{}
Definition
- Hypoxic pulmonary vasoconstriction (HPV) is a reflex contraction of vascular smooth muscle in the pulmonary circulation in response to a low regional partial pressure of oxygen (PO₂).
- Low alveolar PO₂ results in smooth-muscle-mediated vasoconstriction by an unknown but direct mechanism, shunting blood away from the hypoxic area.
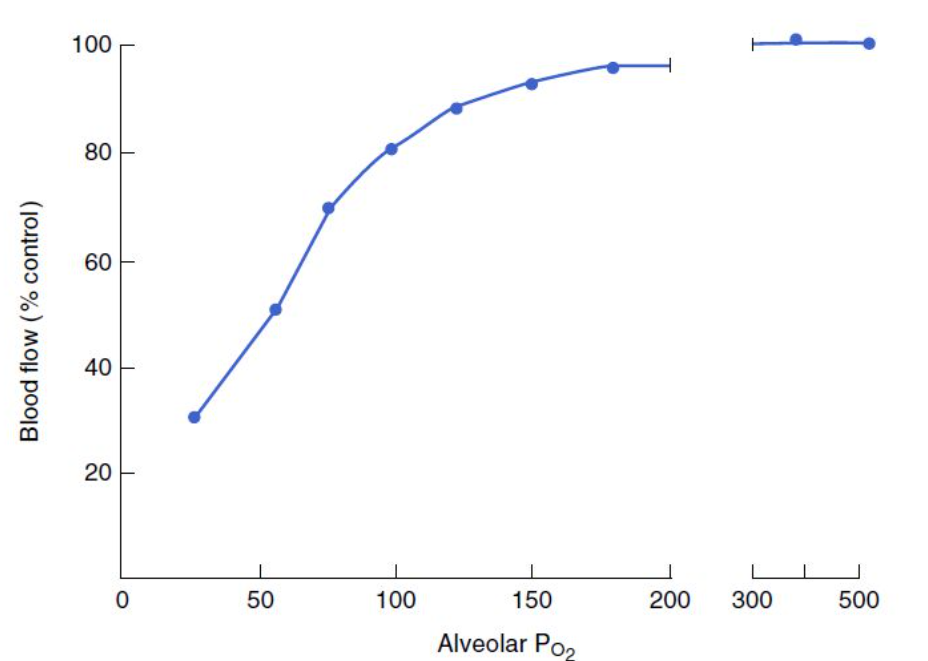
- The response is non-linear: a PAO₂ drop below 70 mmHg results in a dramatic drop in blood flow.
- Occurs naturally at high altitudes, causing pulmonary hypertension.
- Reversal of HPV at birth allows circulation to transition from fetal to neonatal physiology.
Physiology
- The systemic circulation dilates in the presence of hypoxia, contrasting with the pulmonary circulation, which vasoconstricts.
- This response, known as hypoxic pulmonary vasoconstriction, is a protective physiological reflex aiming to divert blood flow away from hypoxic areas of the lungs to areas with better ventilation and oxygenation.
V/Q Matching
- In an ideal lung model, ventilation and perfusion would be identically distributed, achieving perfect matching.
- In vivo, both ventilation and perfusion increase from non-dependent to dependent areas, with perfusion increasing more. This results in varying V/Q ratios throughout different lung regions (e.g., in the upright posture, there is more perfusion and less ventilation at the bases, i.e., low V/Q ratios; and more ventilation with less perfusion at the apices, i.e., high V/Q ratios).
- HPV aims to improve V/Q matching, though its role is minimal in normal, healthy lungs with already well-matched ventilation and perfusion.
- HPV plays a significant role in chronic respiratory diseases like chronic obstructive pulmonary disease (COPD) and interstitial lung disease. In these conditions, maintaining normal gas exchange relies on optimizing V/Q matching influenced by HPV.
- In chronic respiratory diseases, the local regional response of HPV aids long-term adequate oxygenation. Inappropriate supplemental oxygen delivery and some drugs can attenuate HPV, worsen V/Q matching, and deteriorate oxygenation. Chronic high-resistance exposure in the pulmonary circulation contributes to irreversible pulmonary hypertension, right ventricular hypertrophy, and cor pulmonale.
