{}
Summary
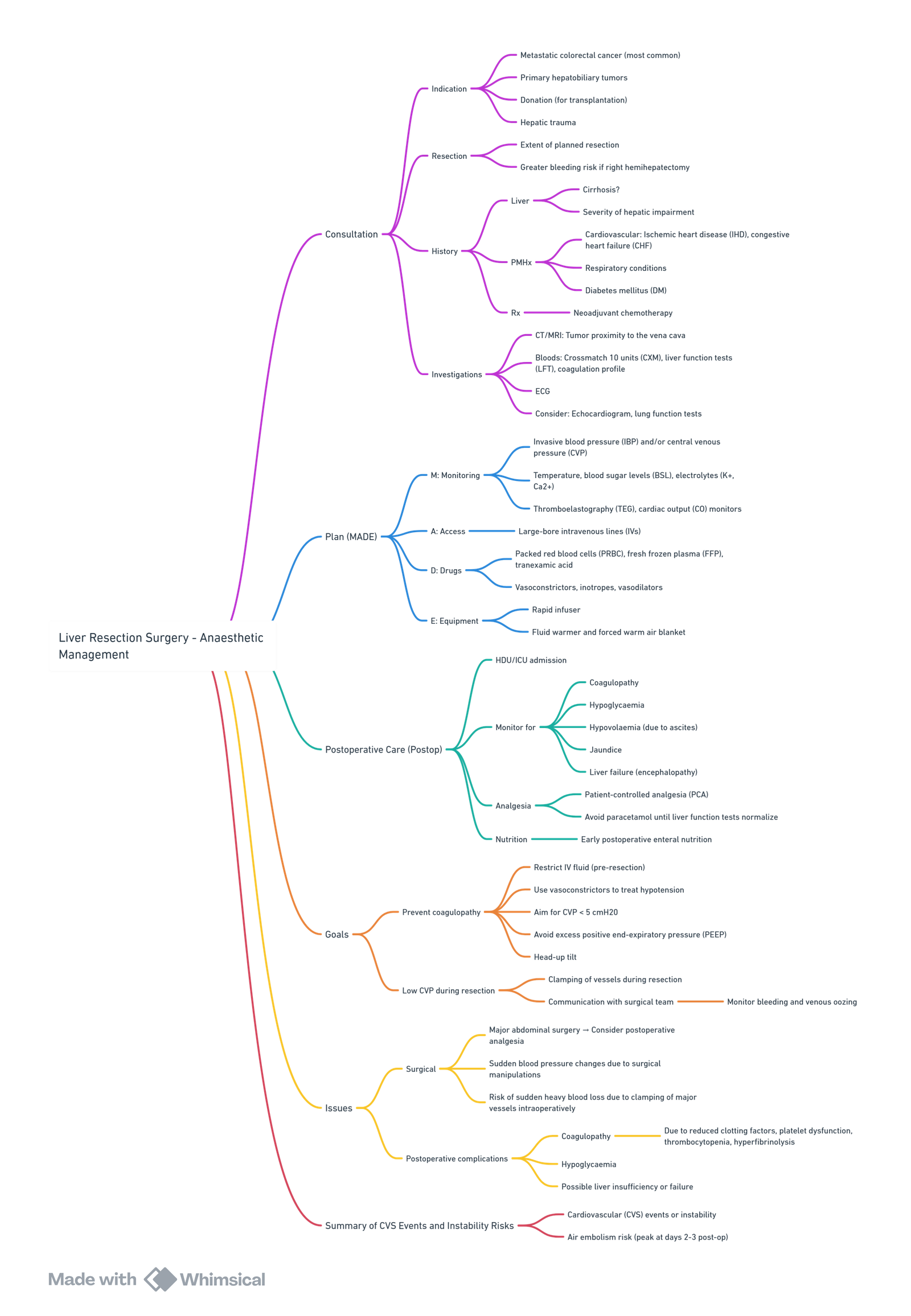
View or edit this diagram in Whimsical.
Background
- Procedures Lobectomy, segmentectomy, wedge resection (open, laparoscopic or robotic).
