- Neuraxial Ultrasound Approach: Systematic Approach to Ultrasound-Guided Neuraxial Block by a Midline Approach
- Ultrasound for Lumbar Spinal and Epidural Anaesthesia: Current Evidence
- Links
{}
Neuraxial Ultrasound Approach: Systematic Approach to Ultrasound-Guided Neuraxial Block by a Midline Approach
- Video guidance
- [Claire Spinal video](https://drive.google.com/file/d/1e0A2UqkYXjhY2G2lvZN7zTUVlS81skGZ/view?usp=drive_link (Claire video))
Equipment & Patient Set-up
- Probe–2–6 MHz curved array for adults; 5–10 MHz linear for slim adults, paediatrics or thoracic scanning.
- Position–sitting or lateral decubitus with flexed hips/knees; table height so probe hand and eye line are level.
- Ergonomics & sterility–non-sterile gel for scouting; sterile cover/gel if real-time scanning after skin prep.
Four-step Scanning Algorithm
| Step | Probe manoeuvre | Sonographic landmarks | Purpose |
|---|---|---|---|
| PSTP | Parasagittal, 3–4 cm off midline | “Trident” shadows of transverse processes, psoas, erector spinae | Identify lumbar segment & depth orientation |
| PSAP | Slide medially | Continuous hyperechoic articular-process line | Track towards midline |
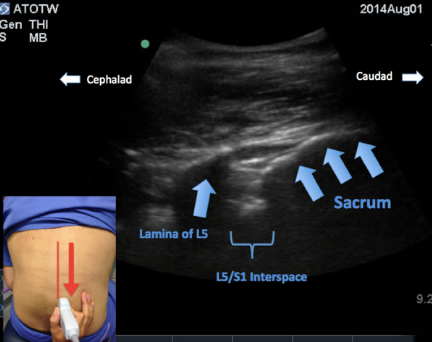
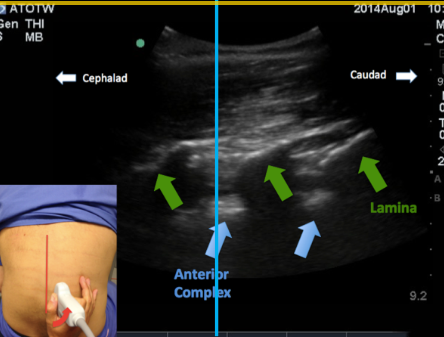
| PSO | From PSAP, tilt medially | Lamina “saw-tooth”; posterior & anterior complexes | Visualise interlaminar window |
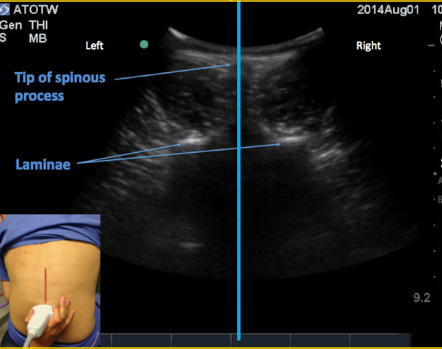
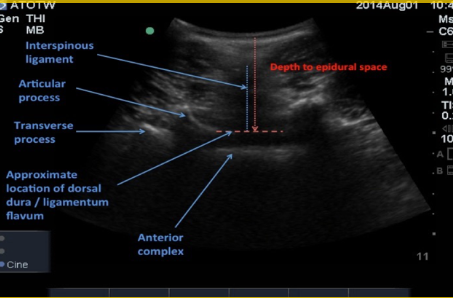
| TI | Rotate 90°, centre midline | Anterior complex ± faint posterior complex | Confirm interspace, measure depth |
Skin Marking & Depth Estimation
- In PSO view slide caudad until sacrum (continuous bright line) ⇒ L5–S1.
- Mark successive interspaces cephalad on skin at probe mid-edge.
- In TI view centre midline/interspace ➔ cross-mark intersection = needle entry.
- Measure skin-to-posterior-complex distance on screen (usually accurate ± 0.5 cm).
Needle Insertion (midline)
- Insert at 85–90° copying the cephalad probe tilt.
- Use loss-of-resistance or CSF flow to confirm entry; limit redirections to fine (<10°) adjustments.
Paramedian US-guided Approach
- Indications–narrowed interspinous spaces, ossified ligaments, previous surgery.
