{}
Exercise Testing and Optimization
Introduction
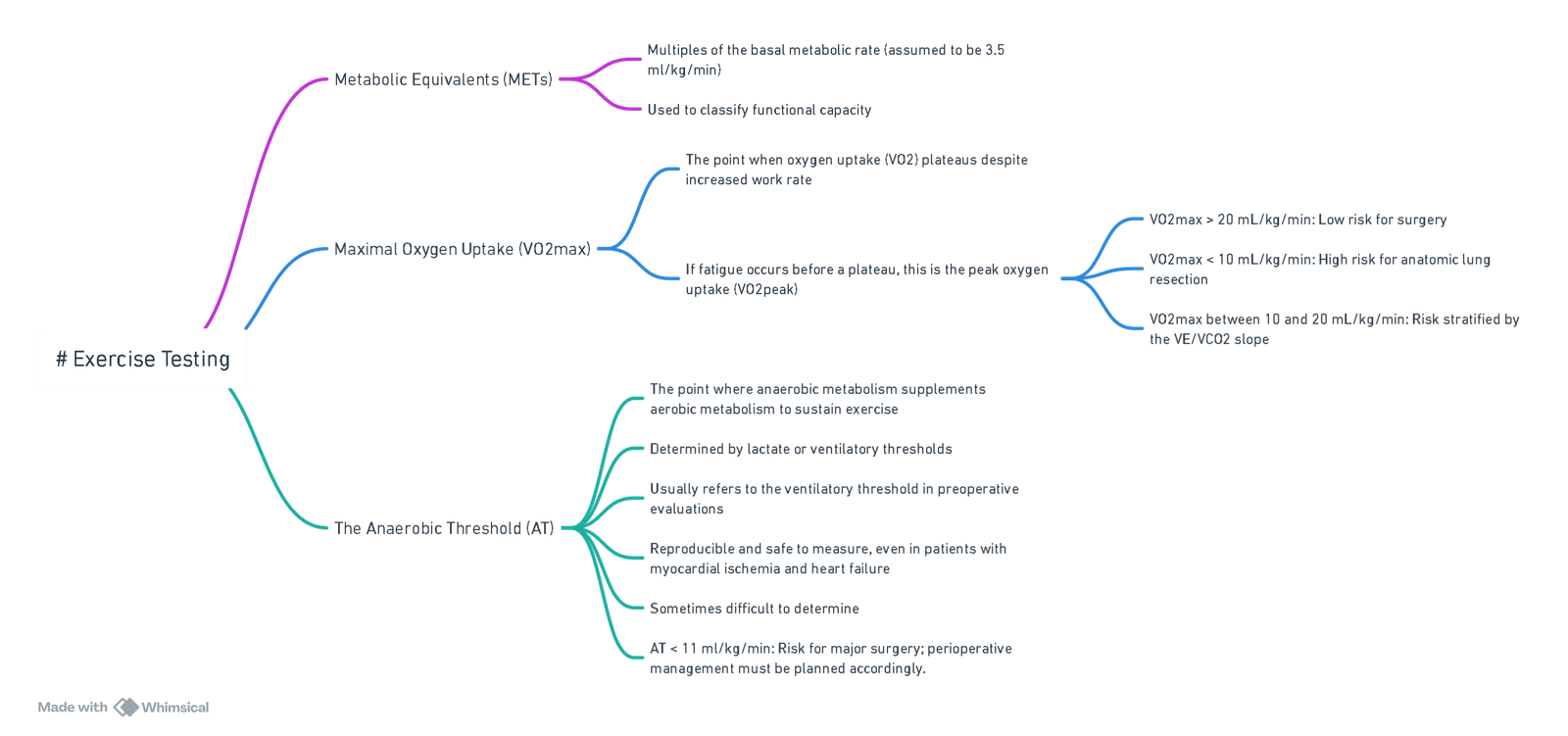
View or edit this diagram in Whimsical.
Differences Between Oxygen-Independent and Oxygen-Dependent Metabolism During Exercise
- Duration of Exercise Test:
- Test duration of at least 10 minutes is recommended for assessing aerobic capacity, similar to anaerobic threshold testing.