- Indications Colorectal liver metastases, hepatocellular carcinoma, cholangiocarcinoma, benign tumours (adenoma, FNH), trauma, living‐donor graft retrieval.
- Physiology Receives ≈ 25 % of cardiac output; dual supply: portal vein ≈ 80 %, hepatic artery ≈ 20 %.
- Risk Post-hepatectomy liver failure (PHLF) and multisystem complications increase with cirrhosis, steatosis, cholestasis, chemotherapy-associated liver injury or malnutrition.
Anaesthetic Goals
- Minimise blood loss.
- Preserve residual liver function and prevent ischaemia–reperfusion injury.
- Maintain stable haemodynamics despite vascular occlusion manoeuvres.
- Provide fast-track recovery within an ERAS† pathway.
†Enhanced Recovery After Surgery.
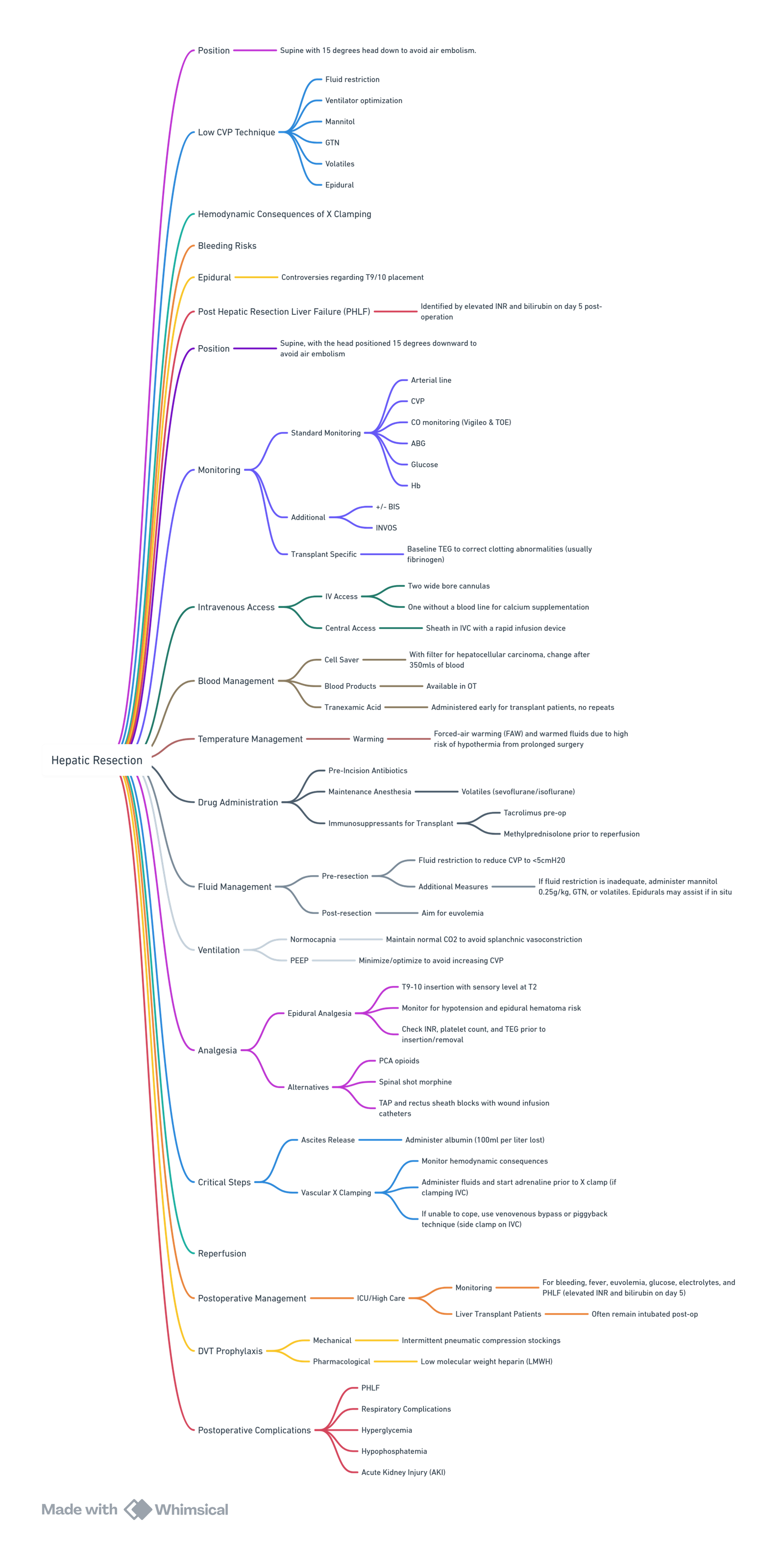
View or edit this diagram in Whimsical.
