- What is PPC (Post Op Pulmonary complications)
- Risk Factors for Postoperative Pulmonary Complications
- Surgical Factors Contributing to Postoperative Pulmonary Complications (PPCs)
- Patient Factors Contributing to PPCs
- ASA Classification and the Rate of PPCs (Postoperative Pulmonary Complications)
- Anaesthetic Factors
- Pathophysiology of General Anaesthesia
- Atelectasis
- Postoperative Respiratory Failure (PRF)
- Postoperative ARDS
- Neuromuscular Block and Reversal
- Volatile vs. Intravenous Anaesthesia
- General Anaesthesia (GA) vs. Neuraxial Blockade (NAB)
- Intravascular Volume Management
- Preoperative Measures
- Intraoperative Ventilation
- Perioperative Testing
- Risk Stratification
- Risk Reduction
- Prevention of PCC
- Postoperative Care for Pulmonary Complications (PPCs)
- Links
{}
What is PPC (Post Op Pulmonary complications)
- A condition affecting the respiratory tract that can adversely influence the clinical course of a patient after surgery or a postoperative decrease in functional residual capacity and total lung capacity that results in ventilation-perfusion mismatch and hypoxaemia
- respiratory failure, the need for endotracheal intubation within 48 hours, weaning failure, atelectasis, pneumothorax, pleural effusions, aspiration pneumonitis, pneumonia, bronchospasm, laryngospasm, hypoxia, exacerbation of chronic obstructive pulmonary disease (COPD) as well as upper airway obstruction
- Prevalence: 2.5-5%
Risk Factors for Postoperative Pulmonary Complications
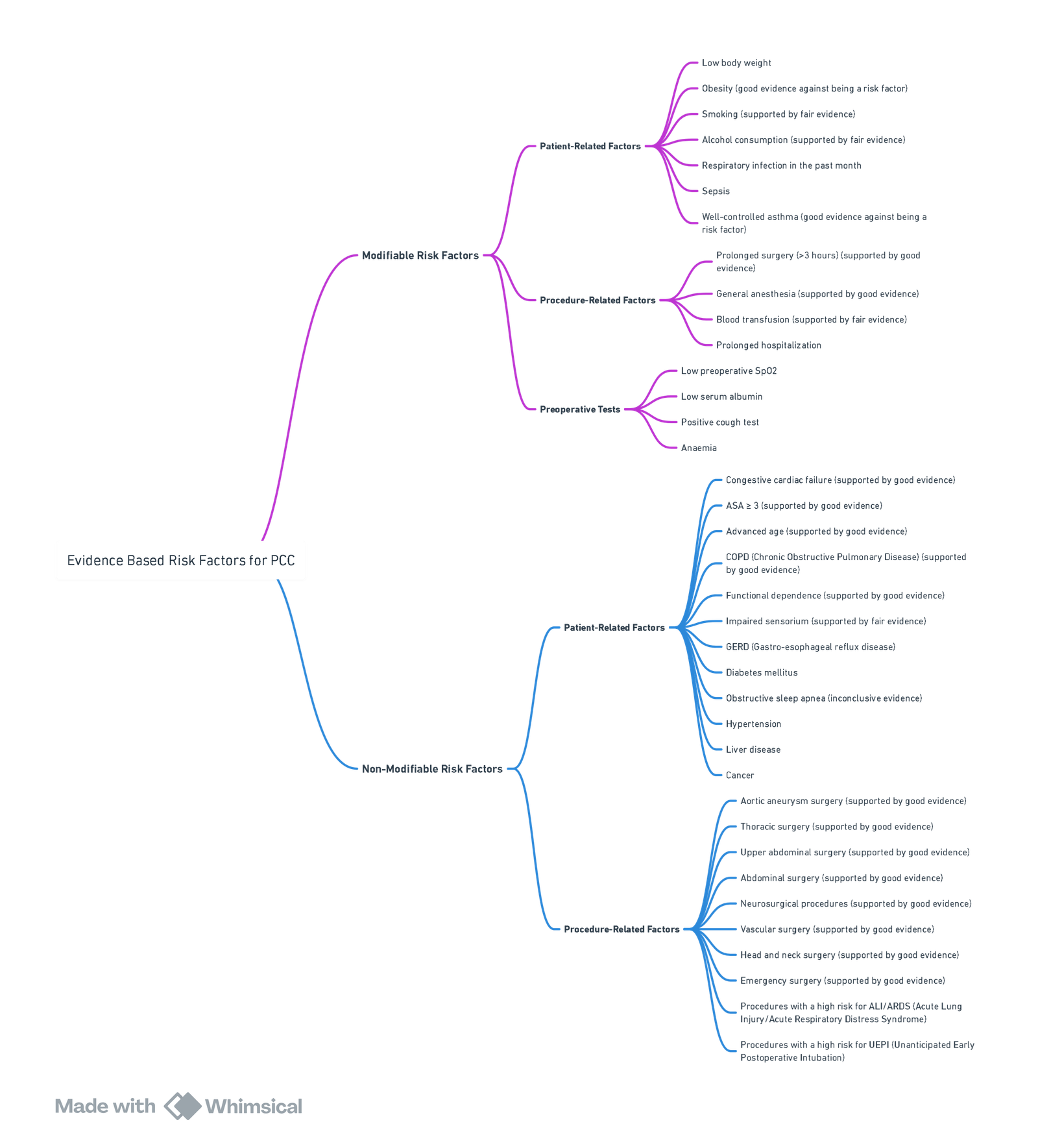
View or edit this diagram in Whimsical.
