advance directive | Begin transfusion while notifying MMS; start urgent court application if time permits |
- Children’s Act §129: blood transfusion = medical treatment–a mature minor’s consent is valid, but a refusal can be overridden when necessary to save life (confirmed in Hay v B, 2003).
- National Health Act §7(1)(e): permits treatment without consent for any patient (child or adult) when delay will cause death or serious, irreversible harm and no valid directive bars it.
- Constitution §12 & HPCSA Booklet 9: a capacitated adult’s refusal of treatment is absolute, including in emergencies.
- Best-interests principle (Children’s Act §7; common-law): for minors or incapacitated adults, clinicians and courts must prioritise survival and long-term welfare, hence the High-Court or Head-of-Dept pathways to authorise transfusion when surrogates refuse.
Links
- Haematology and Blood testing
- Blood conservation
- Blood transfusions and conservation strategies
- Morbidity and mortality in Anaesthesia
References:
- West, James M.. Ethical issues in the care of Jehovah’s Witnesses. Current Opinion in Anaesthesiology 27(2):p 170-176, April 2014. | DOI: 10.1097/ACO.0000000000000053
- Lawson, T. and Ralph, C. (2015). Perioperative jehovah’s witnesses: a review. British Journal of Anaesthesia, 115(5), 676-687. https://doi.org/10.1093/bja/aev161
- Nicola Caine and Karin Zybrands. “The Challenges of Treating Jehovah’s Witnesses.” Medical Protection, May 2014. Accessed July 25, 2024. MPS
- Association of Anaesthetists. Anaesthesia and peri-operative care for Jehovah’s Witnesses and patients who refuse blood. Anaesthesia 2019;74:74-82. anaesthetists.org
- Health Professions Council of South Africa. Guidelines on Informed Consent (Bk 9), 2021.
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
- National Health Act 61/2003, Chapters 2 & 8.
- Children’s Act 38/2005, §129; Regulations 33-47.
- Hay v B 2003 (3) SA 492 (W).
- Nair N. Durban High Court interim order: blood transfusion for JW children. TimesLIVE 26 Feb 2019. timeslive.co.za
- Barrington MJ, Kluger R. Cell salvage in JW surgery. Reg Anesth Pain Med 2023;48:155-63.
- Medical Protection Society. The challenges of treating Jehovah’s Witnesses (Casebook) 2014.
- Malikane, B. H. and McQuoid‐Mason, D. (2022). Right of reply. South African Medical Journal, 509-510. https://doi.org/10.7196/samj.2022.112i8.16603
Summaries
JW
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “91815968-8856-424a-a93f-d7dbabce5d0e”