Pre-operative Management
Assessment
| Domain | Key points |
|---|---|
| History & exam | Alcohol intake, viral hepatitis, previous hepatectomy, chemotherapy, portal hypertension signs. |
| Laboratory | Full blood count (FBC), renal panel, liver function tests (LFT), international normalised ratio (INR), fasting glucose. |
| Imaging & function | CT/MRI volumetry: Future liver remnant (FLR) ≥ 25 % (normal parenchyma), ≥ 35 % (steatosis/chemotherapy), ≥ 40 % (cirrhosis). Indocyanine-green retention at 15 min (ICG-R15) < 10 % for major resection. Elastography or transient elastography for fibrosis staging. |
| Cardiorespiratory reserve | 12-lead ECG, transthoracic echo if cardiac disease, pulmonary function tests (PFT) if significant lung pathology. |
Optimisation & Risk Stratification
- Child–Pugh B/C or MELD > 9: major resection contraindicated; consider two-stage or associating liver partition and portal vein ligation (ALPPS).
- Portal vein embolisation or hepatic vein deprivation to hypertrophy FLR.
- Correct anaemia, cholestasis-related coagulopathy (vitamin K) and nutritional deficits.
Intra-operative Management
Monitoring & Access
- Large-bore peripheral IV × 2 ± rapid infuser; arterial line before induction; central venous catheter (CVC) for vasoactive drugs and low central venous pressure (CVP) strategy.
- Cardiac output monitor or trans-oesophageal echo (TOE) for > 500 mL predicted blood loss or vascular exclusion.
- Cell-salvage permissible (avoid when bile contamination or tumour rupture).
Anaesthetic Technique
| Aspect | Current practice |
|---|---|
| Maintenance | Volatile (desflurane / isoflurane) or propofol-TIVA; avoid halothane. Neuromuscular block with atracurium / cisatracurium. |
| Low-CVP period | Target CVP < 5 mm Hg during parenchymal transection: restrict crystalloids to ≤ 1 mL kg⁻¹ h⁻¹, reverse Trendelenburg, diuretics or low-dose GTN, minimised PEEP. |
| Fluid strategy | Balanced acetate solution; goal-directed haemodynamic therapy (GDHT) with stroke-volume optimisation superior to fixed restrictive or liberal regimens. Albumin for blood loss > 25 % blood volume. |
| Blood conservation | Intermittent Pringle manoeuvre 15 min clamp / 5 min reperfusion; topical fibrin sealant; recent evidence does not support routine tranexamic acid (TXA) because of uncertain efficacy and possible thrombo-embolism. |
| Hepatic vascular occlusion | Haemodynamic effects • Total hepatic vascular exclusion (THVE): ↑SVR ≈ 80 %, ↓CO ≈ 60 % → anticipate norepinephrine bolus/infusion. • Selective hepatic vascular exclusion (SHVE): modest MAP rise, mild CO fall. Use incremental vasopressors and volume to maintain MAP ≥ 65 mm Hg. |
| Metabolic protection | Maintain normothermia, normoglycaemia 5–9 mmol L⁻¹; 10 % dextrose infusion if clamp > 30 min; correct ionised Ca²⁺. Evidence for prophylactic N-acetyl-cysteine is inconclusive–individualise. |
| Analgesia | Thoracic epidural effective but evaluate coagulation; alternatives: erector-spinae plane (ESP) catheter, wound infiltration or IV lidocaine infusion. |
Emergence
- Reverse neuromuscular block with sugammadex 2–4 mg kg⁻¹.