- Initial metabolism at the onset of exercise is predominantly anaerobic; oxidative phosphorylation dominates after about 2 minutes.
- Time to oxidative phosphorylation is prolonged in conditions like heart failure, COPD, peripheral vascular disease, and diabetes.
- Relationship Between VO2peak and Anaerobic Threshold:
- Central (cardiorespiratory) and peripheral (musculoskeletal) factors influence the relationship.
- Diseases like ischemic heart disease and heart failure affect this relationship.
- The anaerobic threshold can vary from 50% to 100% of VO2peak.
- Performance during exercise depends partly on mechanical efficiency; perioperative survival depends on cardiorespiratory capacity, not musculoskeletal function, although frailty is a strong predictor of perioperative morbidity and mortality.
- Patients with Acceptable Aerobic Capacity but Poor Functional Group:
- Due to musculoskeletal factors associated with frailty.
- Unlikely to die of cardiovascular failure in the perioperative period but at increased risk of postoperative complications.
- AT testing minimizes peripheral factors’ contribution to poor exercise performance by limiting weight-bearing with cycling.
Assessment of Functional Capacity for Surgical Patients
- Importance:
- Major surgery triggers a stress response lasting up to 72 hours, increasing oxygen consumption to about 5 ml/kg/min, sometimes up to 7 ml/kg/min.
- Preoperative functional capacity assessment determines the ability to survive this increased metabolic demand.
