{}
Summary
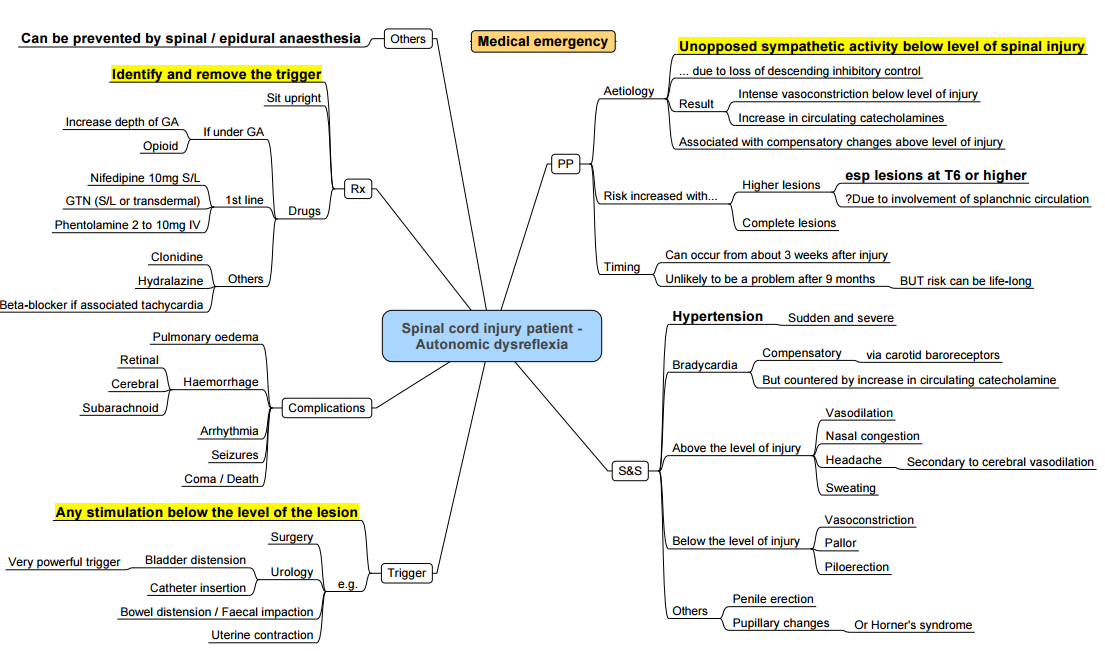
Autonomic Dysreflexia (AD)
- Definition: A condition associated with spinal cord injury (SCI) typically at T6 or above.
- Risk Factors: Higher level SCI and complete lesions.
- Most commonly presents between 3-6 months after injury
- Frequency variable: 20-70% of patients
- Above lesion: reflex bradycardia & vasodilation (flushed)
- Below lesion: unopposed sympathetic stimulation (vasoconstriction/hypertension)
Mechanism
- Noxious stimuli activate pain fibers, sending an afferent impulse to the spinal cord.
- This triggers a generalized sympathetic response.
- Resulting in an increase in blood pressure.
- Above the level of injury:
- Carotid baroreceptors sense the increased blood pressure.
- Vagus nerve-mediated parasympathetic response increases.
- Dysregulated parasympathetic response occurs only above the SCI.
- Below the level of injury:
- SCI blocks descending inhibitory signals to preganglionic sympathetic neurons.
- Leads to an increased sympathetic response.
- Causes splanchnic vasoconstriction.
Clinical Manifestations
- Bradycardia
- Sweating
- Bilateral headache
- Flushing
- Nasal congestion
- Splanchnic vasoconstriction
- Pallor
- Piloerection
- Cold extremities
Consequences
- Arrhythmia
- Intracranial pressure increases
- Pulmonary edema
- Renal insufficiency
- Seizures
- Stroke
- Death
Note
- The unregulated sympathetic tone leads to sustained increasing blood pressure.
- Autonomic dysreflexia occurs with lesions at or above T6 because of the loss of sympathetic control of splanchnic circulation, resulting in a critical mass of blood vessels causing elevated blood pressure.
Considerations
- Potential for hypertensive emergency with end-organ damage
- Considerations of chronic SCI
- Need for invasive monitoring
- Difficult to assess success of neuraxial technique
Management
- Discussion with surgeon regarding plan for procedure
- Remove potential triggers: full bladder, Foley insertion, full rectum, surgical stimulus
- General anesthetic vs neuraxial technique (if GA, consider a deep anesthetic)
Management of Hypertensive Event
- Consider deepening level of anesthesia if under GA
- If epidural, consider top-up
Treat Severe Hypertension with Fast-acting Titratable Agents
- Nitroprusside 0.5-3 mcg/kg/min or nitroglycerin 5-200 mcg/min
- Hydralazine 10-20 mg IV prn
- Phentolamine 5 mg IV prn
- Look for evidence of end-organ involvement & treat accordingly
Pregnancy Considerations
- Multidisciplinary discussion regarding plan for labor & delivery
- Consider scheduled elective cesarean section
If Vaginal Delivery
- Admit early to monitored bed with telemetry
- Need continuous BP monitoring with arterial line
- Remove all preventable triggers of autonomic hyperreflexia (vaginal exams, full bladder = Foley insertion)
- Start early epidural to prevent hypertensive episodes from contractions
Difficult to Assess Success of Epidural
- May need larger test dose to rule out subarachnoid placement
Two Ways to Assess Level of Epidural
- Sensory block cephalad to level of spinal cord lesion
- Evaluating segmental reflexes below level of the lesion: lightly stroke each side of the abdomen above & below the umbilicus, looking for contraction of the abdominal muscles & deviation of the umbilicus toward the stimulus (reflexes are absent below the level of the block)
If Cesarean Delivery
- Either general anesthetic or neuraxial technique:
- Must have arterial line
- Vasodilators drawn up & ready
- Succinylcholine contraindicated
- Severe respiratory insufficiency or technical difficulties with neuraxial anesthesia may necessitate the use of general anesthesia
Links
References:
- The Calgary Guide to Understanding Disease. (2024). Retrieved June 5, 2024, from https://calgaryguide.ucalgary.ca/
- Krassioukov, A. V., Warburton, D. E. R., Teasell, R., & Eng, J. J. (2009). A systematic review of the management of autonomic dysreflexia after spinal cord injury. Archives of Physical Medicine and Rehabilitation, 90(4), 682-695. https://doi.org/10.1016/j.apmr.2008.10.017
- Anesthesia Considerations. (2024). Retrieved June 5, 2024, from https://www.anesthesiaconsiderations.com/
Summaries:
Copyright
© 2025 Francois Uys. All Rights Reserved.
id: “ec9cd4de-7119-4895-a508-7d43ce401980”