- Extubate if normothermic, haemodynamically stable and no severe acidosis. Major/complex resections often ventilated overnight in ICU.
Post-operative Care
| Focus | Management |
|---|---|
| PHLF surveillance | Daily INR and bilirubin; “50-50” rule (bilirubin > 50 µmol L⁻¹ & INR > 1.5 on day 5) predicts mortality–escalate early. |
| Coagulopathy | Point-of-care viscoelastic testing guides fibrinogen, platelets or PCC; avoid routine FFP. |
| Glucose & electrolytes | Continuous dextrose 5 % / 10 % if glucose < 4.5 mmol L⁻¹; replace phosphate aggressively (< 0.8 mmol L⁻¹ impairs regeneration). |
| Fluid | Balanced crystalloids; target urine ≥ 0.5 mL kg⁻¹ h⁻¹; diuretics for ascites if CVP high. |
| Analgesia & ERAS | ESP/epidural infusion + regular paracetamol ± COX-2 inhibitor (safe if no AKI), early mobilisation (day 0), oral intake within 6 h, no routine nasogastric tube or drains. |
| Complications | Haemorrhage, bile leak, pleural effusion, venous air embolism; maintain low threshold for CT if haemodynamics unstable or rising bilirubin. |
Complications after Hepatic Resection Surgery
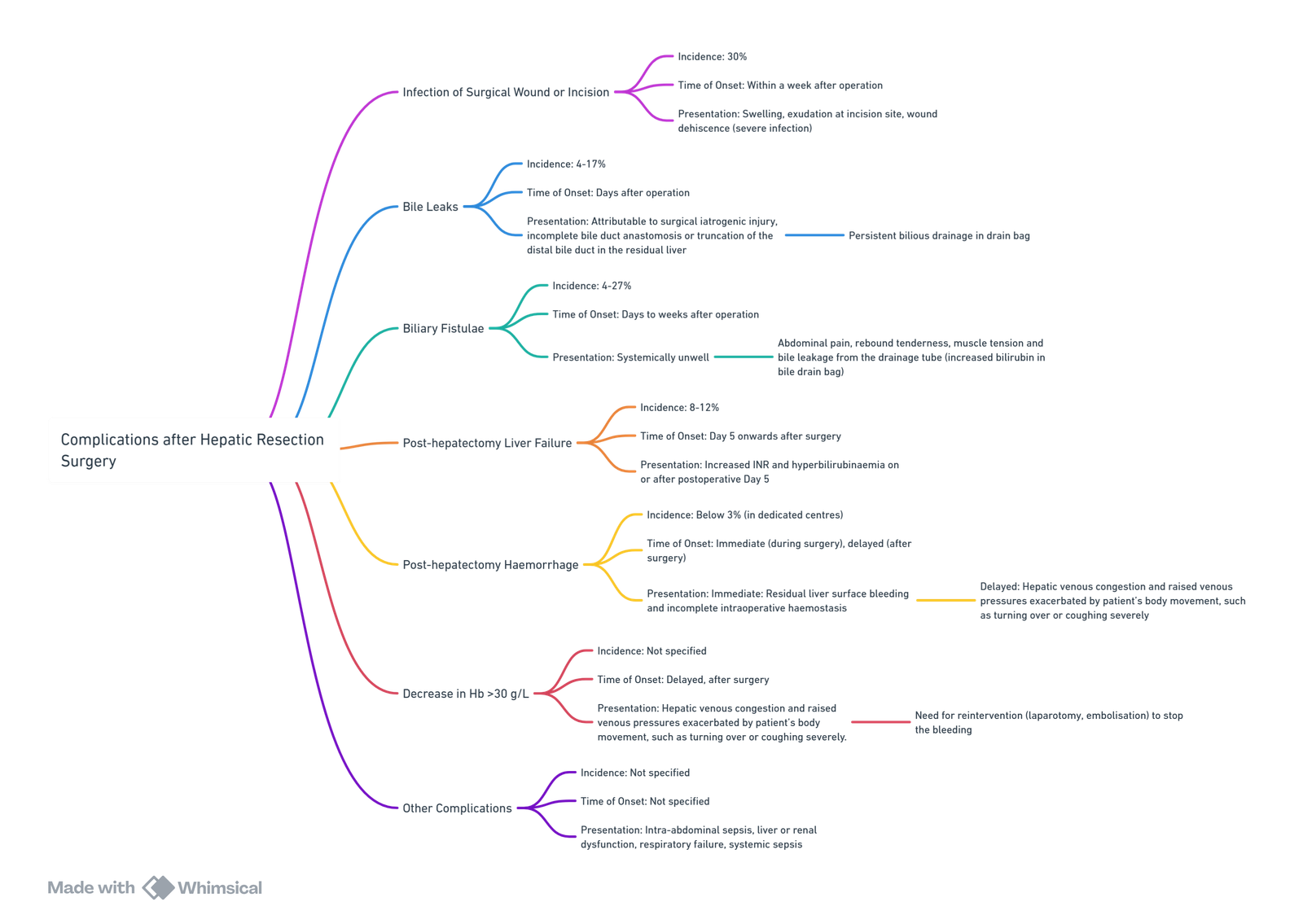
View or edit this diagram in Whimsical.