Surgical Factors Contributing to Postoperative Pulmonary Complications (PPCs)
Surgical Site
- The surgical site is a significant risk factor for PPCs due to inhibition of respiratory muscle function from:
- Incisional pain
- Functional disruption from the surgical incision
- Reflex inhibition of phrenic nerve output from traction on abdominal viscera
- Highest risk of PPCs is associated with aortic, thoracic, and upper abdominal surgeries.
- Emergency surgeries, regardless of site, carry a high risk of PPCs.
Laparoscopic vs. Open Surgery
- Minimally invasive surgical procedures, such as laparoscopic surgery, may reduce the risk of PPCs compared to open surgery.
Duration of Surgery
- Procedures lasting more than 3 hours are associated with a higher risk of PPCs.
Nasogastric Decompression
- Routine use of nasogastric tubes post-abdominal surgery is associated with an increased risk of aspiration and PPCs.
Patient Positioning During Surgery
- Positions such as Trendelenburg, jack-knife, and kidney rest may reduce cardiac output, worsening ventilation/perfusion mismatch.
- Pulmonary vascular congestion, particularly in the supine position, can reduce functional residual capacity (FRC), especially in patients with orthopnea.
- Prolonged surgeries in dependent lung positions (zone 3 or 4) are prone to fluid accumulation, potentially leading to pulmonary edema and decreased FRC, especially with aggressive fluid administration.
Patient Factors Contributing to PPCs
Age
- Elderly patients have an increased risk of PPCs, even after adjusting for comorbidities.
- Advanced age is associated with:
- Decreased respiratory muscle strength
- Decreased chest wall compliance
- Decreased elastic recoil of lung parenchyma
- Decreased alveolar surface area
- PPC rates dramatically increase in patients over 80 years old.
Asthma
- Well-controlled asthma is not a significant risk factor for PPCs.
- Patients with peak flow within 80% of predicted or personal best have a similar risk to non-asthmatics.
- Short-acting bronchodilators, anticholinergics, and anxiolytics may help reduce bronchial tone.
- Short-acting corticosteroids may prevent PPCs if clinically indicated, without strong evidence of impairing wound healing or increasing infection rates.
Chronic Lung Disease
- COPD is an important risk factor for PPCs.
- Restrictive lung pathologies are not significantly identified as risks.
- COPD patients can be optimized with medication and pulmonary rehabilitation.
- Daily use of bronchodilators benefits COPD patients undergoing surgery.
- Inhaled ipratropium bromide (or tiotropium bromide) should be used daily in symptomatic COPD patients.
- B2 agonists should be used as needed for symptoms and wheezing.
- Corticosteroids should be used in patients with persistent wheeze or effort intolerance despite bronchodilator use.
- Empiric antibiotics are not recommended unless there is an acute exacerbation, delaying non-urgent surgery until symptoms resolve and for 4 weeks thereafter.
Obstructive Sleep Apnea (OSA)
- OSA increases the risk of PPCs, but postoperative respiratory care such as noninvasive ventilation devices can mitigate this risk.
- Initiating nCPAP preoperatively, ideally for a week, can reduce postoperative respiratory failure.
Congestive Cardiac Failure (CCF)
- CCF is a significant risk factor for PPCs.
Smoking
- Current smokers have a higher incidence of 30-day postoperative respiratory events compared to former smokers.
- Cessation of smoking for more than 1 year prior to elective surgery reduces PPCs.
- The exact duration of abstinence needed to reduce PPCs is unclear.
- Smokers have a higher incidence and severity of coughing during emergence from anesthesia.
