{}
Who Can Make the Decisions
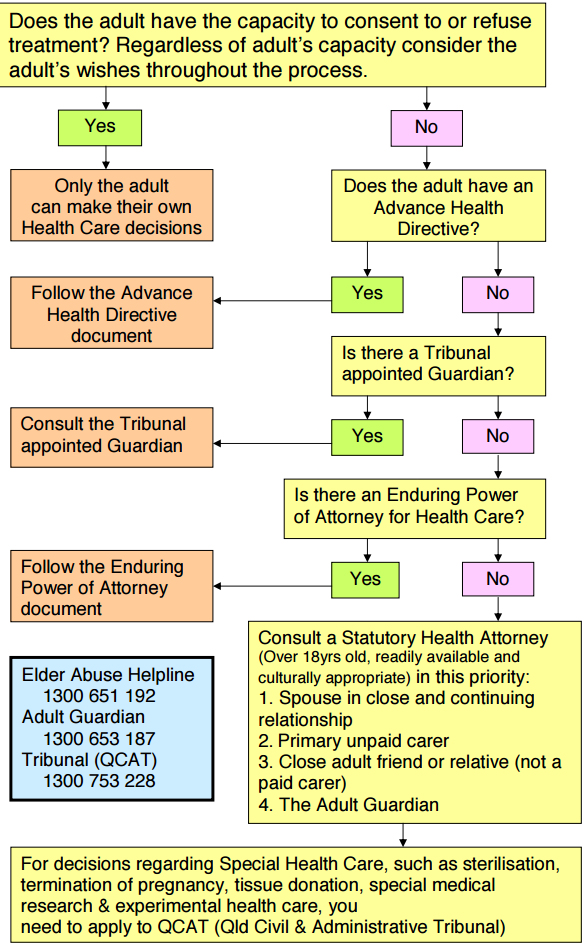
Impaired Capacity–Consent, Urgent Care & Surrogate Decision-making
Assessing Decision-making Capacity
| 4-Step Test (HPCSA Booklet 9, 2021; National Health Act §7) | Practical prompt |
|---|---|
| Understand relevant information | “Tell me in your own words what the surgery is for.” |
| Retain that information long enough to decide | Re-check after 5 min; watch for delirium. |
| Weigh risks v benefits in line with values | “What matters most to you if things go wrong?” |
| Communicate a choice | Any reliable method (speech, writing, blink, AAC device). |
- Presume capacity unless evidence to the contrary; capacity is decision and time-specific and can fluctuate.
Legal Framework (SA)
| Instrument | Key provisions for incapacitated adults |
|---|---|
| National Health Act 61/2003 §7 | Consent must be obtained from authorised “user” or substitute; emergency life-saving treatment may proceed without consent if delay risks death/irreversible harm. |
| HPCSA Booklet 9–Informed Consent (2021) | Sets ethical duty to involve patients “as far as possible”, record capacity assessment, and consult surrogate hierarchy. |
| Mental Health Care Act 17/2002 | Governs patients with severe psychiatric illness–use appointed curator/administrator; urgent care allowed if necessary to prevent harm. |
| Common-law Living Will / Advance Directive | Not yet statute-based but accepted in practice; weighty ethical authority if clearly applicable and not revoked. |
Surrogate Consent Hierarchy (National Health Act §7(1)(d))
- Court-appointed curator / mandatory power of attorney
- Spouse or life-partner
- Parent
- Grandparent
- Adult child
- Adult sibling
- If none available → treating clinicians decide in the patient’s best interests
Best-Interests Checklist
- Clinical effectiveness and expected benefit.
- Known values, cultural or religious beliefs, prior verbal statements.
- Least-restrictive alternative (maintain autonomy where possible).
- Balance of burdens (pain, loss of dignity) v benefits.
- Resource implications (justice)–but never sole criterion.
- Multidiscplinary discussion; document reasoning.
Urgent or Emergency Treatment Pathway
| Scenario | Action | Authority |
|---|---|---|
| Valid advance directive exists | Follow directive unless obviously revoked/irrelevant. | Common law; HPCSA Bk 9 §10 |
| No directive; surrogate reachable | Obtain verbal consent; two-clinician witness if phone. | NHA §7(1)(d) |
| Life-threatening emergency; no surrogate available | Proceed with necessary treatment to prevent death or serious harm; note NHA basis. | NHA §7(1)(e) |
| Doubt whether treatment is in best interests | Phone hospital medical-services manager or ethics on-call (GSH policy) and document. | Institutional SOP |
Practical Documentation
- Capacity assessment: time, persons present, responses to 4 questions.
- Surrogate details: name, relationship, contact number, summary of discussion.
- Treatment decision & rationale (esp. best-interests balancing).
- If emergency: “Treatment commenced under NHA 61/2003 §7(1)(e)–emergency to avert imminent death.”
- File copy of any advance directive or photograph on EMR.
Special Groups & Notes
| Group | Nuance |
|---|---|
| Minors (< 18 yr) | Use Children’s Act 38/2005–≥ 12 yr & mature may consent to medical (not surgical) care; otherwise parent/guardian. |
| Research participation | Requires NHREC-registered REC approval + surrogate consent + patient assent where possible. |
| Mental-health users | Emergency psychiatric treatment governed by Mental Health Care Act; capacity can still be present for physical decisions. |
| Refusal of blood by JW surrogate | If clearly competent previously and directive explicit, respect refusal even in emergency. |
Links
References:
- White, S. and Baldwin, T. (2006). The mental capacity act 2005–implications for anaesthesia and critical care. Anaesthesia, 61(4), 381-389. https://doi.org/10.1111/j.1365-2044.2006.04533.x
- Health Professions Council of South Africa. Guidelines on Informed Consent (Booklet 9). 2021.
- Republic of South Africa. National Health Act 61 of 2003, §7.
- Mental Health Care Act 17 of 2002.
- Medical Protection Society. Living wills and advance directives in South Africa (Factsheet, 2024). medicalprotection.org
- Mpedi G. What doctors should know when working with surrogate decision-makers. SAMJ 2023;113:1364-7. samajournals.co.za
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “46f6576a-3555-42c2-a7a3-7af822074986”



