- Lung Resection
- Types of Pneumonectomy
- Goals
- Incision Types: Pros and Cons
- Preoperative Assessment for Pneumonectomy
- Risk Assessment Summary
- Conduct of Anaesthesia for Lung Resection
{}
Lung Resection
Morbidity and Mortality
-
Postoperative mortality increases with age, possibly due to the right ventricle’s inability to adapt to the increased pulmonary vascular resistance (PVR) following resection. The right-sided pneumonectomy presents a higher mortality risk than left-sided due to:
- Higher pulmonary vascular resistance in the smaller left lung
- Increased incidence of right ventricular failure
- Higher rates of bronchopleural fistula (BPF)
-
Quality of life after pneumonectomy is poorer than after lobectomy or bilobectomy.
Given these concerns, thoracic surgeons reserve pneumonectomy as a last resort, after excluding other surgical options such as sleeve lobectomy or non-anatomical resections. When pneumonectomy is considered, careful evaluation of the patient’s physiological reserve and predicted postoperative (ppo) respiratory function is crucial. Patients should also be fully informed of alternative approaches, including those that may carry a higher risk of cancer recurrence
Indications
The primary indication for pneumonectomy is bronchial carcinoma, particularly when:
- The tumor is located at the main stem bronchus, proximal to the bronchus intermedius, or involves the hilar structures.
Other indications for pneumonectomy include:
- Traumatic lung injury with uncontrolled hemorrhage
- Chronic infectious diseases like tuberculosis
- Fungal infections causing significant lung destruction
Types of Pneumonectomy
-
Standard Pneumonectomy
- Most common approach involving the removal of the affected lung.
- Ensures a safe bronchial margin for closure of the bronchial stump.
- Pulmonary artery and veins are ligated without intrapericardial access.
-
Intrapericardial Pneumonectomy
- Required when:
- The right or left main pulmonary artery is involved.
- Tumor proximity to the pulmonary veins necessitates isolation and division at the left atrium to ensure clear vascular margins.
- Close coordination between the surgeon and anesthetist is essential during pulmonary artery clamping to maintain stable cardiac output.
- Required when:
-
Extrapleural Pneumonectomy
- A more radical procedure, typically reserved for mesothelioma.
- Involves excision of:
- Affected lung
- Ipsilateral pleura
- Hemidiaphragm
- Hemipericardium
- Reconstruction with patches may be required.
- Rarely performed after the Mesothelioma and Radical Surgery trial showed worse outcomes compared to medical management.
-
Completion Pneumonectomy
- Refers to excision of remaining lung tissue after prior resection surgery.
-
Carinal Pneumonectomy
- Rarely performed, involving the excision of the lung and carina.
- Typically done for patients with tumors at the distal trachea or carina.
Goals
- Determine suitability for resection with the “3-legged stool” approach:
- Respiratory mechanics
- Gas exchange
- Cardio-respiratory interaction
- Preoperative optimization:
- Smoking cessation
- Pulmonary rehabilitation
- Treatment of lung infections and bronchospasm
- Pristine intraoperative management:
- Thoracic epidural analgesia
- Fluid restriction
- Lung-protective ventilation
- Avoidance of hypothermia
Incision Types: Pros and Cons
| Incision | Pro | Con |
|---|---|---|
| Posterolateral Thoracotomy | Excellent exposure to entire operative hemithorax | Postoperative pain; ± respiration dysfunction (short and long term) |
| Lateral Muscle-Sparing Thoracotomy | Decreased postoperative pain | Increased incidence of wound seromas |
| Anterolateral Thoracotomy | Better access for laparotomy, resuscitation, or contralateral thoracotomy, especially in trauma | Limited access to posterior thorax |
| Axillary Thoracotomy | Decreased pain; adequate access for first rib resection, sympathectomy, apical blebs, or bullae | Limited exposure |
| Sternotomy | Decreased pain; bilateral access | Decreased exposure of left lower lobe and posterior thoracic structures |
| Transsternal Bilateral Thoracotomy (“clamshell”) | Good exposure for bilateral lung transplantation | Postoperative pain and chest wall dysfunction |
| Video-Assisted Thoracoscopic Surgery | Less postoperative pain and respiratory dysfunction | Increased local recurrence of lung cancer |
Preoperative Assessment for Pneumonectomy
Lung Cancer Staging
Lung cancers are categorized into:
- Non-small-cell lung cancer (NSCLC) (85% of cases), further divided into:
- Adenocarcinoma
- Squamous cell carcinoma
- Large-cell carcinoma
- Small-cell lung cancer (SCLC)
Staging of lung cancer follows the eighth edition of the tumour, node, metastasis (TNM) classification. All patients should undergo:
- CT scan
- Positron emission tomography-CT (PET-CT) to evaluate lymph node status.
