{}
Summary of Cystic Fibrosis and Anaesthesia
Pathogenesis
Cystic fibrosis is caused by a mutation in the Cystic Fibrosis Transmembrane Regulator (CFTR) gene on chromosome 7. This mutation leads to the dysfunction of the CFTR protein, a transmembrane chloride ion channel found in exocrine tissue, resulting in impaired chloride ion transport.
Mutation of CFTR Gene
- Gene: CFTR gene on chromosome 7
- Effect: Dysfunction of CFTR protein, leading to defective chloride ion transport
Effects on Sweat Glands
- Normal Function: Reabsorption of chloride ions (Cl⁻) by CFTR proteins
- With Mutation: Decreased reabsorption, increased Cl⁻ secretion in sweat
- Outcome: Elevated sweat chloride concentration
Effects on Epithelial Tissue
- Function: CFTR proteins facilitate Cl⁻ diffusion into secretions
- With Mutation:
- Reduced Cl⁻ diffusion into peri-ciliary fluid, altering water composition
- Decreased mucociliary clearance
- Outcome: Accumulation of secretions, obstructing secretory passages
Specific Organ Systems
Lower Respiratory Tract
- Symptoms: Chronic productive cough
- Signs:
- Lung hyperinflation (on x-ray)
- Abnormal pulmonary function tests
- Complications:
- Retained secretions leading to bacterial proliferation, airway infection, and inflammation