- Sevoflurane anesthesia in smokers has a high probability of coughing at extubation, which is crucial in surgeries where coughing is undesirable, such as cervical spine surgery.
Mechanisms of Smoking-Induced Pulmonary Damage
a. Pre-existing Tobacco-Induced Damage: Tobacco smoking causes widespread damage to organ systems, particularly the lungs.
b. Impaired Immune Function: Smoking weakens the immune system, making the body more susceptible to infections.
c. Small Airway Narrowing: Smoking increases the closing volume of small airways, leading to obstructed airflow.
d. Reduced Pulmonary Capacity: Smoking decreases lung function and pulmonary capacity.
e. Increased Secretion of Hyperviscous Mucus: Smoking causes excessive mucus production, which is thicker and more viscous.
f. Reduced Ciliary Function: Smoking impairs the function of cilia, reducing the clearance of mucus and debris from the airways.
Smoking Cessation and Its Benefits
- Optimal Cessation Period: At least 4-8 weeks before surgery.
- Patients who quit smoking >8 weeks before surgery have PPC rates comparable to non-smokers.
- Smokers with normal spirometry have a 4% risk of PPCs, while heavy smokers have up to a 43% risk.
Physiological Recovery Post-Smoking Cessation:
- 12-48 hours: Reduction in carboxyhaemoglobin levels, shifting the oxyhaemoglobin dissociation curve to the right, increasing oxygen availability.
- 2-3 days: Recovery of ciliary function, with an increase in sputum production.
- 2 weeks: Reduction in airway reactivity.
- 6 weeks: Normalization of sputum volume.
- 3 months: Near-normal tracheobronchial clearance.
- 6 months: Improvement in small airway narrowing.
Alcohol Consumption and Its Impact
- Risk Increase: Preoperative alcohol consumption is associated with a 1.80-fold increase in pulmonary complications, infections, wound complications, prolonged hospital stays, and ICU admissions.
- High alcohol consumption (>60g/day) increases postoperative mortality risk.
- Subgroups with high alcohol exposure report higher relative risks of PPCs.
Pathophysiological Mechanisms:
- Reduced immunity and an increased stress response to surgery.
Recommendation:
- Avoid alcohol for at least 2 weeks before surgery to reduce complications and avoid short-term abstinence syndrome.
Nutritional Status and Its Impact
Obesity
- Not a significant risk factor for PPCs generally but increases risk in specific surgeries (e.g., uvulopalatopharyngoplasty, thoracic surgery).
- Comorbidities associated with obesity increase PPC risk.
- Severe obesity (BMI >40 kg/m²) is linked to higher rates of pneumonia, respiratory failure, and unplanned tracheal intubation.
Malnutrition
- Increases the risk of PPCs.
- Weight loss >10% in the past 6 months is a significant risk factor.
Respiratory Infections
-
Upper Respiratory Tract Infection (URTI):
- Increases bronchial reactivity and risk of laryngospasm, bronchospasm, and perioperative hypoxemia.
- Elective surgery should be delayed for 1 month after URTI resolution.
-
Lower Respiratory Tract Infection (LRTI):
- Considered a risk factor for PPCs, especially with fever and antibiotic requirement.
Functional Dependence
- Total Dependence: Associated with an OR of 2.51 for PPCs (95% CI: 1.99-3.15).
- Partial Dependence: Associated with an OR of 1.65 for PPCs.
ASA Classification and the Rate of PPCs (Postoperative Pulmonary Complications)
| ASA Class | Class Definition | Rate of PPCs by Class (%) |
|---|---|---|
| I | Normally healthy | 1.2 |
| II | Mild systemic disease | 5.4 |
| III | Systemic disease not incapacitating | 11.4 |
| IV | Incapacitating disease that is a constant threat to life | 10.9 |
| V | Moribund and not expected to survive 24 hours | N/A |
Anaesthetic Factors
Pathophysiology of General Anaesthesia
- Muscle Tone and Thoracic Dimensions: General anaesthesia reduces muscle tone, decreasing thoracic diameters, lung volumes, and airway dimensions, resulting in a decrease in functional residual capacity (FRC), potentially falling below closing capacity in diseased states.
- FRC Reduction: Even in healthy lungs, induction of general anaesthesia decreases FRC by up to 20%, occurring immediately after intubation and often accompanied by airway closure and atelectasis, leading to abnormal gas exchange with ventilation-perfusion mismatch and shunt.
- Diaphragmatic Dysfunction: General anaesthesia affects diaphragmatic movement, increasing ventilation of poorly perfused superior lung portions and decreasing ventilation of well-perfused dependent areas, causing increased shunt and dead space.