- If PET-CT positive mediastinal lymph nodes are found, further sampling via endobronchial ultrasound (EBUS) or mediastinoscopy is required.
- Surgery is typically offered to patients with T1-3 N0-1 M0 disease. In select cases, patients with T4 or N2 disease may also undergo radical multimodal treatment after discussion within the multidisciplinary team (MDT).
Suitability for Surgery
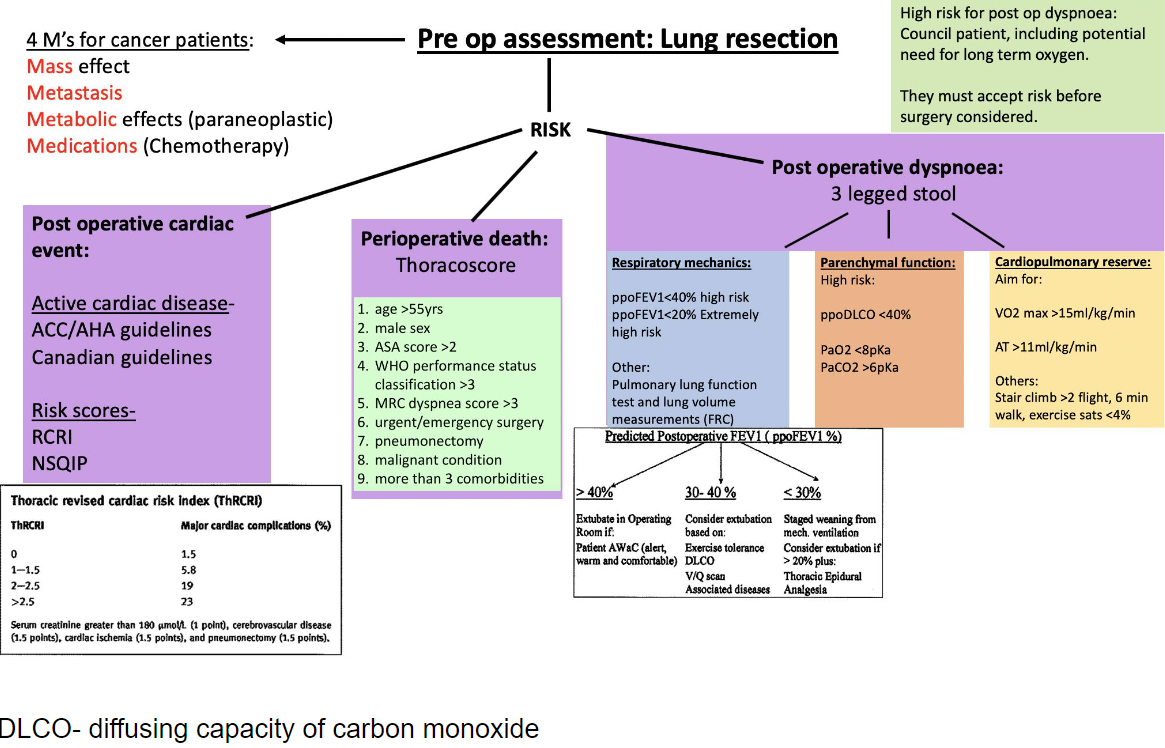
According to the British Thoracic Society (BTS), preoperative risk assessment for lung resection is divided into three domains:
- Operative mortality
- Perioperative myocardial events
- Postoperative dyspnoea
Operative Mortality
- Thoracoscore can estimate postoperative mortality based on nine factors: age, sex, ASA score, performance status, dyspnoea score, surgical priority, extent of surgery, malignancy, and co-morbidity.