- Chronic bronchitis and bronchiectasis (primary cause of death in CF)
Upper Respiratory Tract
- Condition: Chronic sinusitis
- Signs: Nasal polyps
- Cause: Retained secretions in sinuses, leading to bacterial proliferation
Pancreas
- Condition: Pancreatic insufficiency
- Mechanism: Pancreas cannot secrete digestive enzymes, leading to degradation of pancreatic tissue
- Complications:
- Fat and protein malabsorption causing failure to thrive
- Decreased absorption of fat-soluble vitamins (e.g., Vitamin D) causing osteoporosis
- Inflammation leading to scarring, fatty infiltration, and islet cell destruction, causing Type II Diabetes Mellitus
Gastrointestinal Tract
- Symptoms: Decreased intestinal motility
- Complications:
- Distal ileal obstruction syndrome (DIOS) in children/adults
- Meconium ileus in newborns
- Prolonged neonatal jaundice due to retained meconium and increased bilirubin reabsorption
Biliary Tree
- Complications: Delayed bile passage causing inflammatory hepatic response, cirrhosis, and portal hypertension
Was Deferens
- Effect in Utero: Degeneration of was deferens and Wolffian ducts
- Outcome: Infertility in males
Additional Notes
- Inheritance Pattern: Autosomal recessive