- Spontaneous Breathing and Hypoventilation: Patients who breathe spontaneously under general anaesthesia tend to hypoventilate with reduced tidal volume (VT), due to decreased compliance, increased airway resistance, and presence of airway devices. Opiates and anaesthetics further reduce the ventilatory response to hypoxaemia and hypercarbia, persisting into the postoperative period.
- Biological Effects on the Respiratory System: General anaesthesia inhibits alveolar macrophage activity, decreases surfactant production, enhances pulmonary vasculature response to neurohumoral mediators, and tracheal instrumentation alters mucociliary function, increasing resistance and work of breathing.
Atelectasis
- Occurrence and Persistence: Atelectasis occurs in up to 90% of perioperative patients, typically self-limiting but may persist for more than two days post-abdominal surgery. It is associated with decreased pulmonary compliance, worsened ventilation-perfusion mismatch, impaired gas exchange, and hypoxaemia.
- Mechanisms:
- Chest wall deformation due to loss of coordinated respiratory muscle activity
- Absence of inspiratory muscle tone during positive pressure ventilation
- Absorption atelectasis behind closed airways
- Compression of lung tissue
- Loss or impaired function of surfactant
Prevention of Atelectasis
- PEEP: Positive end-expiratory pressure counteracts alveolar collapse and increases FRC. While PEEP is effective intraoperatively, evidence for its impact on postoperative outcomes is limited.
- Oxygen Management: High inspired oxygen concentration can cause absorption atelectasis. Lowering FiO2 from 1.0 to 0.8 may reduce atelectasis while maintaining a margin of safety. Preoxygenation using CPAP reduces atelectasis. Avoid high FiO2 during maintenance and use low FiO2 with CPAP before extubation.
Postoperative Respiratory Failure (PRF)
- Determinants: PRF is influenced by respiratory muscle function, hampered by residual effects of anaesthetics, opiates, sedatives, and residual neuromuscular blockade, compounded by comorbidities like COPD, smoking, obesity, and OSA.
Postoperative ARDS
- Classification and Incidence: Classified by the Berlin criteria: mild (PaO2/FiO2 200-300 mmHg), moderate (100-200 mmHg), severe (<100 mmHg). Incidence ranges from 0.2% in general surgical patients to 10.2% in high-risk surgeries, with mortality ranging from 17% (mild) to 58% (severe).
Neuromuscular Block and Reversal
- Residual Blockade: A significant risk factor for PPCs, impairing breathing and airway reflexes. Use of short-acting neuromuscular blocking agents, peripheral nerve stimulators, and cholinesterase inhibitors like neostigmine reduces this risk. Pancuronium, a long-acting agent, is particularly associated with higher PPC rates and residual blockade effects lasting up to 7 days.
Volatile vs. Intravenous Anaesthesia
- Cytokine Release: Volatile anaesthetics like sevoflurane and desflurane reduce cytokine release during one-lung ventilation compared to propofol, though clinical significance remains unclear.
General Anaesthesia (GA) vs. Neuraxial Blockade (NAB)
- PPCs in COPD: General anaesthesia is associated with more PPCs in COPD patients compared to NAB. However, recent studies show no mortality benefit for regional over general anaesthesia. In severe COPD, regional anaesthesia’s adverse effects may outweigh benefits. In mild/moderate COPD, spinal anaesthesia may be preferable.
Intravascular Volume Management
- Positive Fluid Balance: A positive fluid balance of >1.5L is associated with increased risk of postoperative acute lung injury (ALI).
Preoperative Measures
- Inspiratory Muscle Training: Reduces PPCs in cardiac surgery patients.
- Physiotherapy and Pulmonary Rehabilitation: Improves exercise capacity and pulmonary function in patients undergoing thoracotomy and lung resection, with uncertain impact on PPC reduction.
Intraoperative Ventilation
- Lung-Protective Strategy: Use of low tidal volume (VT) 6-8 mL/kg predicted body weight (PBW), moderate PEEP (5-8 cmH2O), and periodic recruitment manoeuvres reduces PPCs and extrapulmonary complications compared to higher VT without PEEP or recruitment.
Perioperative Testing
Blood
- Albumin: Low serum albumin (<35 g/L) is a predictor of PPCs and perioperative mortality.
- Haemoglobin (HB): Both low haemoglobin (<10 g/dL) and intraoperative transfusion are linked to PPCs. Preoperative transfusions increase PPC risk, especially with >4 units.
Glucose
- Diabetes Mellitus: Modest impact as a risk factor for PPCs.