Enhanced Recovery After Surgery (ERAS) Protocol Elements for Liver Surgery 2022
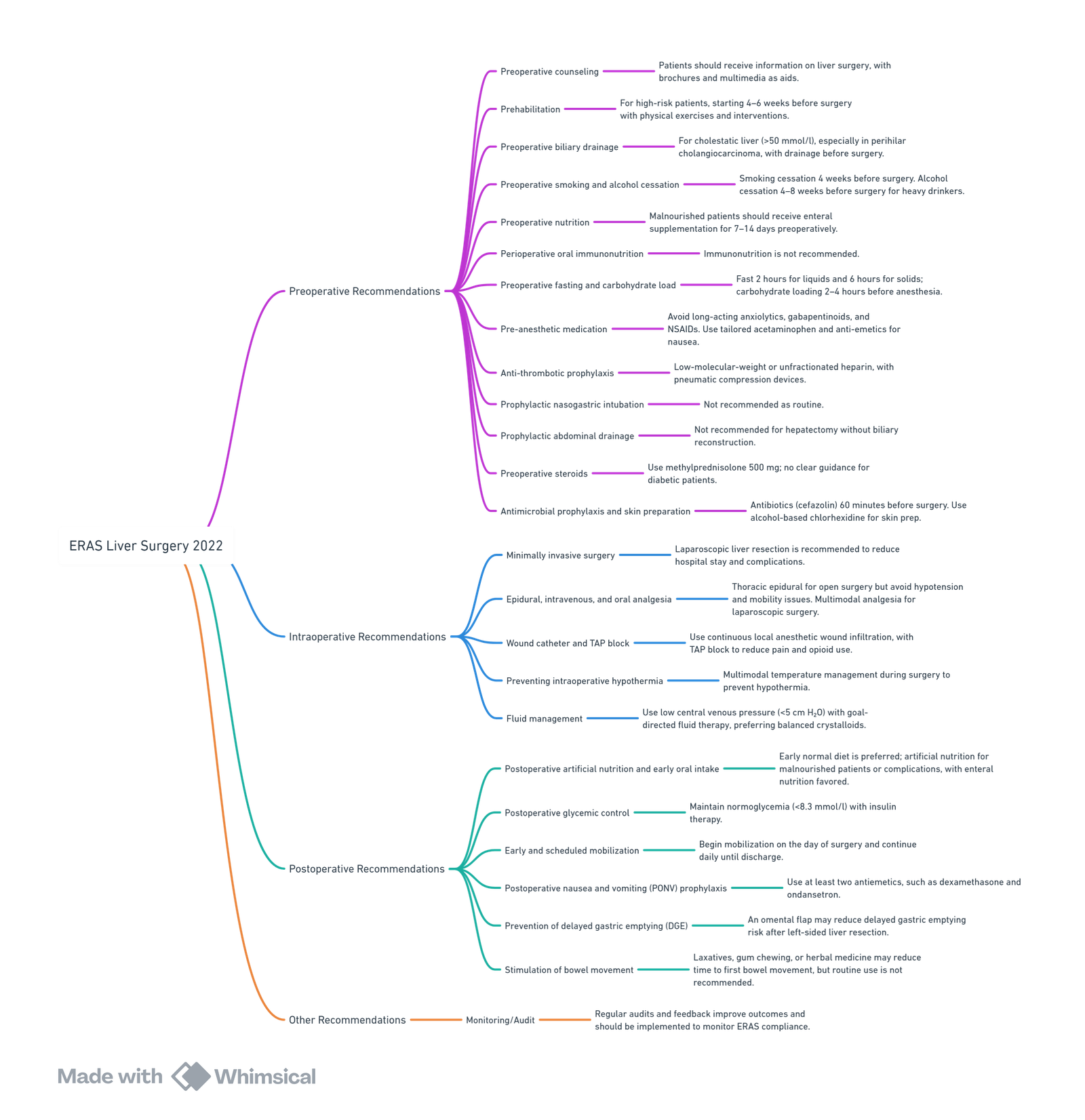
View or edit this diagram in Whimsical.