- Thoracoscore has limitations, and therefore, more emphasis is placed on evaluating exercise capacity and physiological reserve.
Perioperative Myocardial Events
- Patients with active cardiac conditions (e.g., unstable angina, heart failure, arrhythmias) should consult a cardiologist for medical optimization.
- In patients without active cardiac conditions, use the Revised Cardiac Risk Index (RCRI). If RCRI ≥ 3 or poor functional capacity is noted, refer for exercise stress testing and cardiology review.
- Transthoracic echocardiography (TTE) is recommended for all patients undergoing pneumonectomy, especially for those with unexplained dyspnoea or audible heart murmur. Pulmonary hypertension is a relative contraindication, particularly for right pneumonectomy due to the increase in pulmonary vascular resistance.
Revised Cardiac Risk Index (RCRI)
- Number of Factors and Risk of Major Cardiac Complication:
- 0: 0.4%
- 1: 1%
- 2: 7%
- ≥3: 11%
- Risk Factors:
- High-risk type of surgery (includes all thoracic surgery)
- Ischaemic heart disease
- History of congestive cardiac failure
- History of cerebrovascular disease
- Insulin therapy for diabetes
- Preoperative serum creatinine > 177 μmol/L
Cardiac complications include myocardial infarction, pulmonary oedema, ventricular fibrillation, primary cardiac arrest, and complete heart block.
Thoracic Revised Cardiac Risk Index (ThRCRI)
- ThRCRI and Major Cardiac Complications (%):
- 0: 1.5%
- 1–1.5: 5.8%
- 2–2.5: 19%
- more than 2.5: 23%
- Criteria:
- Serum creatinine > 180 μmol/L (1 point)
- Cerebrovascular disease (1.5 points)
- Cardiac ischemia (1.5 points)
- Pneumonectomy (1.5 points)
Surgical Options:
- Lobectomy or pneumonectomy usually not recommended if <35% or <10 ml/kg/min
- Consider other options if risk is high
(Source: ERS, European Respiratory Society; ESTS, European Society of Thoracic Surgeons)
Postoperative Dyspnoea
Preoperative lung function testing assesses respiratory mechanics and lung parenchymal function:
- Respiratory Mechanics (ppo FEV1): Predicted postoperative forced expiratory volume in 1 second (ppo FEV1) can be calculated using the formula:
- ppo FEV1 = preop FEV1 × (19 – number of segments to be resected) / 19
- Scintigraphy can be used in borderline cases to estimate lung function based on perfusion data
- % ppo FEV1 = preop FEV1 × (100 – % perfusion to lung to be resected) / predicted FEV1
- Lung Parenchymal Function (DLCO): Measures gas transfer effectiveness at the alveolar-capillary unit. A ppo DLCO < 30% predicts increased risk of postoperative complications and should prompt further testing such as cardiopulmonary exercise testing (CPET).
Segment Methods for Predicting Postoperative Pulmonary Function
Ppo is predicted by:
- Calculating the portion of all bronchopulmonary segments (BPS) that will remain after resection.
- Multiplying this portion by the preoperative lung function value.
Segments:
- Total pulmonary segments: 19
- Right lung: 10 segments (3/2/5): 55%
- Left lung: 9 segments (3 upper, 2 lingula, 4 lower): 45%
Calculate Predicted Postoperative FEV1 (ppoFEV1):
- ppoFEV1=Preoperative FEV1×(Number of Remaining Lung Segments/Total Number of Lung Segments)
- ppoFEV1%= (ppoFEV1/Predicted Normal FEV1)×100
- FEV1 in litres
Example
- Preoperative values:
- Preoperative FEV1: 2.5 liters
- Predicted normal FEV1 for the patient (based on age, sex, height): 3.0 L
- Surgery involves resection of the right lower lobe (which contains 5 segments).