Other Tests
- Saturation (SO2): Preoperative peripheral saturation predicts unforeseen hypoxaemic events.
- Cough Test: Early warning for COPD exacerbation or infection. Positive if the patient coughs more than once.
- Spirometry and Chest X-Rays: Not routinely recommended but may be useful in high-risk patients, particularly those with pulmonary disease.
Risk Stratification
ARISCAT (A Postoperative Pulmonary Complications Risk Score)
- Risk Levels:
- Low risk: <26 points
- Moderate risk: 26-44 points
- High risk: >45 points
The ARISCAT Score for the Prediction of a Composite of PPCs (Postoperative Pulmonary Complications)
| Predictor | Score |
|---|---|
| Age (years) | |
| ≤50 | 0 |
| 51-80 | 3 |
| >80 | 16 |
| Preoperative SpO₂ | |
| ≥96% | 0 |
| 91-95% | 8 |
| ≤90% | 24 |
| Respiratory infection in the last month | 17 |
| Preoperative anaemia (Hb ≤10 g/dL) | 11 |
| Surgical incision | |
| Peripheral | 0 |
| Upper abdominal | 15 |
| Intrathoracic | 24 |
| Duration of surgery (hours) | |
| ≤2 | 0 |
| 2-3 | 16 |
| >3 | 23 |
| Emergency procedure | 8 |
Notes
- Advanced age: >80 years appears to be the cutoff at which the PPC rate dramatically increases (OR 5.6 after 80 years of age).
- Low preoperative arterial oxygen saturation: Breathing room air while supine is the strongest patient-related risk factor for PPC.
- Acute respiratory tract infection within the past month (both upper and lower airways).
SPORC
SPORC 1
Factors Considered
- All five predictors of the previously reported SPORC were considered: ASA physical status ≥ 3; history of chronic pulmonary disease; history of heart failure; emergency surgery; and high-risk surgical services (vascular surgery; transplant surgery; neurosurgery; thoracic surgery; general surgery; and burn surgery)
SPORC Score for Re-intubation Probability
Risk Factors and Scores
- ASA Score ≥ 3: 3 points
- Emergency Procedure: 3 points
- High-Risk Service: 2 points
- Congestive Heart Failure: 2 points
- Chronic Pulmonary Disease: 1 point
Re-intubation Probability
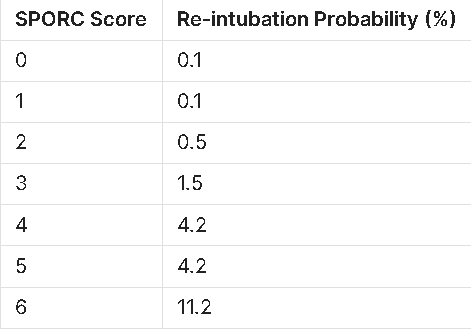
Interpretation
- The SPORC score uses specific risk factors to predict the probability of re-intubation.
- A higher score indicates a higher probability of re-intubation postoperatively.
SPORC2
- A total of 12 predictors were retained in the final model for SPORC-2: five pre-operative variables (ASA physical status ≥ 3; heart failure; chronic pulmonary disease; emergency surgery; and high procedural severity score (32–48 and ≥ 49)
- Seven intra-operative factors (desaturation (SpO2 ≤ 90%) 5 min after tracheal intubation; duration of surgery > 140 min and > 225 min; high median FIO2 (> 0.61); high total noradrenaline equivalent dose (> 0.18 mg); intra-operative transfusion of packed red blood cells; the absence of volatile anaesthetic agents; and lack of lung-protective ventilation patterns).
- The final prediction score reached a maximum score point value of 46 points
Risk Factors for Postoperative Complications: Pre-operative and Intra-operative Variables
Pre-operative Variables
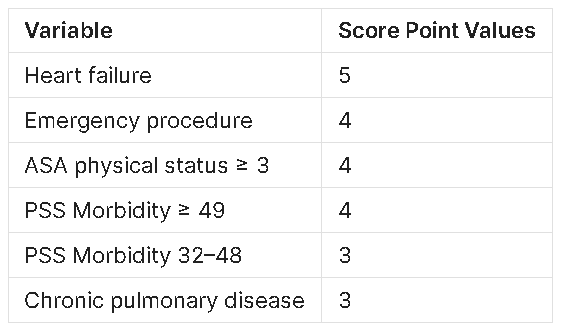
Intra-operative Variables
Interpretation
- Each variable contributes to the overall risk score for postoperative complications.