- In patients over 60 undergoing major abdominal surgery, an AT < 11 ml/kg/min during CPET predicts perioperative cardiovascular mortality.
- Myocardial Ischemia and Poor Functional Capacity:
- Significantly increases adverse perioperative cardiac events.
- Functional status is integral to the American College of Cardiology / American Heart Association preoperative cardiac evaluation algorithm.
- Risk stratification is based on whether a patient can complete 4 METS of exercise.
- The risk of myocardial infarction and cardiac arrest increases nearly threefold between functionally independent and dependent patients.
Clinical Assessment of Functional Capacity
- Common Assessments:
- Stair climbing, Duke Activity Status Index (DASI), six-minute shuttle walk test, and cardiopulmonary exercise testing (CPET).
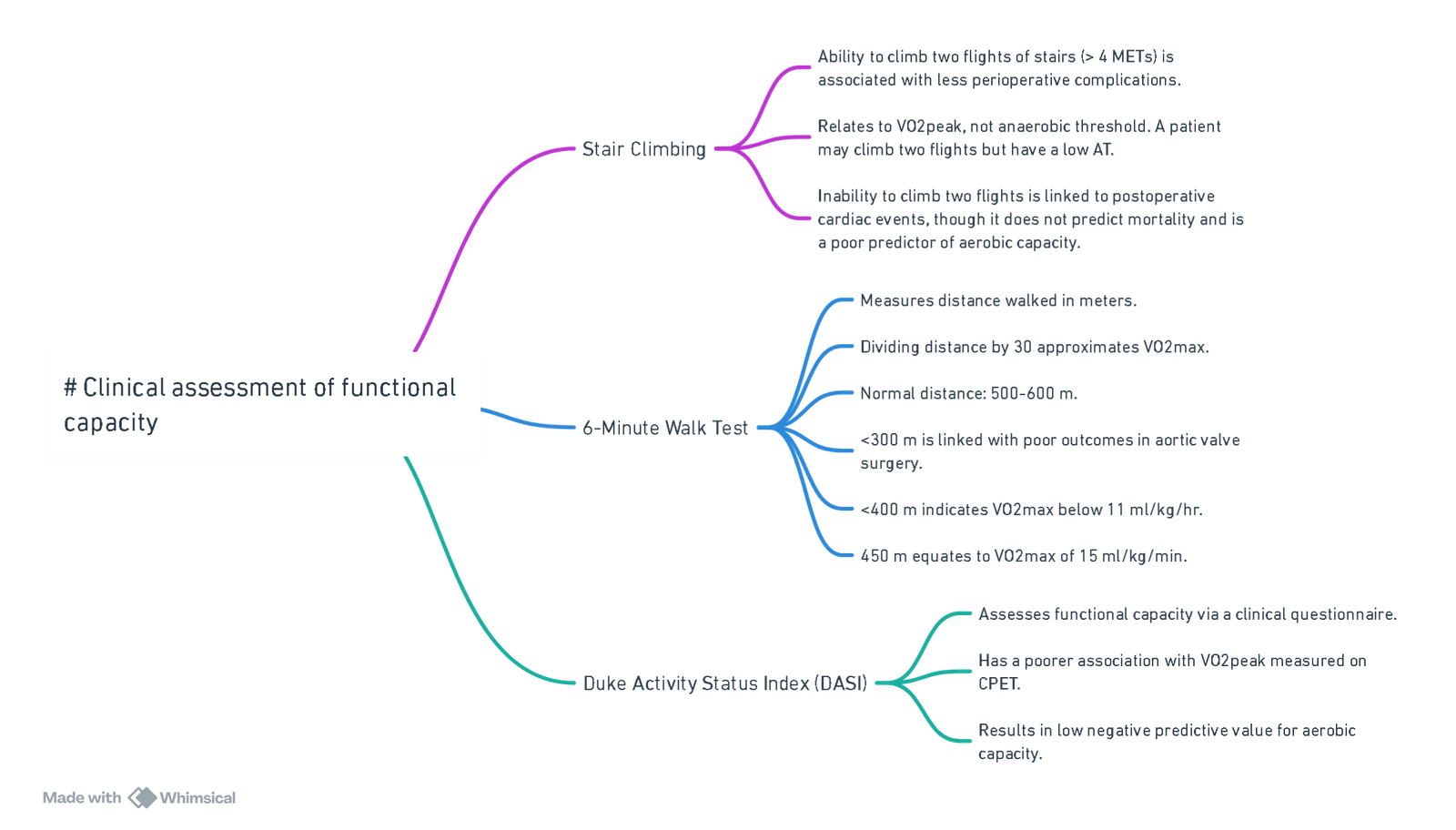
View or edit this diagram in Whimsical.+_
| Criteria for adequate functional capacity |
|---|
| Anaerobic threshold > 11 ml/kg/min and VO2peak > 15 ml/kg/min |
| DASI > 46 |
| Shuttle walk > 360 m |
- Despite limitations, the VO2peak can be estimated where CPET is unavailable:
- VO2peak (ml/kg/min) = 13.43 + 0.02 x shuttle walk test distance (m)
- VO2peak (ml/kg/min) = 11.82 + 0.23 x Duke Activity Status Index (DASI)
Cardiopulmonary Exercise Testing (CPET)
Indications for CPET
| Recommendations | Class | Level of Evidence |
|---|---|---|
| Recommended: For patients with ≥3 cardiac risk factors undergoing high-risk surgery | I | C |