- HPV also plays a role in acute respiratory pathology, such as acute asthma, pneumonia, pulmonary embolism, and pulmonary edema. HPV benefits these settings by redirecting blood flow to better-ventilated lung areas, improving V/Q matching.
Mechanism of HPV Optimization of V/Q Mismatch
- The pulmonary circulation’s low-resistance, low-pressure system means that HPV, by causing localized high resistance to blood flow, promotes diversion of flow to areas of lower resistance. This leads to passive distension and recruitment of pulmonary capillaries, increasing perfusion.
Mechanism and Phases
- HPV in humans has two distinct temporal phases:
- Phase 1 begins within a few seconds and is maximal at 15 minutes, likely mediated by potassium channels.
- Phase 2 begins when moderate hypoxia is sustained for more than 30-60 minutes, with a further increase in pulmonary vascular resistance peaking at 2 hours, likely due to increased endothelin release.
- When normoxia returns, pulmonary vascular resistance takes several hours to return to baseline.
Mediators Produced by Pulmonary Endothelial Cells and Their Mechanisms for Modulating HPV
| Mediator | Mechanism |
|---|---|
| Nitric oxide | Reduces intracellular calcium, relaxing smooth muscle. Hypoxia reduces basal nitric oxide production, enhancing HPV. |
| Prostacyclin | Stimulates cyclic adenylate cyclase, increasing cyclic AMP production, leading to vasodilation. |
| Endothelin-1 | Acts via G-protein receptors on PASMCs, causing potent vasoconstriction. |