- After resection, the remaining lung segments are 14 out of 19.
- Calculate ppoFEV1:
- ppoFEV1 = 2.5 liters × (14 / 19) = 1.84 liters
- Calculate ppoFEV1 as a percentage:
- ppoFEV1% = (1.84 liters / 3.0 liters) × 100 = 61.3%
Risk Categories:
- Low risk: ≥40% ppoFEV1
- Moderate risk: 30% to 40% ppoFEV1
- High risk: <30% ppoFEV1
Functional Assessment of Cardiopulmonary Interaction
- Shuttle Walk Test: Patients walk between two 10 m spaced cones at an increasing pace. A distance >400 m correlates with a peak oxygen consumption (VO2 peak) > 15 mL O₂/kg/min. Patients covering <400 m should be referred for CPET.
- Cardiopulmonary Exercise Testing (CPET): The most critical measure is V_O2 peak:
- VO2 peak >20 mL O₂/kg/min: Suitable for pneumonectomy.
- VO2 peak <10 mL O₂/kg/min: Contraindication for surgery.
Determine Physiological Suitability for Procedure by Assessing Predicted Postpneumonectomy Pulmonary Function
- ppoFEV1 > 40%
- ppoDLCO > 40%
- VO2 max > 15 mL/kg/min (> 4 METS)
- Consider V/Q scanning for all pneumonectomies &/or if ppoFEV1 < 40%
Risk Assessment Summary
The “3-Legged” Stool of Pre-thoracotomy Respiratory Assessment
-
Respiratory Mechanics
- FEV1: Predicted postoperative (ppo) > 40%
- MVV, RV/TLC, FVC
-
Cardio-Pulmonary Reserve
- VO2 max: > 15 ml/kg/min
- Stair climb > 2 flights, 6 min walk, Exercise SpO2 < 4%
-
Lung Parenchyma Function
- DLCO: ppo > 40%
- PaO2 > 60, PaCO2 < 45
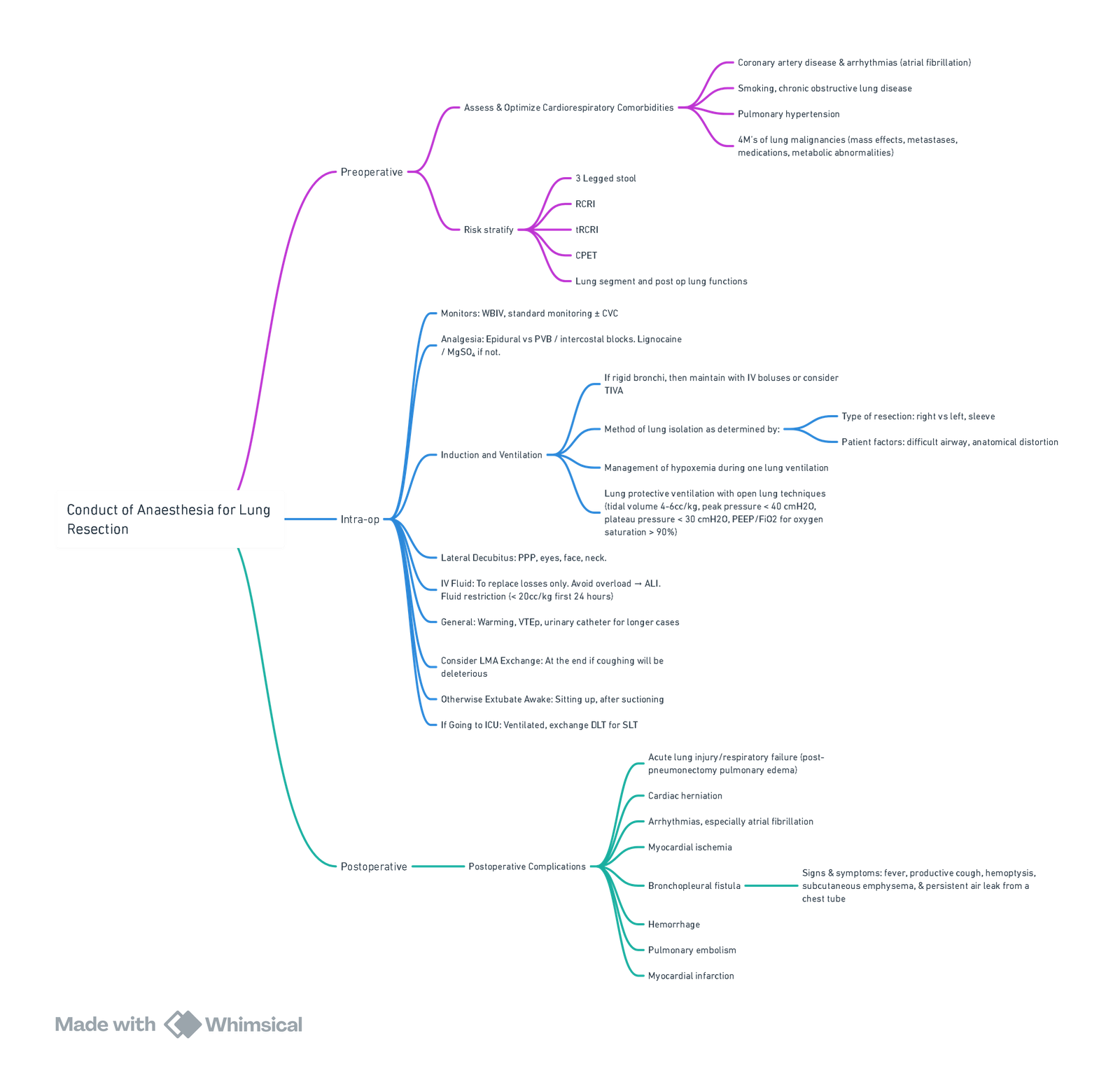
Conduct of Anaesthesia for Lung Resection
Surgical Approach
-
Preoperative Rigid Bronchoscopy:
- Performed after induction of anesthesia to confirm sufficient bronchus length free of tumor, ensuring the feasibility of the procedure.