| May be considered: | ||
| For patients with ≤2 cardiac risk factors undergoing high-risk surgery | IIb | B |
| For patients undergoing intermediate-risk surgery | IIb | C |
| Not recommended: Scheduled low-risk surgery | III | C |
Contraindications to CPET
| Contraindications to CPET | Conditions |
|---|---|
| Absolute | Cardiac: |
| Acute MI (3-5 days) | |
| Unstable angina | |
| Active endocarditis | |
| Acute myocarditis or pericarditis | |
| Uncontrolled heart failure | |
| Uncontrolled arrhythmias (symptomatic or CVS compromise) | |
| Syncope | |
| Vascular: | |
| Suspected dissection or leaking AAA | |
| Respiratory: | |
| Uncontrolled asthma | |
| Sats <85% (RA) at rest | |
| Other: | |
| Unable to cooperate | |
| Conditions aggravated by exercise or may impact exercise performance | |
| Relative | Embolic: |
| Thrombosis of lower extremities | |
| Acute PE | |
| Cardiac: | |
| Left main coronary stenosis | |
| Severe stenotic heart lesion (asymptomatic) | |
| Hypertrophic cardiomyopathy | |
| Pulmonary arterial hypertension | |
| Vascular: | |
| Untreated severe hypertension | |
| AAA >8 cm | |
| Arrhythmia: | |
| Tachy or bradyarrhythmia | |
| High degree AV block | |
| Other: | |
| Advanced or complicated pregnancy | |
| Electrolyte abnormalities | |
| Orthopaedic impairment that compromises exercise performance |
Conducting CPET
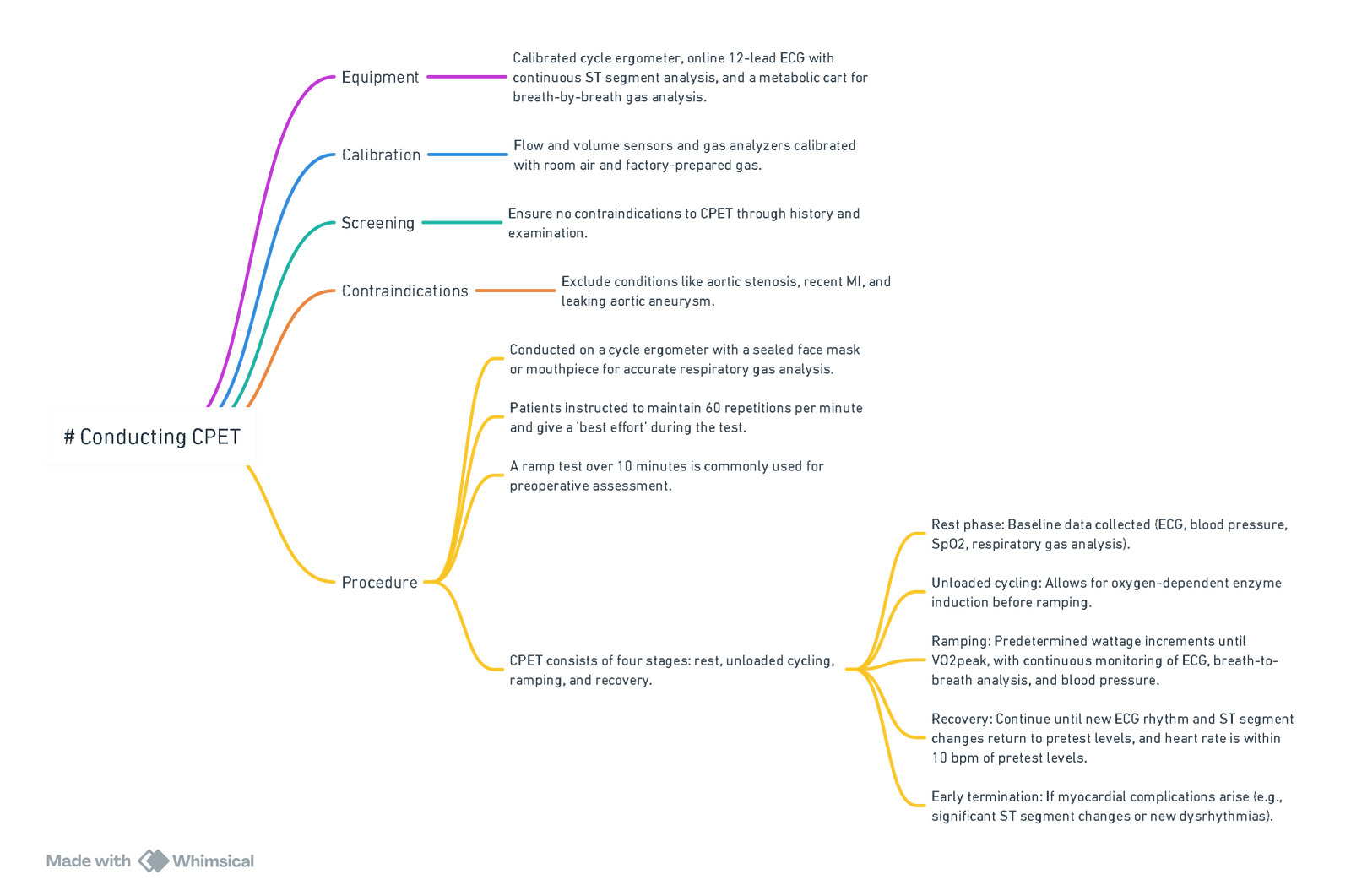
View or edit this diagram in Whimsical.
