{}
Indications & Listing Criteria
| Setting | Recommended listing trigger (2024 EASL & AASLD guidance) |
|---|---|
| Chronic liver disease | • MELD-Na ≥ 15 (or rapid rise ≥ 5 points / 3 months) • Child–Pugh B/C with ≥ 1 de-compensating event (refractory ascites, GI bleed, hepatorenal syndrome, encephalopathy) • Hepatocellular carcinoma within Milan criteria or down-staged into them |
| Acute liver failure (ALF) | King’s College criteria (updated 2023): –Paracetamol: arterial pH < 7.30 or INR > 6.5 + creatinine > 300 µmol L⁻¹ + grade III–IV encephalopathy. –Non-paracetamol: INR > 6.5 or any 3 of: age < 18 or > 40, jaundice-to-encephalopathy > 7 d, INR > 3.5, bilirubin > 300 µmol L⁻¹, aetiology = indeterminate / HBV / idiosyncratic DILI. |
Contra-indications to Elective Liver Transplant
| Absolute | Relative (require MDT discussion) |
|---|---|
| Uncontrolled sepsis, irreversible multi-organ failure, untreated malignancy with vascular/extra-hepatic spread, severe pulmonary HTN (mPAP > 45 mmHg), MELD-Na < 12, active substance abuse, non-adherence. | Age > 70 y, BMI > 40 kg m⁻², portal-vein thrombosis, significant CAD, high frailty index, active extra-hepatic infection, HIV with unsuppressed viral load. |
Conduct of Anaesthesia (recipient)
Considerations
| Surgical Phase | Surgical Considerations | Anesthetic Considerations |
|---|---|---|