- Sleeve lobectomy is considered if a portion of the bronchus or pulmonary artery is involved, eliminating the need for pneumonectomy by excising the affected lobe and bronchus/artery with anastomosis of the remaining structures.
-
Common Surgical Approach:
- The most common access is a posterolateral thoracotomy at the fifth intercostal space, sometimes requiring excision of the fifth rib for exposure.
- Alternatively, video-assisted thoracoscopic surgery (VATS) can be used.
- The chest is explored for pleural effusions and metastatic deposits on the pleura or diaphragm before continuing.
- Once confirmed, the lung is retracted, and the superior and inferior pulmonary veins and pulmonary artery are sequentially ligated and divided.
- The bronchus is stapled and cut, with the patency tested by filling the thorax with warm saline and performing a leak test.
- A thoracostomy tube is placed in the postpneumonectomy space.
Anaesthesia
-
Induction:
- Confirm availability of an ICU bed and crossmatch two units of blood.
- Postoperative analgesia options include midthoracic epidural or paravertebral catheter.
- Invasive arterial pressure monitoring and central venous catheterisation are recommended for fluid and vasopressor management.
- Temperature probes and urinary catheter should be placed.
- Antibiotics are administered per local guidelines.
- Anesthesia maintenance may use a volatile agent or total intravenous anesthesia (TIVA), especially during rigid bronchoscopy.
-
Position:
- The patient is positioned in lateral decubitus with careful attention to eye protection, pressure points, and neck alignment.