- CFTR Gene Mutations: Over 1700 identified, with ΔF508 mutation in ~67% of Caucasians
- Diagnosis: Based on increased sweat chloride concentration, CFTR mutations, and symptoms affecting ≥1 organ system
Manifestations of Cystic Fibrosis
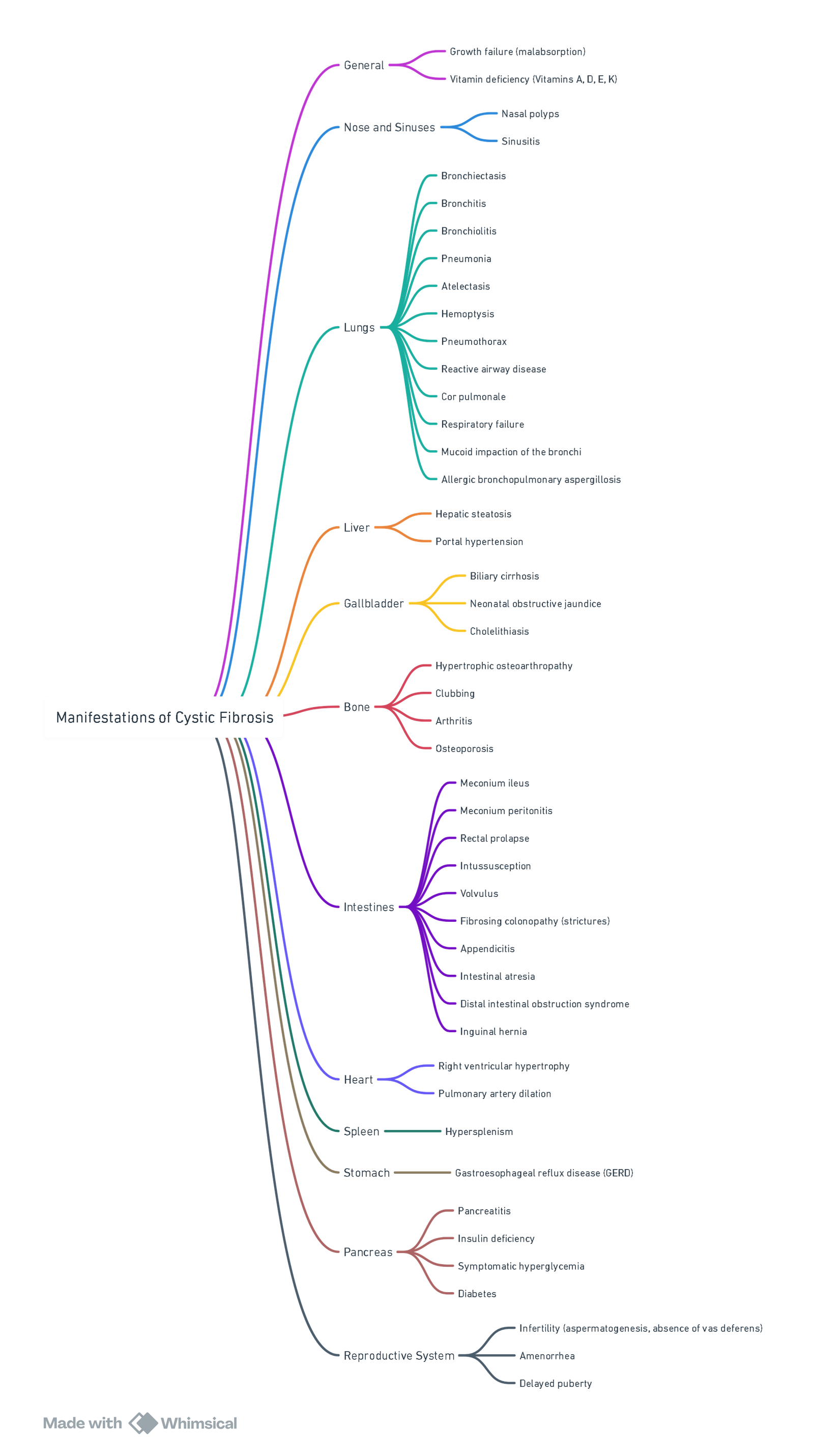
View or edit this diagram in Whimsical.
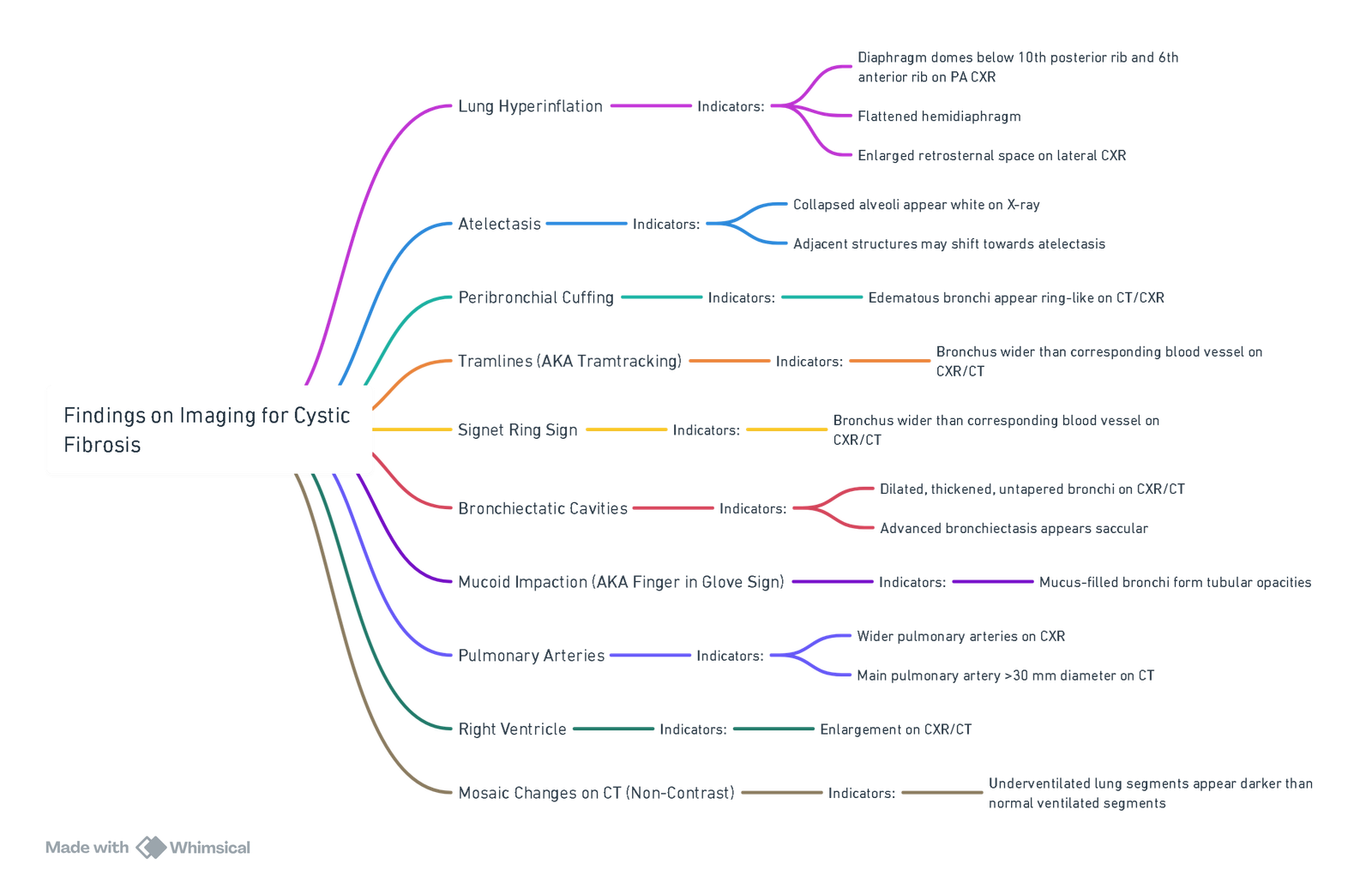
Findings on Chest X-Ray and CT Scan
CXR and CT findings in Cystic fibrosis
Pathophysiology
- CFTR Mutation: Causes abnormal transmembrane Cl⁻ transport in exocrine tissue, resulting in viscous secretions
Mechanism
Early Life
- Bronchial Secretion Accumulation: From birth, secretions accumulate in bronchial lumen, delaying mucociliary clearance
- Obstruction: Mucus plugs obstruct bronchial lumen, trapping air in lungs
Progression
- Lung Hyperinflation:
- Diaphragm domes below 10th posterior rib and 6th anterior rib on PA CXR
- Flattened hemidiaphragm, enlarged retrosternal space on lateral CXR
- Collapsed alveoli appear more solid and radiodense
- Adjacent structures may shift towards atelectasis on CXR
- Air Trapping: Pulmonary capillaries absorb gases in alveoli distal to obstruction, leading to alveolar collapse (Atelectasis)
Imaging
View or edit this diagram in Whimsical.