| Preoperative | Transplantation evaluation (psychological evaluation, MELD score, UNOS listing) | Preoperative evaluation, vascular access, blood product availability |
| Dissection | Surgical incision, mobilization of liver and vascular structures, isolation of bile duct | Hemodynamic compromise from loss of ascites, hemorrhage during dissection, decreased venous return |
| Anhepatic | Clamping of hepatic artery and portal vein, removal of diseased liver, anastomosis of IVC and portal vein of donor liver | Hemodynamic compromise from clamping IVC, metabolic (lactic) acidosis, hypocalcemia from citrate intoxication, hyperkalemia, hypothermia, hypoglycemia |
| Reperfusion | Anastomosis of hepatic artery and biliary system, reperfusion of transplanted liver | Hemodynamic instability, dysrhythmias, hyperkalemia, acidosis, cardiac arrest |
| Posttransplantation | Hemostasis, evaluation of graft function, ultrasound for vascular patency | ICU admission, early or late extubation, hemodynamic management |
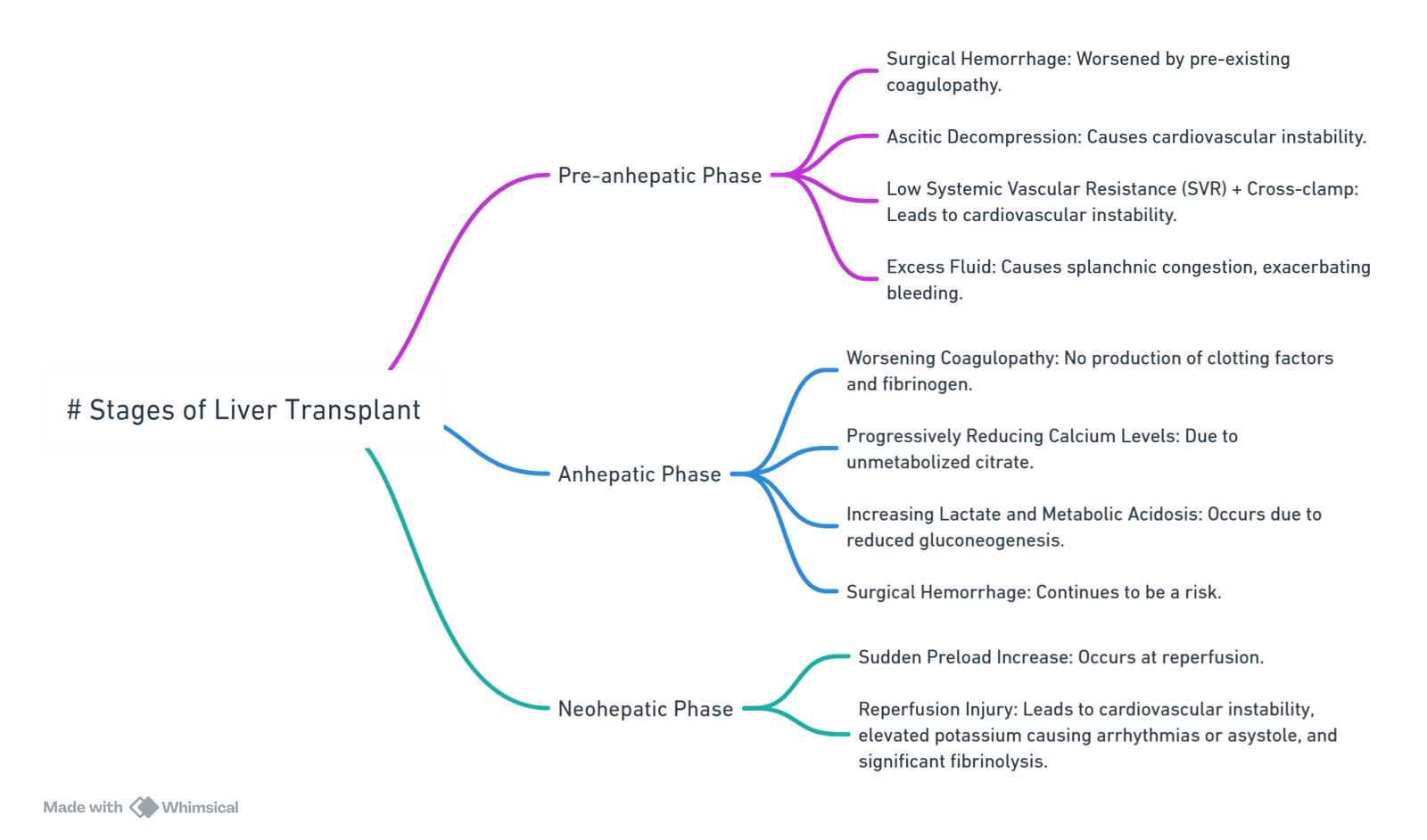
View or edit this diagram in Whimsical.
Surgical Considerations
Surgical Phases of Liver Transplant Procedure and Common Anaesthetic Problems
| Phase | Surgical Details | Common Anaesthetic Problems |
|---|---|---|
| Pre-anhepatic | Inverse T or extended/bilateral subcostal incision Mobilization of the structures around the liver and porta hepatis Hepatic artery and bile duct divided |