- Venous thromboembolism (VTE) prophylaxis is provided using graduated compression stockings, and normothermia is maintained with a warming blanket and fluid warmer.
-
Lung Isolation:
- The operative lung is collapsed, typically with a double lumen tube (DLT), or alternatively a bronchial blocker if DLT placement is difficult.
- Fibreoptic bronchoscopy is used to confirm positioning, with particular attention to the right upper lobe in right-sided DLTs.
- One-lung ventilation (OLV) should begin before thoracotomy. Lung-protective strategies during OLV include low tidal volumes and sufficient PEEP.
- Suggested OLV ventilatory targets:
- Tidal volume: 5–6 mL/kg (ideal body weight)
- Peak airway pressure: <35 cm H₂O
- Plateau airway pressure: <25 cm H₂O
- PEEP: 5 cm H₂O
- Maintain oxygen saturation at 94–98% (avoid hyperoxia)
Haemodynamic Management
- Clamping of the pulmonary artery causes the entire pulmonary circulation to divert through the remaining lung. Fluid management is crucial to avoid both hypovolemia and excessive fluid, which increases the risk of post-pneumonectomy pulmonary oedema (PPO). Fluid restriction targets include:
- Positive fluid balance within 24 hours not exceeding 20 mL/kg
- Urine output ≥0.5 mL/kg/h should be accepted
- Intraoperative fluid restricted to the previous hour’s urine output plus 20 mL/h
- Hypotension due to epidural should be treated with vasoactive drugs, not fluids.
Pulmonary Artery Clamping Test
- Final test for suitability for pneumonectomy is clamping of the ipsilateral pulmonary artery.
- Significant cardiovascular collapse or elevated central venous pressure (CVP) indicates right ventricular failure and a high risk of postoperative cardiac complications.
- If physiological deterioration occurs and other causes (e.g., surgical compression) are excluded, the surgical team must reconsider continuing the procedure.
Postoperative Care
- Extubation:
- The patient should be extubated awake, warm, and comfortable before transfer to a postoperative care unit.
- Pain Management and Monitoring:
- Adequate analgesia (epidural/paravertebral) is essential for effective coughing and secretion clearance.
- Invasive monitoring for blood pressure allows for titration of vasoconstrictors.
- Early detection and treatment of complications such as haemorrhage, PPO, and cardiac arrhythmias are crucial.
- Chest Drain Management:
- The drain is clamped at the end of surgery and opened briefly every hour to check for bleeding.
- Prolonged drain opening can cause mediastinal shift and cardiovascular instability.
- The drain is usually removed on postoperative day 1, allowing the hemithorax to accumulate serous fluid.
- Ward Transfer and Recovery:
- Uncomplicated patients typically step down to a thoracic surgical ward by day 2 and are discharged within 7–10 days.
- Physiotherapy and incentive spirometry help reduce postoperative pulmonary complications.
View or edit this diagram in Whimsical.
Links
- One lung Ventilation and VATS
- Double lumen and Bronchial blocker
- Hypoxia Pulmonary Vasoconstriction (HPV)
- Respiratory physiology and Thoracic anaesthesia
- Thoracic pre-op assessment
- Anaesthesia and cancer surgery
References:
1. Hackett, S. F., Jones, R., & Kapila, R. (2019). Anaesthesia for pneumonectomy. BJA Education, 19(9), 297-304. https://doi.org/10.1016/j.bjae.2019.04.004
2. Lederman D, Easwar J, Feldman J, Shapiro V. Anesthetic considerations for lung resection: preoperative assessment, intraoperative challenges and postoperative analgesia. Ann Transl Med. 2019 Aug;7(15):356. doi: 10.21037/atm.2019.03.67. PMID: 31516902; PMCID: PMC6712248.
3. Anaesthesia considerations for lung resection. Wits refresher 2018 Hlongwane
Summaries:
Pulmonary end arterectomy-video
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “4efd3226-03e4-42b8-ad49-70a357d68efd”