Clinical Findings
Inflammatory Response
- Early Years: Retained bronchial secretions serve as nidus for recurrent bacterial colonization and infection
- Late Findings: Secretion accumulation blocks inhaled air to affected lung segments, causing chronic hypoxia
- Inflammatory Response: Leads to bronchial and peribronchial destruction
- Fluid Leakage: Into bronchial walls and peribronchial regions
- Destruction of Elastic Components: Of bronchi by inflammatory cytokines
- Accumulation of Inflammatory Exudate: In bronchi
Hypoxia and Pulmonary Hypertension
- Hypoxia: Induces pulmonary capillary vasoconstriction
- Pulmonary Artery Hypertension: Blood backs up in pulmonary arteries, causing right ventricular dilation
- Blood Dilation: Of pulmonary arteries
- Underventilated Lung Segments: Appear as lower intensity on imaging
Imaging Indicators
- Collapsed Alveoli: Appear white on X-ray
- Peribronchial Cuffing: Edematous bronchi appear ring-like
- Tramlines: Bronchus wider than corresponding blood vessel
- Signet Ring Sign: Bronchus wider than corresponding blood vessel
- Bronchiectatic Cavities: Dilated, thickened, untapered bronchi
- Mucoid Impaction: Mucus-filled bronchi form tubular opacities
- Pulmonary Arteries: Appear wider on X-ray
- Right Ventricle Enlargement: On imaging
- Mosaic Changes
Summary
- CFTR Mutation: Leads to abnormal transmembrane Cl⁻ transport and viscous secretions
- Secretions: Accumulate, obstruct, and lead to lung hyperinflation and atelectasis
- Inflammatory Response: Causes bronchial destruction and chronic hypoxia
- Pulmonary Hypertension: Results from capillary vasoconstriction and blood backing up in pulmonary arteries
- Key Imaging Findings: Atelectasis, peribronchial cuffing, tramlines, signet ring sign, bronchiectatic cavities, mucoid impaction, pulmonary artery widening, right ventricle enlargement, and mosaic changes on CT
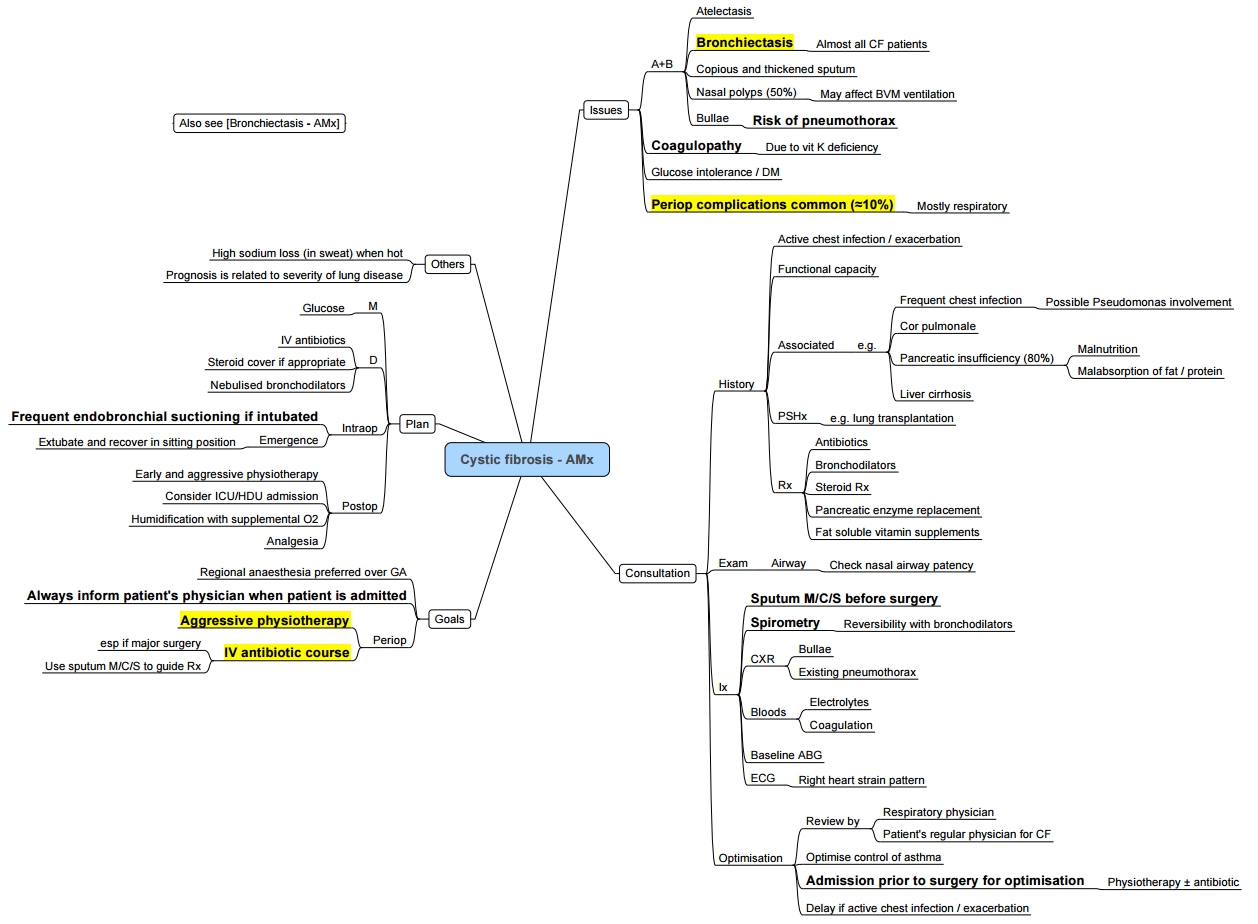
Cystic Fibrosis and Anaesthesia
Cystic fibrosis (CF) is characterized by thick secretions and ciliary dysfunction involving the respiratory and gastrointestinal systems, resulting in malabsorption syndromes, pneumonia, wheezing, and bronchiectasis.