Hemorrhage from dissection, varices, and adhesions Cardiovascular instability from ascitic decompression Low SVR state causes hypotension, exacerbated by vasodilatation of blood away from central compartment towards splanchnic circulation |
| Anhepatic | Portal vein and hepatic veins divided Explantation of native liver IVC preparation for implantation New liver inserted Caval and portal anastomoses fashioned |
No production of clotting factors, fibrinogen deficiency, and worsening coagulopathy Progressive hypocalcemia Absent citrate/lactate metabolism, reduced gluconeogenesis, increasing serum lactate Worsening metabolic acidosis |
| Neo-hepatic | Graft reperfusion Hepatic artery anastomosis Biliary reconstruction |
Hypotension and further decrease in SVR Sudden preload increase at reperfusion Worsening metabolic acidosis |
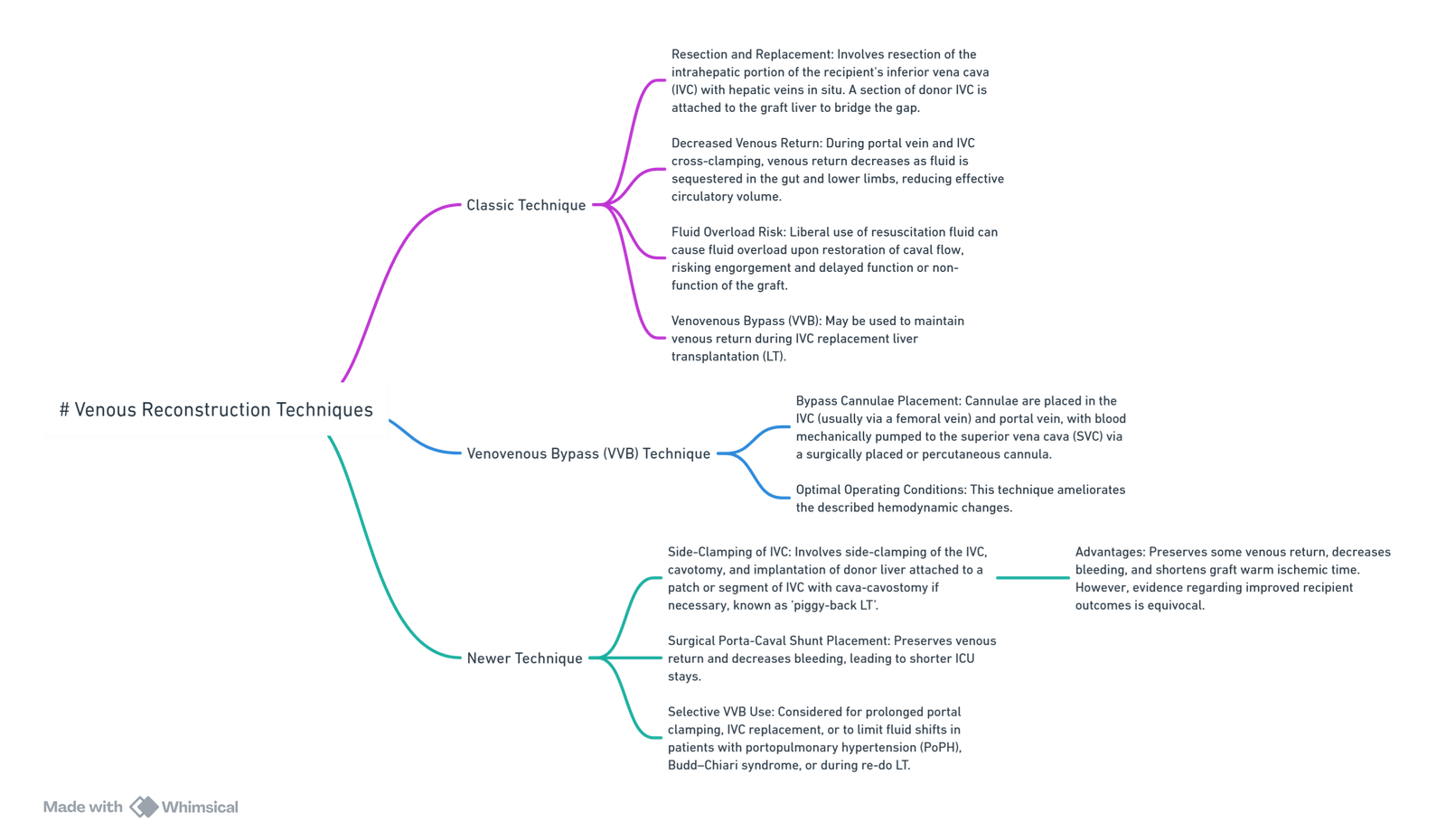
View or edit this diagram in Whimsical.
Preparation
- Two large-bore IVs, rapid infuser, arterial line before induction, quad-lumen CVC (internal jugular) + introducer sheath for rapid blood/fluid.
- Cell-salvage and point-of-care visco-elastic testing (TEG 6s® / ROTEM sigma®).
- Baseline ABG, ionised Ca²⁺, lactate, glucose, temperature.
- Blood products: ≥ 10 units PRBC, 10 FFP, fibrinogen concentrate, PCC, platelets.