- Mark midline & two adjacent spinous processes in transverse view.
- Needle entry = 1 cm lateral to midline and 1 cm caudal to upper spinous mark; advance 5–10° medial/cephalad alongside lamina.
Special Situations & Tips
- Obesity / parturients (BMI > 35 kg m⁻²)–deeper setting, increase depth & gain; US halves attempts/time.
- Scoliosis / instrumentation–scan both sides; choose widest window; consider high-frequency probe to visualise hardware.
- Paediatrics–linear probe; structures superficial & well defined.
- Real-time (in-plane/out-of-plane)–useful for difficult epidurals but needs sterile cover and advanced skill; current evidence shows no clear advantage over pre-scan mapping.
Troubleshooting
- Poor image–lower frequency, rock/tilt to eliminate anisotropy, adjust depth/gain.
- Sacrum mistaken for lamina–sacrum appears as a long, unbroken hyperechoic line.
- Depth over-estimate–ensure beam perpendicular to ligamentum flavum–dura complex.
Competency & Governance
- RA-UK 2024 recommends ≥ 20 supervised scans to attain basic competence; keep a logbook of success rates/complications.
- Audit first-pass success ≥ 80 % in routine cases.
- Disinfect probe between patients; use single-use sterile cover if scanning after skin prep.
3 Aims
1. Identify the Correct Level
- Paramedian sagittal oblique view
2. Identify the Midline
- Transverse view over spinous processes M-mode for midline
3. Identify the Intrathecal Depth
- Transverse view between spinous processes
- Anterior complex = dura
- Articular process = depth to epidural space
Paramedian Sagittal Oblique view
Anterior complex = dura M-mode: correctly identifies space
Ultrasound for Lumbar Spinal and Epidural Anaesthesia: Current Evidence
Accurate Localisation of the Intervertebral Level
- Palpation versus ultrasound (US)–Agreement between surface landmarks and US is poor (14–64 %).
- Modern prospective studies that used fluoroscopy or MRI as the reference confirm that pre-procedural US locates the correct space in > 90 % of adults after a short learning phase (≈ 10–15 scans).
- Palpation misidentifies the space by ≥ 2 levels in one-third of obese obstetric patients; US reduces this to < 5 %
Prediction of Skin-to-epidural / Intrathecal Depth
- Linear correlation coefficient r ≥ 0.9 between US-measured depth and actual needle depth; mean absolute error 2–5 mm.
- Compression error is minimised by light transducer pressure and measuring to the deep border of the posterior complex in the transverse-interlaminar view
Clinical Efficacy Outcomes (procedural success)
| Setting & operator | Technique compared | Absolute failure reduction | First-pass success gain | Notes |
|---|---|---|---|---|
| 300 labour epidurals, consultants | Pre-scan US vs palpation | 6 % → 2 % | +10 % | Faster onset, lower Was pain at 30 min |
| 370 labour epidurals, first-year trainees | Pre-scan US vs palpation | 5.5 % → 1.6 % | +18 % | Vallejo protocol |
| 212 elective hip/knee arthroplasty spinals, mixed BMI | Pre-scan US vs palpation | 9 % → 3 % | +22 % | 2023 SAJAA RCT |
- Network meta-analysis of 26 RCTs (n = 3 240) shows 49–79 % relative reduction in composite procedural failure with US guidance compared with palpation alone.
Technical Performance
- Punctures & needle passes–Mean reduction 0.7–1.2 passes; more pronounced in obesity, scoliosis and after lumbar surgery
- Time to establish block–30–90 s shorter once operators have performed ≥ 20 US-assisted cases.
- Number-needed-to-scan (NNS) to avoid one traumatic or bloody tap ≈ 11 in high-BMI obstetric population
Safety Outcomes
- Accidental dural puncture–Pooled risk ratio 0.37.
- Post-dural puncture headache–Absolute risk reduction 1.8 %.
- Vascular puncture & paraesthesia–Significantly less frequent with US owing to fewer passes.
- No signal of increased infection when aseptic probe covers are used for real-time guidance.
Special Populations and South-African Data
- Obesity (BMI ≥ 35 kg m⁻²)–SAJAA 2022 study demonstrated halving of attempts (median 2 → 1) and higher patient satisfaction (90 % vs 64 %).