Preoperative Recommendations
- Preoperative counseling
- Patients should receive preoperative information and counseling on liver surgery. Brochures and multimedia may help improve verbal counseling.
- Prehabilitation
- Recommended for high-risk patients (e.g., elderly, malnourished, overweight, smokers, or those with psychological disorders). Prehabilitation should start 4–6 weeks before surgery, focusing on physical exercises and other interventions. Specific content is not standardized.
- Preoperative biliary drainage
- Recommended in cholestatic liver (>50 mmol/l), particularly for perihilar cholangiocarcinoma, via percutaneous or endoscopic drainage. Surgery should wait until bilirubin drops below 50 mmol/l.
- Preoperative smoking and alcohol cessation
- Smoking cessation is advised 4 weeks preoperatively. Alcohol cessation is recommended for heavy drinkers (≥24 g/day for women and ≥36 g/day for men) at least 4–8 weeks before surgery.
- Preoperative nutrition
- Malnourished patients (e.g., weight loss >10% or >5% in 3 months, low BMI, or low fat-free mass) should receive enteral supplementation for at least 7–14 days preoperatively.
- Perioperative oral immunonutrition
- Immunonutrition is not recommended due to lack of evidence.
- Preoperative fasting and carbohydrate load
- Patients should fast 2 hours for liquids and 6 hours for solids before surgery. Carbohydrate loading is recommended 2–4 hours before anesthesia to improve insulin resistance, though the effect on length of stay is unclear.
- Pre-anesthetic medication
- Long-acting anxiolytics should be avoided, especially in elderly patients. Gabapentinoids and NSAIDs are not recommended. Preoperative acetaminophen should be dose-adjusted to the extent of resection. Anti-emetic patches may be used in patients at risk of postoperative nausea.
- Anti-thrombotic prophylaxis
- Low-molecular-weight heparin or unfractionated heparin is recommended to reduce thromboembolic risk, starting postoperatively unless contraindicated. Intermittent pneumatic compression devices are also suggested.
- Prophylactic nasogastric intubation
- Routine prophylactic nasogastric intubation is not recommended as it does not improve outcomes and may increase hospital stay.
- Prophylactic abdominal drainage
- Routine abdominal drain placement is not recommended for hepatectomy without biliary reconstruction, though it may be considered for biliary reconstruction cases.
- Preoperative steroids
- Steroid administration (methylprednisolone 500 mg) is recommended. No specific recommendation for diabetic patients due to lack of data
- Antimicrobial prophylaxis and skin preparation
- Antibiotics (e.g., cefazolin) should be given 60 minutes before surgery. In complex surgeries, targeted regimens may be needed. Skin preparation with alcohol-based chlorhexidine is recommended.
Intraoperative Recommendations
- Minimally invasive surgery
- Laparoscopic liver resection is recommended in trained teams, as it reduces length of stay and complication rates.