Induction & Maintenance
| Phase | Haemodynamic priorities | Common interventions |
|---|---|---|
| Dissection (pre-anhepatic) | Low SVR, haemorrhage from varices/adhesions | Norepinephrine 0.05-0.15 µg kg⁻¹ min⁻¹, permissive low CVP (< 8 mmHg), balanced transfusion guided by VET. |
| Anhepatic | Loss of venous return after IVC/portal clamping, citrate load | Calcium chloride 5–10 mmol q30 min, NaHCO₃ if pH < 7.20, keep temp > 36 °C. |
| Reperfusion | Post-reperfusion syndrome (PRS)–MAP ↓ > 30 % for ≥ 1 min ± arrhythmia | 100 mg CaCl₂ + 0.5 mg phenylephrine bolus at unclamp, epinephrine 0.05-0.1 µg kg⁻¹ min⁻¹ if PRS, insulin + glucose for K⁺ > 5.5 mmol L⁻¹. |
- Volatile (desflurane/isoflurane) or propofol-TIVA (does not worsen PRS).
- Sugammadex 4 mg kg⁻¹ enables immediate reversal if extubation planned.
Coagulation Strategy (TEG-guided)
| TEG/ROTEM abnormality | First-line treatment |
|---|---|
| Prolonged R / CT (> 1.5 × baseline) | 15 mL kg⁻¹ FFP or PCC 25 IU kg⁻¹ |
| α-angle < 45° or FIBTEM A5 < 8 mm | Fibrinogen concentrate 3–4 g |
| MA / MCF < 45 mm (thrombocytopenia) | Platelets 1 pool (≈ 4–6 units) |
| LI30 > 8 % (hyperfibrinolysis) | TXA 15 mg kg⁻¹ (avoid after reperfusion if thrombotic risk high) |
Special Peri-operative Issues
| Complication | Prevention / Management |
|---|---|
| Hypocalcaemia (citrate) | Ionised Ca²⁺ every 15 min; CaCl₂ 5 mmol per 4 units PRBC/FFP. |
| Hyperkalaemia at reperfusion | Flush liver with 1 L cold albumin-Ringer’s; Ca²⁺, insulin-dextrose, gentle ventilation. |
| Hepato-renal syndrome | Pre-op vasoconstrictor + albumin protocol (telipressin or norepi) improves outcome |
| Severe post-reperfusion hypoxaemia | 100 % FiO₂ > 5 min + head-down; inhaled prostacyclin 30–50 ng kg⁻¹ min⁻¹ → iNO 20 ppm → methylene blue 1.5 mg kg⁻¹; escalate to VV-ECMO algorithm. |
Post-operative Care
| Time-frame | Key issues & surveillance |
|---|---|
| First 24 h | PRS-related vasoplegia, bleeding, early allograft dysfunction (AST/ALT > 2000 IU L⁻¹ + INR > 1.6 + bilirubin > 100 µmol L⁻¹/Day 3), hypocalcaemia, AKI (KDIGO). |
| Days 2-7 | Biliaryor vascular-compromise Doppler, infection screen, rejection (↑ LFT), careful diuresis for ascites. |
| Late | Immunosuppression toxicity (calcineurin-induced HTN/AKI, PTDM), metabolic syndrome, recurrent disease. |
- Early extubation (within 6 h) is feasible in haemodynamically stable, normothermic recipients with PaO₂/FiO₂ > 200 mmHg and minimal vasopressor need.
Donor Considerations
- Patient Selection:
- Donors should be fit and healthy (ASA I – II). Confirm fitness pre-operatively.
- Monitoring:
- Use an arterial line (A-line).
- Central venous pressure (CVP) monitoring.
- Large bore peripheral line.
- Anaesthetic Technique:
- Standard general anaesthesia (GA).
- Cisatracurium is not mandatory; rocuronium with or without sugammadex can be used.
- Analgesia:
- Epidural analgesia and/or rectus sheath catheter for midline incisions.
- Fluid Management:
- Restrict fluids until after the hepatectomy to reduce bleeding (maintain CVP at 4-5 mmHg).
Acute Liver Failure Management
- Cardiovascular System (CVS):
- Profound vasodilation and circulatory collapse may occur.
- Volume replacement guided by cardiac output (CO) monitoring and the use of vasopressors as needed.