- Higher scores indicate a greater risk of postoperative complications.
- The scores for each variable should be summed to estimate the patient’s risk profile.
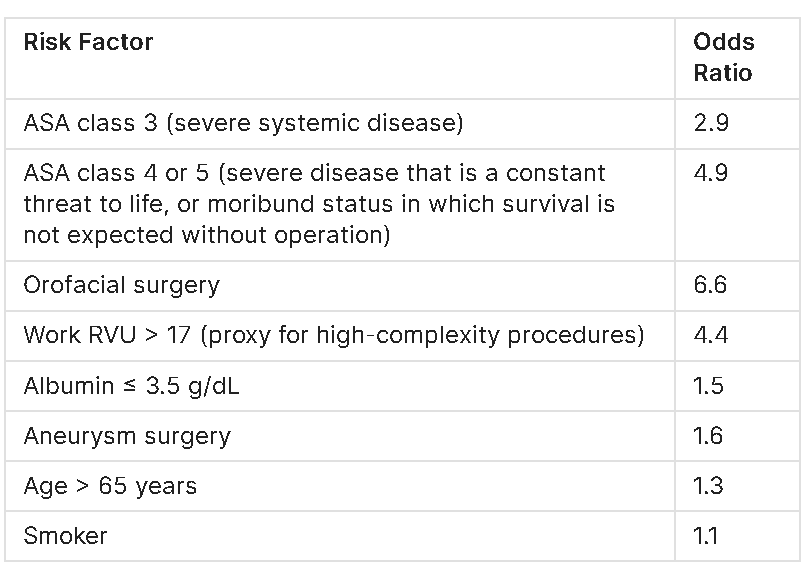
Risk Factors for Postoperative Pulmonary Complications
Odds Ratios for Risk Factors
Risk Reduction
Perioperative Management Algorithm for Reducing Postoperative Pulmonary Complications
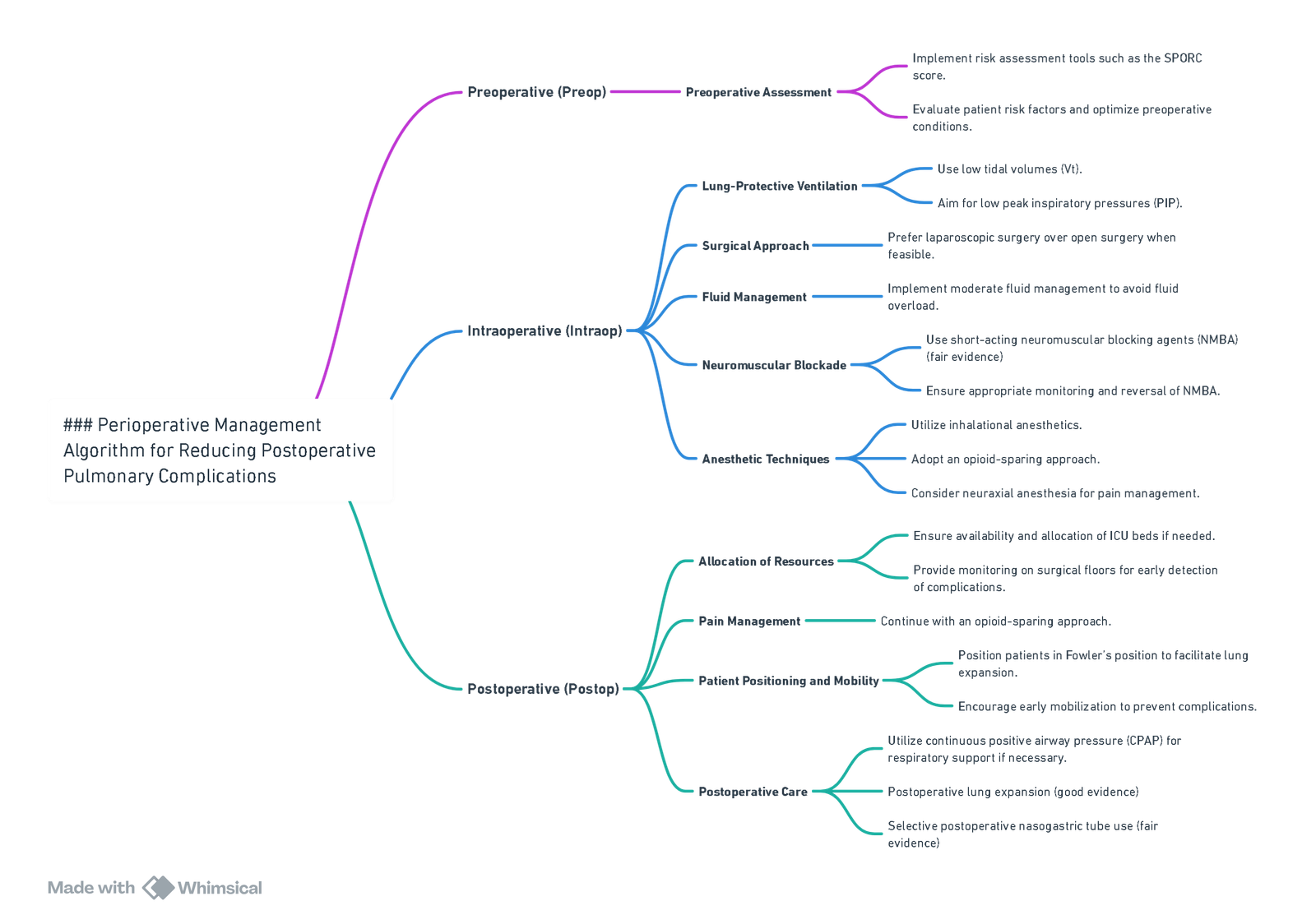
View or edit this diagram in Whimsical.