Effects of Different Inotropes on HPV
- Catecholamines with β effects (Adr, Dop, Dob) inhibit HPV at standard doses. Dobutamine can be used to augment RV function but may cause hypotension from decreased SVR.
- Vasopressors with α effects (Norad, PEP) enhance HPV.
- Vasopressin increases SVR but decreases PVR, useful in pulmonary hypertension crisis.
- Milrinone dilates pulmonary vasculature and augments myocardial contractility.
Effects of General Anaesthesia on HPV
- No or minimal effect on HPV: Ether, Thiopental, Halothane, Fentanyl, Propofol, Desflurane, Isoflurane, Sevoflurane.
- Direct inhibitors: Nitroglycerin, nitroprusside, infection, hypocarbia, alkalemia.
- Indirect inhibitors (increase PA pressures, overcoming vasoconstriction): Vasopressors, volume overload, mitral stenosis, thromboembolism.
- Acidosis improves HPV, but the clinical significance is minimal as it is accompanied by an overall increase in PVR.
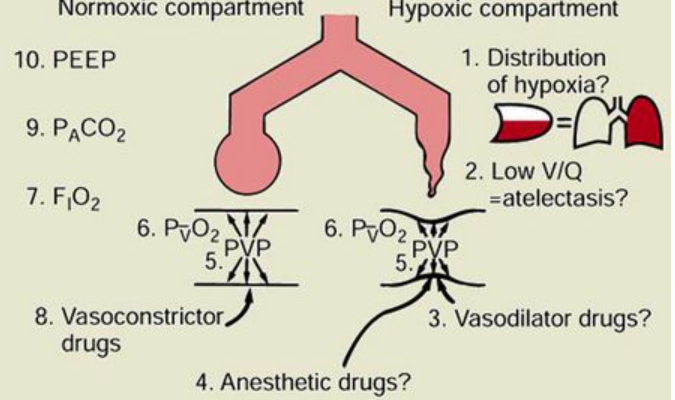
Impact of Various Factors on Normoxic and Hypoxic Compartments
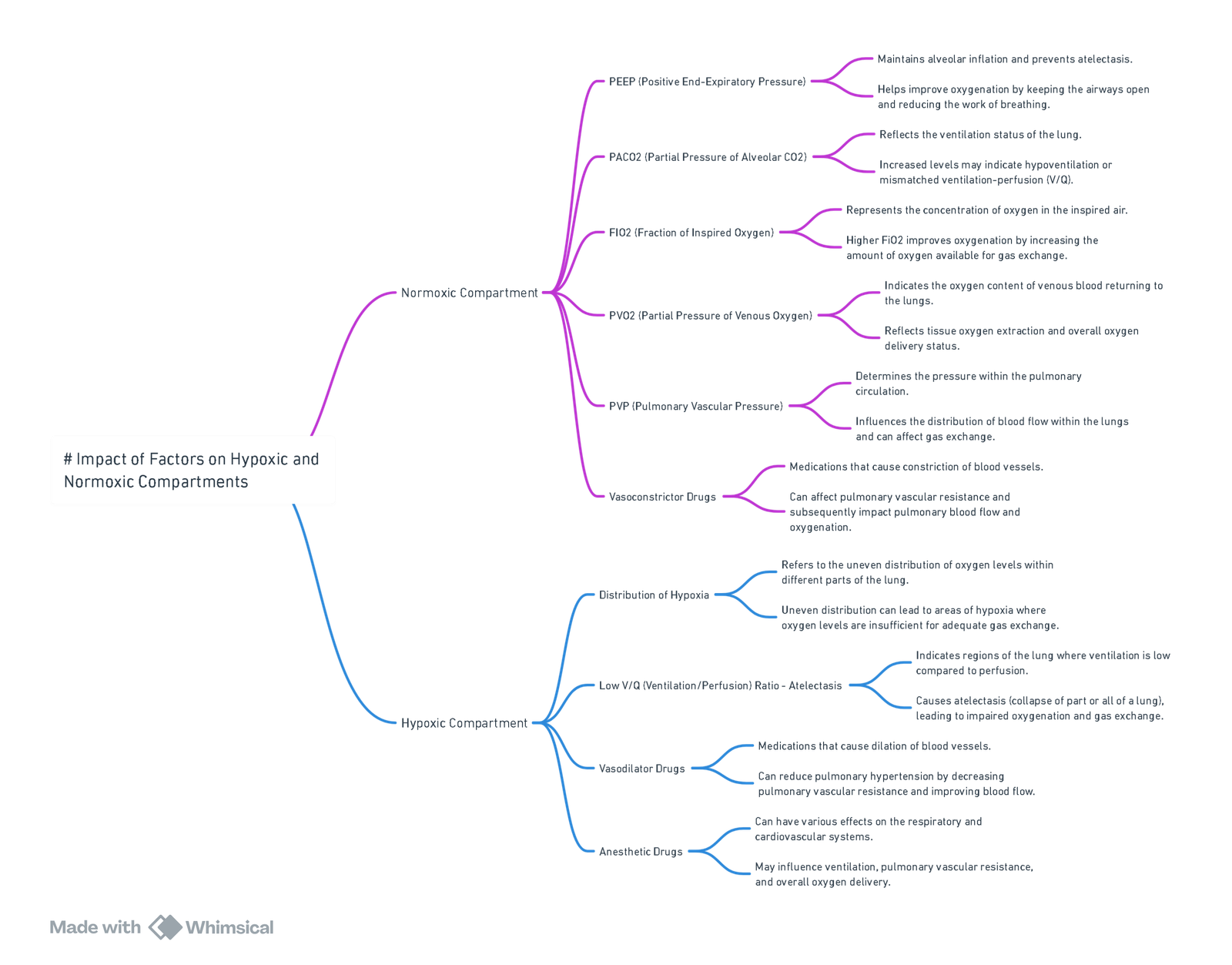
View or edit this diagram in Whimsical.
Links
- Respiratory physiology and Thoracic anaesthesia
- One lung Ventilation and VATS
- Pulmonary Hypertension
- Long volume reduction surgery
References:
- Tarry, D. and Powell, M. L. (2017). Hypoxic pulmonary vasoconstriction. BJA Education, 17(6), 208-213. https://doi.org/10.1093/bjaed/mkw076
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “abaed5ca-3902-4d2a-a232-232b49246f18”