Considerations
- High risk for perioperative pulmonary complications
- Pathophysiologic Sequelae:
- Pulmonary: Mucous plugging, chronic pneumonia, bronchiectasis, hemoptysis, bronchospasm, pneumothorax, mixed restrictive & obstructive lung physiology, bullous disease, hypoxemia/hypercarbia
- Cardiovascular: Pulmonary hypertension, cor pulmonale
- Extra-pulmonary Disease:
- Anemia of chronic disease
- GERD, sinusitis
- Hepatic: Abnormal transaminases, cirrhosis, portal hypertension, coagulopathy
- Pancreatic insufficiency & diabetes
- Chronic malnutrition, cachexia, deconditioning
- CF-related Medications: Oxygen, bronchodilators, mucolytics, antibiotics, steroids, insulin, pancreatic enzymes
Goals & Conflicts
- Preoperative optimization in collaboration with respiratory medicine
- Avoidance of general anaesthesia (GA) if feasible
- Intraoperative Management Principles:
- Lung protective ventilation
- Aggressive pulmonary toilet, bronchodilation, hydration
- Avoid prolonged ventilation
- Multimodal analgesia with limited sedating analgesics
- Avoid exacerbation of pulmonary hypertension
- Postoperative high acuity setting with aggressive respiratory therapy
- Verify normal coagulation parameters prior to neuraxial/regional anaesthesia
Preoperative Management
- Intense physiotherapy and use of BiPAP machine (if available)
- Nebulize drugs as late as possible
- CXR, ABG, and spirometry
- FBC, U+E, LFTs, coagulation, BSL
- ECG, Echo (assess for cor pulmonale), raised JVP, enlarged liver, peripheral oedema
- Check for cyanosis and assess saturations
- Signs of liver disease
- Previous surgeries (transplants, ERCP, etc.)
Intraoperative Management
- Use arterial line (A-line)
- Avoid nasal intubation (due to polyps)
- Short-acting agents and opioid-sparing techniques to minimize respiratory depression
- Caution with muscle relaxation (some patients rely on muscle tone for airway patency)
- Regional anaesthesia (consider altered coagulation due to malabsorption)
- Careful positioning (cachectic patients)
- Aim for early extubation (trial extubation even if predictors of postoperative ventilation are present)
- Postoperative care in PACU/ICU
Predictors of Postoperative Ventilation
- FEV1 <61% predicted (<1L in adults)
- PaO2 <9.3kPa (RA) (70mmhg)
- PaCO2 >6.6kPa (50mmhg)
Pregnancy
- Very high-risk patient with increased risk of low birth weight babies and pre-term delivery
Vaginal Delivery
- Ensure monitored setting, consider invasive monitoring if significant cardiorespiratory dysfunction
- Epidural is an excellent choice to reduce hyperventilation and stress, but titrate carefully to T10 to prevent respiratory muscle weakness
Cesarean Delivery
- Epidural preferred with careful titration to avoid high block
- GA is acceptable but remember goals:
- Prevent perioperative bronchospasm
- Frequent suctioning for pulmonary toilet
- Appropriate ventilatory settings to avoid air trapping/pneumothorax
- Post-op monitoring in HAU/ICU, chest physiotherapy, pulmonary optimization
- Use NIPPV to treat respiratory failure
Links
- Post op pulmonary complications
- Lung resection
- Bronchiectasis
- Tracheal surgery
- Thoracic pre-op assessment
References:
- Fitzgerald, M. and Ryan, D. (2011). Cystic fibrosis and anaesthesia. Continuing Education in Anaesthesia Critical Care &Amp; Pain, 11(6), 204-209. https://doi.org/10.1093/bjaceaccp/mkr038The
- Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “91563247-46fd-45aa-b0ab-3862b8aafb3f”