-
Calculation for Predicted Oxygen Consumption:
Definition Calculation Unloaded VO2 VO2 unloaded (ml/min) = 150 + (6 x weight (kg)) Peak VO2 (female) Peak VO2 (ml/min) = height (cm)–age (years) x 14 Peak VO2 (male) Peak VO2 (ml/min) = height (cm)–age (years) x 20 Increment in work rate per min (Watts/min) = (Peak VO2–Unloaded VO2) / 100
Interpretation of CPET Results
- Anaerobic Threshold (AT):
- Determined using the modified V-Slope method, confirmed by changes in variables like the respiratory exchange ratio, ventilatory efficiency, and end-tidal oxygen values.
- V-slope method: Slope of VCO2-VO2 graph exceeds 1 due to increased glycolytic and lactate production.
- Alternative methods may be used if AT determination is difficult.
Determination of the Anaerobic Threshold
- Combination of indicators:
- Rising ventilatory efficiency for oxygen despite a plateau for carbon dioxide.
- Respiratory Exchange Ratio > 1.
- Increase in end-tidal oxygen preceding a fall in end-tidal carbon dioxide.
- VCO2 crossing over VO2 on the same axis.
- Increase in VCO2-VO2 gradient above 1.
Prognostic Capacity of CPET
- Low AT: Indicates inability to sustain metabolic energy requirements post-major noncardiac surgery.
- Systematic review findings:
- VO2peak and AT associated with survival following hepatic transplant and resection, AAA repair, and intra-abdominal surgery.
- Definitions of prognostic VO2peak and AT thresholds vary.
- Inability to determine AT during CPET is a poor prognostic sign.
Perioperative Management Based on CPET Results
- AT < 10-11 ml/kg/min: Clinically significant.
- Early myocardial ischemia: Positive result requiring further coronary investigation.
- CPET results interpretation: No standardized guidelines, but proposed perioperative management strategies exist.
| CPET Result | Perioperative Management for Major Noncardiac Surgery |