- Coagulation:
- Check prothrombin time (PT) every 12 hours.
- Do not correct PT routinely; correct only if there is acute hemorrhage or before invasive procedures.
- Renal Function:
- Use renal replacement therapy (RRT) for oliguric/anuric renal failure.
- Continuous venovenous hemodialysis (CVVHD) with lactate-free dialysate is preferred.
- Infection Control:
- Routine infection screening.
- Administer antibiotics only for Grade 3-4 encephalopathy.
- Glycaemic Control:
- Patients are prone to hypoglycemia.
- Monitor blood glucose every 2 hours and correct as needed.
- Initiate early enteral nutrition.
- Intracranial Pressure (ICP) Management:
- Consider ICP monitoring for Grade 3 or 4 encephalopathy.
- Maintain ICP < 20 mmHg.
- Specific Therapies:
- Consider N-acetylcysteine (NAC) for all patients with acute liver failure (ALF).
- Administer antivirals for acute hepatitis B.
- Liver Replacement Therapies:
- Use Molecular Adsorbent Recirculating System (MARS) or Prometheus as a bridge to transplantation.
Anaesthetic Concerns in Recipients of Liver Transplants Presenting for Non-Transplant Surgery
- Paracetamol:
- Safe to use.
- Hepatitis Recurrence:
- Monitor for recurrence of hepatitis.
- Reversal of Pre-Transplant Issues:
- Early Post-Transplant (Days to Weeks):
- Portal hypertension, ascites, pleural effusions.
- Intermediate Post-Transplant (Weeks to Months):
- Encephalopathy, pulmonary hypertension (PHT), hepatopulmonary syndrome, hepatorenal syndrome.
- Risk of prolonged emergence from anesthesia due to hypoalbuminemia and any residual encephalopathy.
- Long-Term Considerations:
- Post-transplant hypertension (due to steroids and cyclosporine), increasing the risk of cardiac events.
- Hepatopulmonary syndrome may persist; pulmonary hypertension may take months to improve.
- Cirrhotic cardiomyopathy can cause heart failure post-transplant.
- Renal failure can be secondary to liver disease or immunosuppression.
- Metabolic issues such as hyperlipidemia, diabetes mellitus, and non-alcoholic liver disease may arise.
- Early Post-Transplant (Days to Weeks):
Links
- Brainstem death
- Transplants and organ donation
- Liver resection
- ICU and liver disease
- Liver physiology and pathology
References:
- Kashimutt, S. and Kotzé, A. (2017). Anaesthesia for liver transplantation. BJA Education, 17(1), 35-40. https://doi.org/10.1093/bjaed/mkw031
- Brezeanu LN, Brezeanu RC, Diculescu M, Droc G. Anaesthesia for Liver Transplantation: An Update. J Crit Care Med (Targu Mures). 2020 May 6;6(2):91-100. doi: 10.2478/jccm-2020-0011. PMID: 32426515; PMCID: PMC7216023.
- Fabbroni, D. and Bellamy, M. C. (2006). Anaesthesia for hepatic transplantation. Continuing Education in Anaesthesia Critical Care &Amp; Pain, 6(5), 171-175. https://doi.org/10.1093/bjaceaccp/mkl040
- EASL Clinical Practice Guidelines on Liver Transplantation. J Hepatol. 2024. journal-of-hepatology.eu
- American Association for the Study of Liver Diseases (AASLD). Principles of Patient Selection for Liver Transplantation. 2023. sciencedirect.com
- Peri-operative coagulopathy management with PCC in LT–randomised trial. Br J Anaesth. 2023. pmc.ncbi.nlm.nih.gov
- Post-reperfusion syndrome update 2024. World J Hepatol. pmc.ncbi.nlm.nih.gov
- Goal-directed haemodynamic therapy after LT (COLT trial). Transplant Evidence Watch 2024. transplantevidence.com
- Telipressin plus albumin for hepatorenal syndrome: meta-analysis. Clin Gastroenterol Hepatol. 2023. easl.eu
Summaries
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “63d2da6d-b489-4849-bfe1-85ecafba4493”