Prevention of PCC
Preoperative Considerations
- Risk Stratification
- Use tools such as the ARISCAT score to assess postoperative pulmonary complications.
- Multidisciplinary Involvement
- Engage healthcare professionals, particularly for patients with significant cardiopulmonary conditions.
- Preoperative Physiotherapy
- Beneficial for cardiothoracic and high-risk surgical patients.
- Address Modifiable Parameters
- Manage reversible airway diseases with bronchodilators, corticosteroids, and antibiotics if needed.
- Postpone surgery for upper respiratory tract infections (URTI) and lower respiratory tract infections (LRTI).
- Address nutritional deficiencies and optimize preoperative anemia.
- Smoking and Alcohol
- Stop smoking at least 4 weeks prior to surgery (preferably 8 weeks).
- Abstain from alcohol for 2 weeks preoperatively.
Intraoperative Considerations
- Surgery Duration
- Limit to < 3 hours to minimize risk of respiratory complications.
- Minimally Invasive Techniques
- Use laparoscopic or other minimally invasive approaches where feasible.
- Nasogastric Tubes
- Use only when clinically indicated to reduce aspiration risk.
- Preoxygenation
- Use FiO₂ ≥ 0.8, even in low-risk patients.
- CPAP use during preoxygenation
- Airway Management
- Consider supraglottic airway devices for low-risk procedures to minimize airway trauma.
- Oxygen Titration
- Aim for SpO₂ ≥ 92% or PaO₂ > 8 kPa.
- Avoid high intraoperative inspiratory oxygen fractions (optimal mean FiO₂ ~0.31) to reduce oxygen toxicity and postoperative pulmonary complications.
- Neuraxial Techniques
- Use as an adjunct to general anaesthesia to improve respiratory outcomes.
- Prefer neuraxial blockade (e.g., epidural or spinal anaesthesia) where applicable.
- Neuromuscular Blocking Agents
- Avoid long-acting agents and minimize the dose of anaesthetic agents to facilitate faster recovery.
- Avoid intermediate-acting NMBA if possible.
- Use low-dose NMBA with proper neostigmine reversal (≤60 μg/kg after TOF count of 2).
- Opioid sparing techniques
- Neuromuscular Monitoring
- Ensure full recovery from neuromuscular blockade before extubation.
- Monitor for signs of residual neuromuscular blockade (e.g., SpO₂ < 90% with ≥3% drop after extubation).
- Ventilation Strategies
- Use lung-protective ventilation:
- Tidal volumes of 6–8 mL/kg ideal body weight
- PEEP > 5 cmH₂O
- Plateau pressure ≤ 30 cmH₂O
- Recruitment maneuvers followed by PEEP titration may be considered in select cases (e.g., morbid obesity, critical illness).
- Use lung-protective ventilation:
- Fluid Management
- Optimize volume status with goal-directed fluid therapy to prevent pulmonary edema and associated complications.
- Inhalational Anaesthetic Dose
- Limit the dose of inhalational agents, as high doses are associated with increased risk of respiratory failure, pneumonia, and reintubation.
- Extubation
- Use FiO₂ ≥ 0.4 and consider CPAP support if required to prevent hypoxemia.
Postoperative Considerations
- Analgesia
- Use multimodal analgesia to reduce opioid consumption and subsequent respiratory depression.