|---|---|
| Early myocardial ischemia | Preoperative coronary angiography |
| Adequate AT, without myocardial ischemia | Preoperative statin therapy |
| Adequate AT with late inducible myocardial ischemia | Preoperative statin therapy and beta-blockade |
| Poor AT without myocardial ischemia | Preoperative goal-directed therapy |
| Poor AT with late inducible myocardial ischemia, or unable to reach AT | Consider deferring surgery, offering lesser procedure, or non-surgical management |
Optimization
Cardiac for non-cardiac surgery
Preoperative Optimization (General)
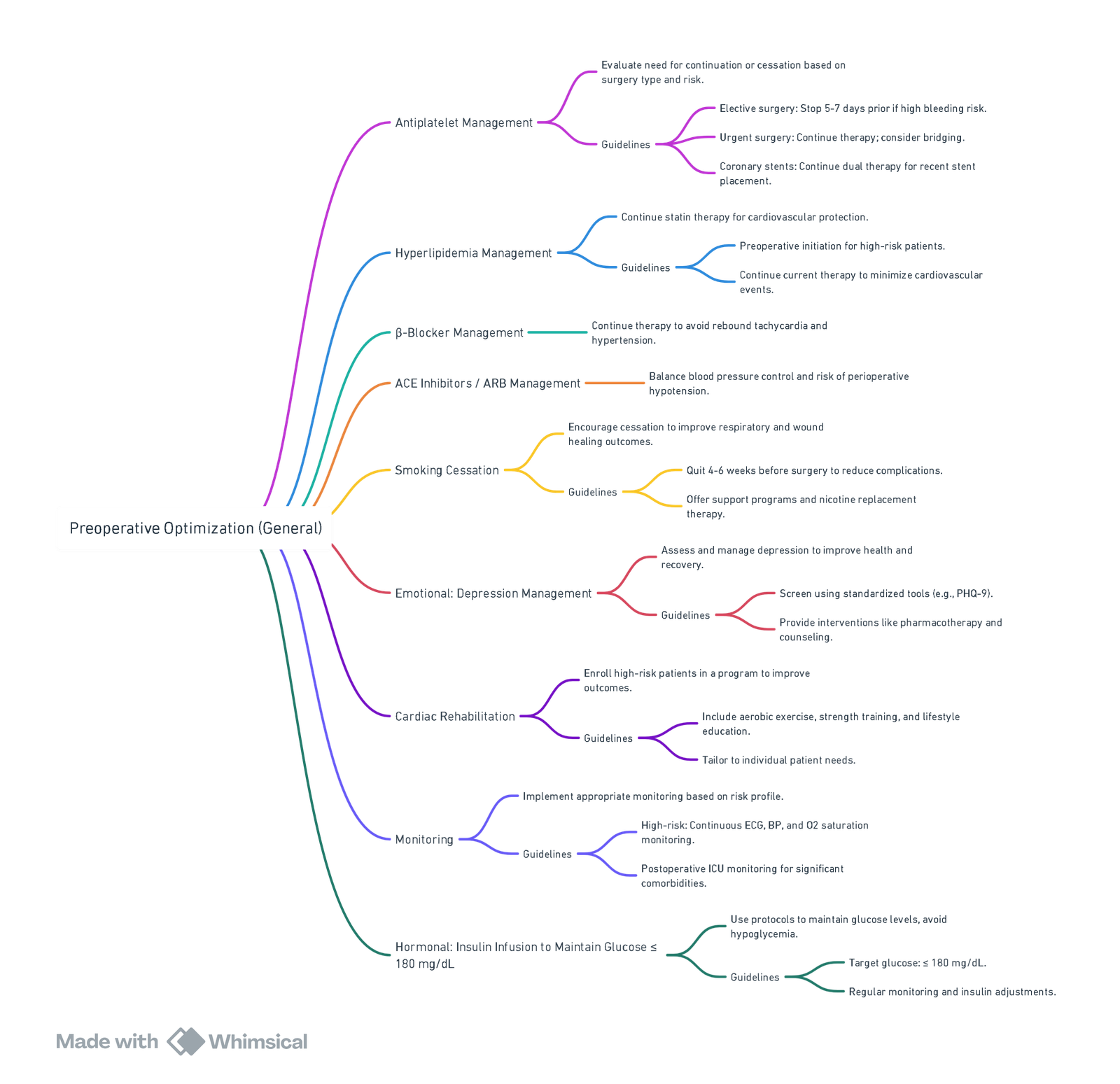
View or edit this diagram in Whimsical.
Multi-Modal Pre-habilitation Program
Exercise & Physical Activity
Goals
- Targeted and Individualized Exercise Program:
- Prescribe a personalized exercise regimen encompassing cardiovascular, resistance, flexibility, and balance training.
- Daily Physical Activity:
- Encourage at least 30 minutes of physical activity per day.
- Reduce Sedentary Time:
- Decrease the amount of time spent sitting or engaging in sedentary activities.
- Long-Term Behavior Change:
- Promote a more active lifestyle over the long term.
Nutritional Optimization
Goals
- Understanding Dietary Habits:
- Gain insights into the patient’s eating patterns and identify areas of deficiency.
- Nutritional Feedback:
- Provide advice on how to optimize the patient’s nutrition.
- Identifying Malnutrition:
- Detect patients who are malnourished.
- Nutritional Supplementation:
- Offer nutritional supplements to patients with identified deficiencies.
Psychological Wellbeing
Goals
- Identify Psychological Needs:
- Recognize patients who need psychological interventions using tools such as the SF-36 and HADS.
- Anxiety Reduction Techniques:
- Provide anxiety-reducing strategies tailored to individual patient preferences.