- Epidural, postoperative intravenous, and postoperative per oral analgesia
- For open liver surgery, thoracic epidural analgesia provides excellent pain relief but has disadvantages (e.g., hypotension, mobility issues). Multimodal analgesia is recommended to avoid these risks. No regional anesthesia is needed for laparoscopic surgery; multimodal analgesia with intravenous opioids is preferred.
- Wound catheter and transversus abdominis plane (TAP) block
- Continuous local anesthetic wound infiltration reduces complication rates and provides similar analgesia to thoracic epidural. Adding a TAP block improves pain control and reduces opioid use.
- Preventing intraoperative hypothermia
- Multimodal temperature management (e.g., warming garments or forced warm air) should be used during open and minimally invasive liver surgery to prevent hypothermia.
- Fluid management
- Low central venous pressure (<5 cm H₂O) with close monitoring is advised during hepatic transection. Balanced crystalloids are preferred over saline or colloids for maintenance fluid therapy. Goal-directed fluid therapy may improve outcomes in patients with low venous pressure states or reduced cardiac function.
Postoperative Recommendations
- Postoperative artificial nutrition and early oral intake
- Early oral intake with a normal diet is recommended post-hepatectomy. Artificial nutrition may be required for malnourished patients or those with complications. Enteral over parenteral nutrition is preferred if necessary.
- Postoperative glycemic control
- Insulin therapy to maintain normoglycemia (<8.3 mmol/l) is recommended postoperatively.
- Early and scheduled mobilization
- Early mobilization (out of bed) after liver surgery should begin on the day of surgery and continue daily until discharge.
- Postoperative nausea and vomiting (PONV) prophylaxis
- Multimodal PONV prophylaxis is recommended with at least two antiemetics, such as dexamethasone and ondansetron.
- Prevention of delayed gastric emptying (DGE)
- Use of an omental flap to cover the cut liver surface may reduce delayed gastric emptying risk after left-sided liver resection.
- Stimulation of bowel movement
- Postoperative laxatives, gum chewing, herbal medicine, or decoctions may reduce time to first flatus or stool, but current evidence is insufficient for routine recommendation.
Other Recommendations
- Monitoring/Audit
- Auditing and feedback are associated with better outcomes in surgery. These should be implemented and performed to monitor and improve compliance with ERAS guidelines.
Links
References:
- Liver resection and anaesthesia L Gilliland. Wits refresher 2018
- Patel, J., Jones, C., & Amoako, D. (2022). Perioperative management for hepatic resection surgery. BJA Education, 22(9), 357-363. https://doi.org/10.1016/j.bjae.2022.05.002
- oliat GR, Kobayashi K, Hasegawa K, Thomson JE, Padbury R, Scott M, Brustia R, Scatton O, Tran Cao HS, Vauthey JN, Dincler S, Clavien PA, Wigmore SJ, Demartines N, Melloul E. Guidelines for Perioperative Care for Liver Surgery: Enhanced Recovery After Surgery (ERAS) Society Recommendations 2022. World J Surg. 2023 Jan;47(1):11-34. doi: 10.1007/s00268-022-06732-5. Epub 2022 Oct 30. PMID: 36310325; PMCID: PMC9726826.
- British Journal of Anaesthesia Education. Peri-operative management for hepatic resection surgery. 2022. bjaed.org
- ERAS® Society. Guidelines for peri-operative care for liver surgery. 2022. pmc.ncbi.nlm.nih.gov
- Lancet eClinicalMedicine. Systematic review of goal-directed fluid therapy in major surgery. 2024. thelancet.com
- PubMed. Restricted versus liberal versus goal-directed fluids for liver resection: network meta-analysis. 2023. pubmed.ncbi.nlm.nih.gov
- Tranexamic acid in liver resection: multicentre randomised trial. 2024. pmc.ncbi.nlm.nih.gov
- Safety and efficacy of TXA in hepatic surgery: meta-analysis. 2025. sciencedirect.com
- N-acetyl-cysteine to mitigate liver ischaemia–reperfusion injury: narrative review. 2024. journals.lww.com
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “ca038946-3dc7-46a1-9cfc-27830cb48bf2”