- Implement opioid-sparing strategies in surgical patients with acute pain.
- Noninvasive Respiratory Support (NRS)
- Consider CPAP in high-risk populations (e.g., bariatric patients) during recovery to reduce oxygen desaturations and apnea-hypopnea index.
- Monitoring on the Surgical Floor
- Ensure appropriate postoperative monitoring (e.g., pulse oximetry) to detect early deterioration and facilitate rescue interventions.
- Physiotherapy and Early Mobilization
- Encourage deep breathing exercises, incentive spirometry, and ambulation to prevent atelectasis and pneumonia.
- In ICU patients, adopt early, goal-directed mobilization strategies using an interprofessional approach and structured algorithms (e.g., SOMS).
- Patient Positioning
- Use upright or Fowler’s positioning (elevated head-of-bed) in at-risk patients to reduce pharyngeal collapsibility and improve oxygenation, especially in OSA and postpartum populations.
- Admission to ICU
- Ensure optimal decision-making regarding ICU versus ward admission postoperatively to reduce complications such as reintubation, pulmonary edema, and pneumonia.
- Avoidance of Reintubation
- Prevent avoidable causes of reintubation in SICU patients by managing modifiable risk factors (e.g., elevated BUN, anemia, muscle weakness).
Postoperative Care for Pulmonary Complications (PPCs)
Postoperative Pain: Regional vs. Systemic
- Regional Anesthesia:
- Decreases pain, improving pulmonary mechanics, coughing, and mobilization.
- May reduce reflex inhibition of respiratory muscles.
- Thoracic epidural analgesia may decrease PPCs, such as pneumonia and postoperative ventilation, although randomized controlled trials have not demonstrated a significant benefit over systemic analgesia.
Physiotherapy
- Techniques include early mobilization, respiratory muscle training, breathing exercises, and neuromuscular electrical stimulation.
- These can reduce radiographic changes, improve gas exchange, reduce postoperative length of stay, and improve quality of life.
- No one technique has been shown to be more effective, although incentive spirometry may be the least labor-intensive.
- There is low-quality evidence for incentive spirometry in preventing PPCs.
- ICOUGH Program:
- An easy and inexpensive program shown to reduce postoperative pneumonia and unplanned intubation.
- Components:
- I: Incentive spirometry
- C: Coughing and deep breathing
- O: Oral care (twice-daily tooth-brushing and mouth-washing)
- U: Understanding (education for patient and family)
- G: Getting out of bed frequently (>3 times a day)
- H: Head of bed elevation
Noninvasive Respiratory Support (NRS)
- Prophylactic Use: Prevent postoperative respiratory failure in at-risk patients.
- Therapeutic Use: Treat respiratory failure when it occurs.
- Effective in:
- Pulmonary edema
- Hypercapnic respiratory failure, especially in COPD exacerbations
- Effective in:
- Contraindications:
- Severe acute respiratory failure with minute ventilation >15 L/min
- Presence of shock
- Base excess more negative than -5 mmol/L
- PaO2/FiO2 <120 mmHg
- Diffuse or patchy infiltrates on chest X-ray
- Impaired ability to clear secretions and swallow
- Intubation Indications:
- If PaO2/FiO2 <175 mmHg after 1-4 hours of NRS treatment, endotracheal intubation should not be delayed.
Monitoring Options
- Pulse Oximetry: Continuous monitoring of oxygen saturation.
- Respiratory Rate: Basic and essential monitoring.
- Additional Options:
- Thoracic Impedance: Measures respiratory rate but can record respiratory effort even with complete airway obstruction.
- Nasal Capnography: Measures exhaled CO2 but may have poor tolerance and be affected by mouth breathing.
- Transcutaneous CO2 Monitoring: Requires complex calibration and frequent probe changes to avoid thermal injury, with delayed detection.
- Acoustic Monitoring: Sensor placed on the neck to monitor respiratory rate.
Links
- Anaesthesia emergencies
- Acute coronary syndrome (ACS)
- Thoracic pre-op assessment
- Post op complications
- Pre-op assessment and investigation
- Spine surgery
- Lung resection
- Scoliosis
References:
- Postoperative pulmonary complications. CT refresher Dr Jenne Piercy 2015
- Miskovic, A. and Lumb, A. B. (2017). Postoperative pulmonary complications. British Journal of Anaesthesia, 118(3), 317-334. https://doi.org/10.1093/bja/aex002
- FRCA Mind Maps. (2024). Retrieved June 5, 2024, from https://www.frcamindmaps.org/
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “b87d5d65-936a-4ce5-ab7d-401123ad6348”