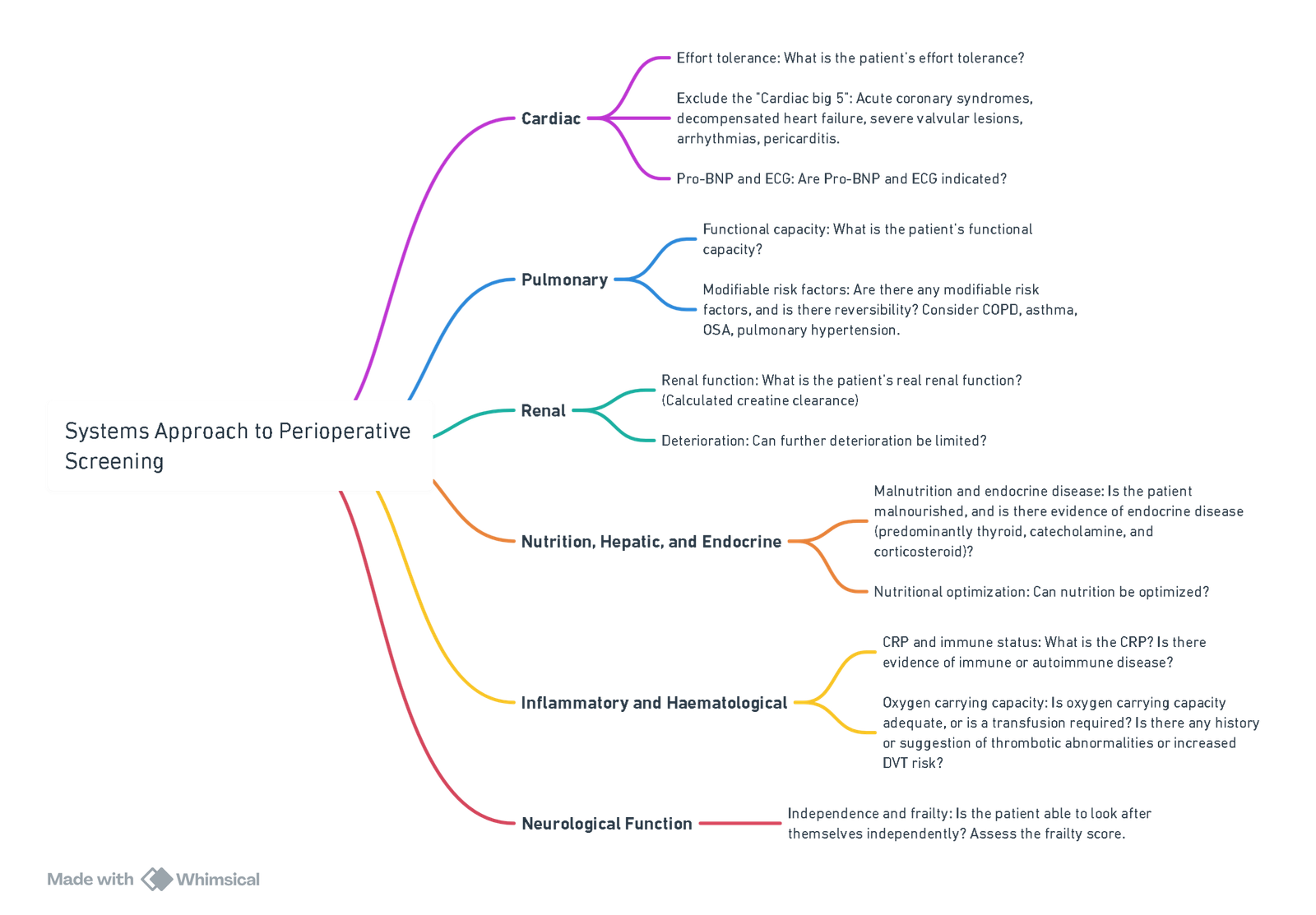
Systems Approach to Perioperative Screening
Preoperative Cardiac Algorithm Incorporating NT-ProBNP
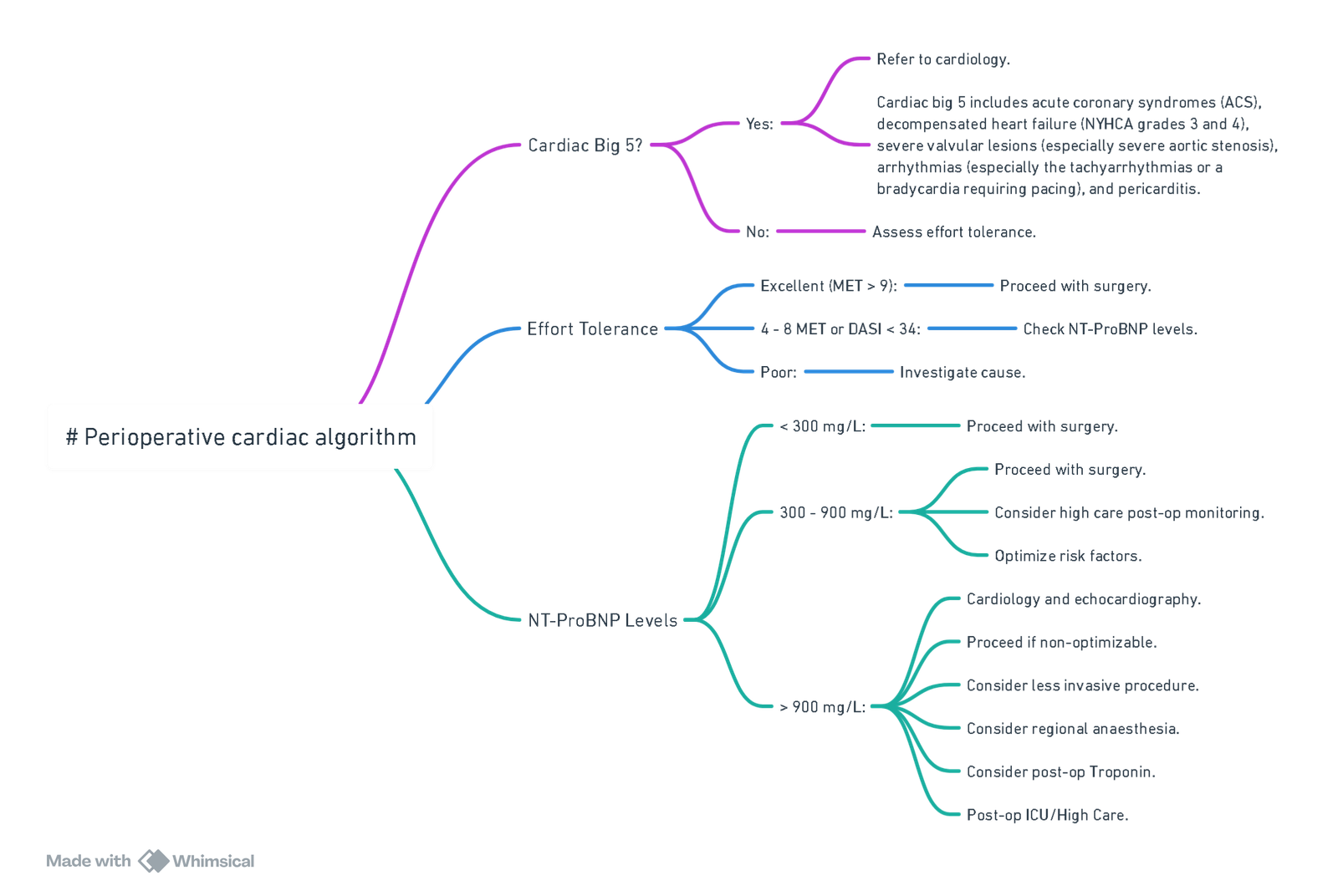
View or edit this diagram in Whimsical.
Links
References:
- Lee, L. K. K., Tsai, P. N., Ip, K. Y., & Irwin, M. G. (2019). Pre‐operative cardiac optimisation: a directed review. Anaesthesia, 74(S1), 67-79. https://doi.org/10.1111/anae.14511
- Cardiopulmonary Exercise Testing. University of Cape Town refresher 2016. Prof B. Biccard
- Alphonsus, C S et al. South African cardiovascular risk stratification guideline for non-cardiac surgery. South African Medical Journal, [S.l.], v. 111, n. 10b, oct. 2021. ISSN 2078-5135. Available at: <http://www.samj.org.za/index.php/samj/article/view/13424/9975>.
- A practical approach to perioperative risk optimisation for non-cardiac surgery. I Cassimjee University of the Witwatersrandhttps://orcid.org/0000-0001-7074-9752
- Bhave, N. M., Cibotti-Sun, M., & Moore, M. M. (2024). 2024 perioperative cardiovascular management for noncardiac surgery guideline-at-a-glance. Journal of the American College of Cardiology. https://doi.org/10.1016/j.jacc.2024.08.018
Summaries:
CPET;
Pre-op cardiac assessment
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “1b7c797e-9908-4dc8-a900-ba196ed18725”