- Spinal deformity / instrumentation–Pre-scan US improves first-pass success to 65–75 % v 25–40 % with landmarks.
- Paediatrics–High-frequency linear probe reliably visualises dura; depth prediction error < 1 mm in infants.
Operator Learning Curve & Governance
- Competence benchmark: ≥ 20 supervised scans to reach 80 % first-pass success; regular audit is advised.
- National and SA professional bodies (RCoA 2024, SAJAA regional anaesthesia guidance 2023) now endorse US as best practice in patients with impalpable landmarks or predicted technical difficulty.
Limitations
- Image quality declines with oedema or extensive subcutaneous emphysema.
- Real-time (in-plane) epidural insertion is technically demanding and currently offers no proven clinical advantage over pre-procedural mapping.
- US does not eliminate, but reduces, the need for expert tactile feedback and vigilantly sterile technique.
Links
References:
- Sm, G., Madjdpour, C., & Chin, K. (2016). Ultrasound-guided lumbar central neuraxial block. BJA Education, 16(7), 213-220. https://doi.org/10.1093/bjaed/mkv048
- Kamimura Y, Yamamoto N, Shiroshita A, et al. Comparative efficacy of ultrasound guidance or conventional anatomical landmarks for neuraxial puncture in adult patients: a systematic review and network meta-analysis. Br J Anaesth 2024;132:1097-1111. Available from: https://pubmed.ncbi.nlm.nih.gov/37806932/
- Makino Y, Miyake K, Roche D, et al. Ultrasound guidance versus anatomical landmarks for neuraxial anaesthesia in adults. Cochrane Database Syst Rev 2025;5:CD014964. Available from: https://pubmed.ncbi.nlm.nih.gov/40421607/
- Korda B, Scribante J, Perrie H, Nel D. Ultrasound-assisted versus landmark-based spinal block in obese parturients undergoing emergency Caesarean delivery. South Afr J Anaesth Analg 2022;28(Suppl S2):S7-S8. Available from: https://www.sajaa.co.za/index.php/sajaa/article/view/2781
- Royal College of Anaesthetists. Guidelines for the Provision of Regional Anaesthesia Services 2024. Available from: https://www.rcoa.ac.uk/node/22406
- Regional Anaesthesia UK; Royal College of Anaesthetists. Curriculum Assessment Guidance: Neuraxial and Peripheral Ultrasound Skills 2024. Available from: https://www.ra-uk.org/
- American Society of Anesthesiologists Committee on Obstetric Anaesthesia. Statement on Neuraxial Analgesia or Anaesthesia in Obstetrics 2023. Available from: https://www.asahq.org/standards-and-practice-parameters/statement-on-neuraxial-anesthesia-in-obstetrics
- American Society of Anesthesiologists. Statement on Neurologic Complications of Neuraxial Analgesia and Anaesthesia in Obstetrics 2023. Available from: https://www.asahq.org/standards-and-practice-parameters/statement-on-neurologic-complications-of-neuraxial-analgesia-anesthesia-in-obstetrics
- Arzola C, Davies S. Ultrasound for lumbar and thoracic neuraxial anaesthesia: current evidence and clinical applications. Curr Opin Anaesthesiol 2022;35:580-586.
- Chin KJ, Karmakar MK. Ultrasonography of the lumbar spine for neuraxial and perineuraxial anaesthesia: anatomy, technique and best evidence. Anesthesiology 2021;134:946-967.
- Miller RD, Cohen NH, Eriksson LI, et al., eds. Miller’s Anaesthesia. 10th ed. Philadelphia: Elsevier; 2023. Chapter 52.
- Kamimura Y, Yamamoto N, Shiroshita A, et al. Ultrasound guidance versus anatomical landmarks for neuraxial puncture in adults: network meta-analysis. Br J Anaesth 2024;132:1097-1111.
- Makino Y, Miyake K, Roche D, et al. Ultrasound guidance for neuraxial anaesthesia in adults. Cochrane Database Syst Rev 2025;5:CD014964.
- Korda B, Scribante J, Perrie H, Nel D. Pre-procedural ultrasound versus landmark technique for spinal anaesthesia in obese parturients: a randomised trial. South Afr J Anaesth Analg 2022;28 (S2):S7-S12.
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “009991c9-7b32-4a49-8e57-51dab974a169”



